
HIT Risk Assessment Calculator
HIT Risk Assessment Tool
This tool calculates the 4Ts score, a clinical tool used to assess the probability of Heparin-Induced Thrombocytopenia (HIT). Remember: this is for educational purposes only and not a substitute for professional medical diagnosis.
Most people assume blood thinners like heparin are safe because they’re used so often - in hospitals, after surgery, even in routine IV lines. But there’s a hidden danger lurking in plain sight: heparin-induced thrombocytopenia, or HIT. It’s rare, yes - affecting only about 1 to 5 out of every 100 people on heparin - but when it happens, it’s not just a side effect. It’s a medical emergency that can turn a healing patient into someone fighting for their life.
What Exactly Is HIT?
HIT isn’t just a low platelet count. It’s an immune system glitch triggered by heparin. Your body mistakenly sees a complex of heparin and a protein called platelet factor 4 (PF4) as an invader. It builds antibodies to attack it. Those antibodies then latch onto your own platelets, making them clump together and get destroyed. That’s why your platelet count drops - often by half or more. But here’s the twist: while your platelets are disappearing, your blood starts clotting like crazy. The activated platelets spill out pro-coagulant signals, turning your bloodstream into a breeding ground for dangerous clots. This isn’t bleeding - it’s the opposite. You’re more likely to get a stroke, pulmonary embolism, or limb-threatening clot than to bleed out.Two Types of HIT - Only One Is Dangerous
Not all platelet drops from heparin are the same. There are two types:- Type I (benign): Happens within the first two days. Platelets dip slightly, but no clots form. It resolves on its own. No treatment needed.
- Type II (immune-mediated): This is the real threat. It shows up between days 5 and 14 after starting heparin. Platelets crash. Clots form. This is what doctors mean when they say “HIT.”
Who’s at Risk?
HIT doesn’t pick favorites, but some people are far more likely to get it:- Women: 1.5 to 2 times more likely than men.
- People over 40: Risk jumps 2 to 3 times compared to younger adults.
- Post-surgery patients: Especially those who’ve had hip or knee replacements - up to 1 in 10 develop HIT.
- Those on unfractionated heparin: Three times more likely than those on low-molecular-weight heparin (like enoxaparin).
- People on heparin for more than 5 days: Risk climbs from under 0.5% in the first 4 days to 5% after 10 days.
How Do You Know You Have It?
Symptoms don’t always scream “HIT.” Sometimes, they’re quiet - until it’s too late. But watch for these signs:- Sudden swelling, warmth, or pain in one leg - classic deep vein thrombosis (DVT).
- Shortness of breath, chest pain, rapid heartbeat - possible pulmonary embolism (PE).
- Dark, bruised, or blackened skin around a heparin injection site - a red flag for skin necrosis.
- Blue or cold fingers, toes, or nipples - signs of acral ischemia.
- Fever, chills, dizziness, or unexplained anxiety - often reported before major clotting starts.
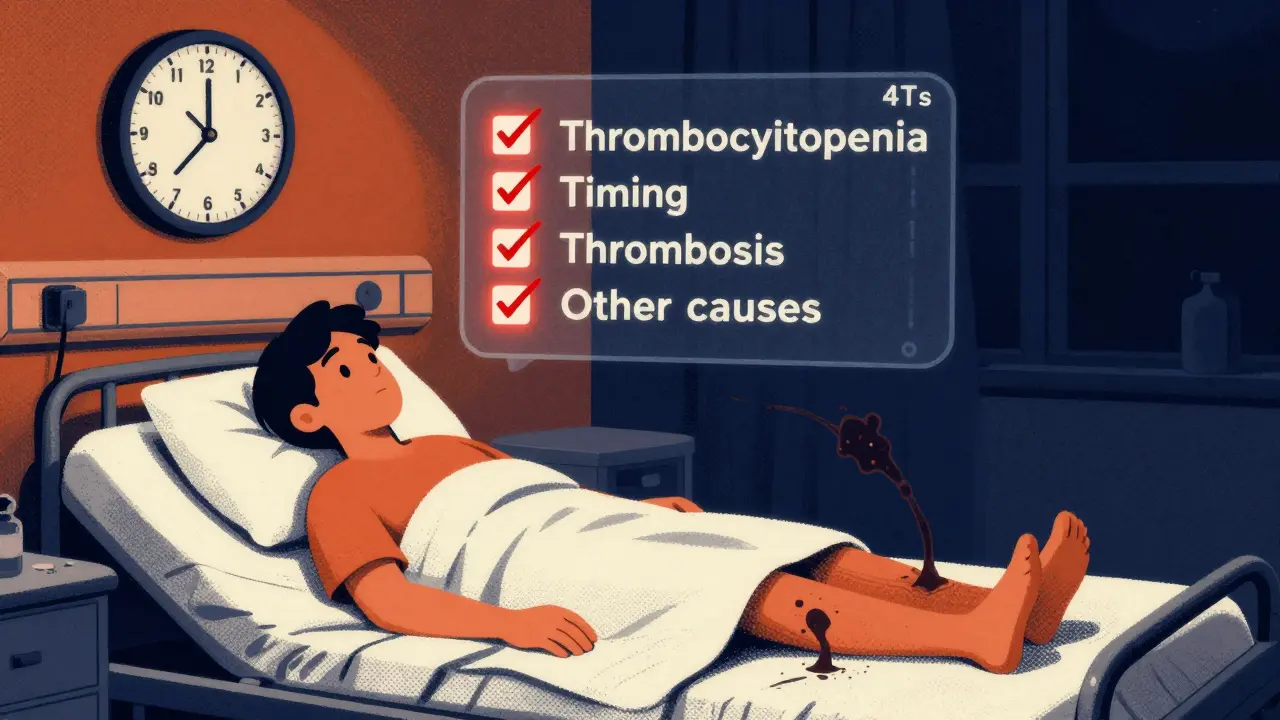
- Thrombocytopenia: How much did platelets drop? (≥50% = 2 points)
- Timing: When did the drop happen? (5-10 days = 2 points)
- Thrombosis: Any new clots? (Yes = 2 points)
- Other causes: Any other reason for low platelets? (No = 1 point)
How Is It Diagnosed?
Testing isn’t simple. First, a blood test checks for antibodies against the PF4-heparin complex. It’s sensitive - catches 95% of real cases - but it’s not perfect. Up to 20% of positive results are false alarms. That’s why the gold standard is a functional test: the serotonin release assay. It checks if your blood actually activates platelets in the presence of heparin. It’s slow, expensive, and only available in big hospitals - but it’s 99% specific. If this test is positive, HIT is confirmed. Even then, about 1 in 1,000 cases slip through. That’s why doctors don’t wait for test results if the clinical picture looks bad. If you’re on heparin, your platelets drop sharply, and you have new clots - stop heparin now.What Happens If You’re Diagnosed?
Stop heparin - all forms. That includes flushes, heparin-coated catheters, even heparin locks on IV lines. One missed source can keep the reaction going. Then, start a non-heparin blood thinner immediately. You can’t wait. The longer you stay on heparin, the higher your chance of dying or losing a limb. Here are the approved alternatives:- Argatroban: Given by IV. Used if you have liver problems. Dose adjusted based on blood clotting tests.
- Bivalirudin: Preferred in heart surgery patients. Short-acting, easy to control.
- Fondaparinux: A once-daily shot. Now recommended as first-line for non-critical cases. Works well if kidneys are okay.
- Danaparoid: Available in some countries. Not in the U.S.
How Long Do You Need Treatment?
If you had HIT without clots, you’ll need anticoagulation for 1 to 3 months. If you had a clot - HITT - you’ll need at least 3 to 6 months. Some need lifelong treatment if they’ve had multiple events. Your doctor will monitor your platelets weekly until they stabilize, then slowly wean you off the alternative anticoagulant.




Siobhan Goggin
January 5, 2026 AT 08:49HIT is terrifying because it looks so innocent at first. I had a friend get it after a routine knee surgery - one day she was walking, the next she couldn’t stand. No bleeding, no obvious warning. Just a drop in platelets and then - boom. Hospital. IVs. Fear. If you’re on heparin past day 4, ask for platelet checks. It’s not extra - it’s essential.
John Ross
January 6, 2026 AT 10:22Let’s cut through the clinical fluff: HIT is a Type II immune-mediated thrombotic disorder triggered by IgG antibodies against PF4-heparin complexes, resulting in platelet activation and consumption. The 4Ts score has a sensitivity of ~90% but specificity is only ~75% without confirmatory functional assays. Fondaparinux is now first-line per ASH 2023 guidelines for non-critical cases - but only if CrCl >30. Argatroban requires aPTT titration every 2-4 hours. And yes - you can get HIT from a heparin flush. I’ve seen it. Stop heparin immediately if platelets drop >50% and clots emerge. No waiting for labs.
Dee Humprey
January 7, 2026 AT 09:46My mom had HIT after her hip replacement. They missed it for two days because her platelets only dropped to 110k. She ended up with a pulmonary embolism. Now I make sure every hospital I go to knows her history. If you’re on heparin longer than 4 days - ask. If you feel sudden pain in your leg or chest - don’t wait. I wish someone had told me sooner. You’re not overreacting. You’re saving your life.
melissa cucic
January 7, 2026 AT 15:56It is, indeed, a matter of considerable clinical significance that heparin-induced thrombocytopenia, despite its relatively low incidence, presents with a paradoxical prothrombotic state, which is counterintuitive to the intended pharmacological effect of anticoagulation. The pathophysiology involves immune complex formation, FcγRIIa receptor-mediated platelet activation, and subsequent thrombin generation. Consequently, the diagnostic algorithm must prioritize clinical suspicion over laboratory confirmation, given the lag time inherent in antibody testing. Furthermore, the administration of warfarin prior to platelet recovery constitutes a documented risk factor for warfarin-induced skin necrosis, which is both morbid and preventable.
Akshaya Gandra _ Student - EastCaryMS
January 9, 2026 AT 07:48wait so heparin can cause blood clots?? i thought it was for preventing them?? i mean i read this but still… like how does that even work??
en Max
January 10, 2026 AT 21:43While I appreciate the clinical overview presented, I must emphasize that the diagnostic ambiguity surrounding HIT necessitates a cautious, algorithm-driven approach. The serotonin release assay remains the gold standard, yet its limited availability in community hospitals creates a significant disparity in care. Furthermore, the reliance on the 4Ts score, while practical, introduces potential for misclassification, particularly in patients with concurrent sepsis or malignancy. Therefore, a multidisciplinary approach involving hematology, pharmacy, and critical care is imperative to mitigate adverse outcomes.
Angie Rehe
January 11, 2026 AT 01:21Why do hospitals still use heparin if this is a known risk? It’s not like we don’t have alternatives. They’re cheap, lazy, and don’t want to change protocols. My cousin lost a foot because the nurse didn’t check his platelets. He was on a heparin lock for 3 days. They didn’t even think to test. This isn’t rare - it’s negligence. Someone needs to get sued. Stop treating patients like lab rats.
Jacob Milano
January 11, 2026 AT 02:22I’ve been a nurse for 18 years and I still get chills thinking about HIT. One day you’re giving a heparin flush like it’s water. The next, you’re watching a 62-year-old woman go from ‘I’m fine’ to ‘I can’t breathe’ in 90 minutes. And the worst part? No one sees it coming - until it’s too late. I started asking every patient on heparin: ‘Any new pain? Swelling? Cold fingers?’ - just to hear them say ‘I didn’t think it mattered.’ It does. It always does.
Enrique González
January 11, 2026 AT 14:42People need to know this. Heparin isn’t harmless. It’s powerful. And sometimes, the thing meant to save you is the thing that almost kills you. If you’re getting surgery or in the hospital - ask about platelet checks. Don’t assume they’re doing it. Ask. Twice. I’ve seen lives saved by one simple question.
Aaron Mercado
January 12, 2026 AT 16:49How is this even allowed? Heparin is given to millions - and yet, no mandatory platelet monitoring? No warning labels? No public awareness campaign? This isn’t negligence - it’s systemic malpractice. People are losing limbs, dying, because hospitals are too cheap to run a simple blood test. And the FDA? Silent. The AMA? Silent. The media? Silent. Until someone’s mother dies, nobody cares. And then - it’s too late.
saurabh singh
January 12, 2026 AT 18:59bro this is wild. in india we use heparin everywhere - even in tiny clinics. no one checks platelets. i had a neighbor get HIT after a tooth extraction - they gave him heparin gel for bleeding gums. he got a clot in his leg. he’s fine now but scared to even get a flu shot. we need more awareness here too. not just in the US.
John Wilmerding
January 14, 2026 AT 16:02For patients who survive HIT, long-term anticoagulation remains a critical consideration. The risk of recurrence is approximately 10-30% if re-exposed to heparin, even after years. Therefore, patient education regarding alternative anticoagulants and strict avoidance of all heparin-containing products - including flushes, catheters, and topical agents - is paramount. Documentation in medical records and patient-held cards should be standard practice.
Peyton Feuer
January 15, 2026 AT 19:09Just wanted to say thank you for writing this. My sister had HIT after her C-section. We didn’t know anything. If I’d read this before, I might’ve pushed harder. Now I tell everyone I know: if you’re on heparin, ask about platelets. Seriously. It’s that simple.