When you pick up a prescription, you might see two options: the familiar brand-name pill with the colorful packaging, or a plain white capsule with a simple label and a much lower price. If you’ve ever wondered whether that cheaper version is really the same, you’re not alone. Millions of people in the U.S. switch to generics every year - and most never notice a difference. But for others, a switch feels like a gamble. So, are generic drugs really just as good as brand-name medications? The short answer: yes. But there’s more to it than that.
They Have the Same Active Ingredient - and That’s What Matters
Generic drugs aren’t copies. They’re exact copies of the active ingredient in the original brand-name drug. That means if you’re taking a brand-name blood pressure pill called Lotrel, the generic version contains the exact same combination of amlodipine and benazepril. The FDA requires this. No exceptions.
The active ingredient is what actually works in your body. It’s the part that lowers your blood pressure, kills bacteria, or balances your thyroid. The FDA doesn’t allow generics to be sold unless they deliver the same amount of that ingredient into your bloodstream at the same rate as the brand. That’s called bioequivalence. To prove it, manufacturers test the drug in 24 to 36 healthy volunteers, measuring how quickly and completely your body absorbs it. The results must fall within 80% to 125% of the brand’s absorption rate. That’s not a wide margin - it’s a tight, scientifically proven standard.
And it’s not just theory. A 2019 study in JAMA Internal Medicine looked at 3.5 million patients taking generics for diabetes, high blood pressure, depression, and osteoporosis. The results? No difference in effectiveness. No increase in hospital visits. No rise in complications. The same outcomes, at a fraction of the cost.
Why Do Generics Look Different?
If the active ingredient is identical, why do generics look so different? Why is the brand-name pill blue and oval, while the generic is white and round? The answer is simple: trademark laws.
Brand-name companies own the look of their pills. That’s why generics have to look different - even if they work the same. That means different fillers, dyes, or coatings. A brand might use sucrose as a filler. The generic might use lactose. One might have a red dye; another might use titanium dioxide. These differences don’t affect how the drug works. But they can matter for a small group of people.
If you’re allergic to a certain dye, or can’t digest lactose, a change in inactive ingredients could cause side effects. That’s rare, but it happens. For most people, though, these differences are invisible. You won’t feel the difference in the pill’s coating or color. You’ll only feel the effect - or lack of effect - of the active ingredient.
What About Narrow Therapeutic Index Drugs?
There’s one big exception: drugs with a narrow therapeutic index (NTI). These are medications where even a tiny change in blood levels can cause problems. Think warfarin (blood thinner), levothyroxine (thyroid hormone), or seizure medications like phenytoin.
For these, the FDA requires stricter bioequivalence standards - 90% to 111% instead of 80% to 125%. That’s because a 10% drop in warfarin might mean a clot. A 10% spike might mean bleeding. For levothyroxine, even a small shift can throw off your TSH levels.
Some doctors and patients prefer to stick with the brand for these drugs. And it’s not just about fear. A 2021 study in the Journal of Clinical Endocrinology & Metabolism found that 5% to 10% of patients on levothyroxine had trouble stabilizing their thyroid levels after switching to a generic. That doesn’t mean generics are unsafe. It means consistency matters. If you’re stable on a brand, switching might not be worth the risk. But if you’re starting fresh, or your doctor says it’s fine, generics are still FDA-approved and safe.

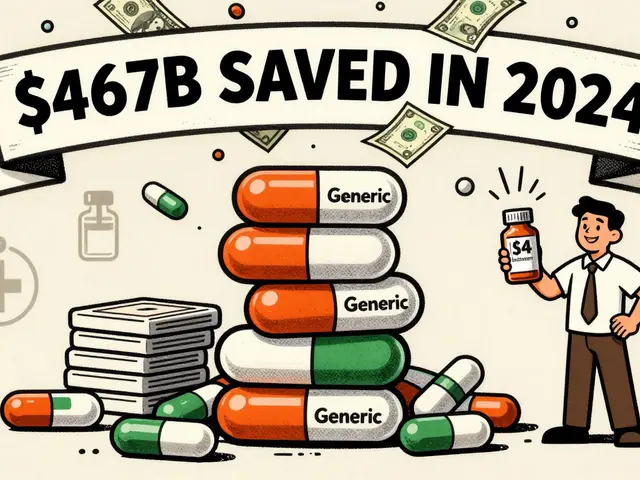
Cost Difference? It’s Not Even Close
Here’s the real reason generics exist: money. Brand-name drugs cost thousands of dollars a year. Generics? Often less than $10 a month.
In 2022, generics made up 90% of all prescriptions filled in the U.S. But they accounted for only 23% of total drug spending. That’s $373 billion saved in one year - enough to cover the healthcare costs of millions of people. The average cash price for a brand-name drug is $685. The generic? Around $15.
Insurance companies push generics hard. Medicare Part D plans require pharmacies to use generics 87% of the time to keep premiums low. Most plans charge you $5 for a generic and $50 or more for the brand. If you’re paying out of pocket, the difference is even starker.
And it’s not just individuals saving money. Hospitals use generics for 97% of their medications. Nursing homes, clinics, and public health programs rely on them. Without generics, the entire U.S. healthcare system would be unaffordable.
Why Do Some People Say Generics Don’t Work?
Despite the data, you’ll still hear stories. “I switched to generic thyroid meds and my energy crashed.” “My seizure came back after the pharmacy changed the pill.” These aren’t made up. People feel real symptoms.
But here’s what’s happening: perception and psychology play a big role. A 2017 study in the Annals of Internal Medicine found that patients who believed generics were inferior were 20% more likely to stop taking them - even when the drug was working fine. That’s no different than thinking a cheap car won’t go as far as an expensive one. The belief changes the behavior.
Another issue? Switching back and forth between different generic brands. One pharmacy might fill your prescription with a generic from India. The next time, it’s from a different manufacturer in China. Even though both meet FDA standards, slight differences in fillers or dissolution rates can cause small fluctuations in how the drug is absorbed - especially for NTI drugs.
And then there’s the placebo effect in reverse. If you expect the generic to be weaker, your body might respond that way. Studies show that even when patients are told they’re getting the same drug, their perception of side effects changes based on the label.

What You Should Do
So what’s the practical advice? Here’s how to make smart choices:
- For most medications - antibiotics, blood pressure pills, statins, antidepressants - generics are perfectly safe and effective. Stick with them.
- For NTI drugs like levothyroxine, warfarin, or seizure meds, talk to your doctor before switching. If you’re stable on a brand, consider staying on it. If you’re starting out, generics are fine - just stay with the same manufacturer once you find one that works.
- Don’t switch pharmacies randomly. If you’re on a sensitive drug, stick with one pharmacy. They’ll keep your prescription filled with the same generic version.
- Use the FDA’s Drugs@FDA database to look up your pill’s appearance. If your generic suddenly looks different, check the name and manufacturer. It might be a different company, not a different drug.
- If you feel something’s off after switching - fatigue, dizziness, worsening symptoms - don’t ignore it. Call your doctor. But don’t assume it’s the generic. It might be something else.
The Bottom Line
Generic drugs aren’t second-rate. They’re not cheap knockoffs. They’re regulated, tested, and proven to work just like the brand-name versions. The FDA doesn’t approve them unless they’re the same. The science says so. The data says so. The savings say so.
Yes, there are rare cases where people need to stick with a brand - especially with complex or critical medications. But for 95% of people, generics are not just cheaper. They’re just as good.
The real problem isn’t the drug. It’s the myth. And that myth costs people money, health, and peace of mind. You don’t need to pay more to get the same result. You just need to know the truth.
Are generic drugs less effective than brand-name drugs?
No. Generic drugs contain the same active ingredient, strength, dosage form, and route of administration as brand-name drugs. The FDA requires them to be bioequivalent, meaning they work the same way in your body. Large studies involving millions of patients show no difference in effectiveness for conditions like high blood pressure, diabetes, and depression.
Why do generic pills look different from brand-name ones?
Trademark laws require generics to look different from brand-name drugs. That means different colors, shapes, sizes, and inactive ingredients like fillers or dyes. These differences don’t affect how the drug works - only the active ingredient does. But if you have allergies to certain dyes or fillers, you should check the ingredients list.
Can I switch between different generic brands?
For most medications, yes. But for drugs with a narrow therapeutic index - like levothyroxine, warfarin, or seizure meds - it’s best to stick with one manufacturer. Even though all generics meet FDA standards, small differences in how they dissolve can affect blood levels. If you switch pharmacies and your pill looks different, check with your pharmacist to see if the manufacturer changed.
Are generic drugs made in the same facilities as brand-name drugs?
Yes. Many generic drugs are made in the same factories as brand-name drugs. The FDA inspects all facilities - whether they make brand or generic - using the same standards. About 78% of active ingredients come from China and India, but those facilities are held to the same quality rules as U.S.-based ones. The FDA conducts regular inspections and can block imports if standards aren’t met.
Why do some people say generics made them feel worse?
Sometimes, it’s because of the inactive ingredients - like a dye or filler they’re sensitive to. Other times, it’s psychological. If you believe generics are weaker, you might notice side effects that aren’t actually there. Switching between different generic manufacturers can also cause small changes in how the drug is absorbed, especially for sensitive medications. If you feel worse after switching, talk to your doctor - but don’t assume it’s the generic. It might be something else.
Is it safe to use generics for chronic conditions like thyroid disease or epilepsy?
For most people, yes. The FDA requires stricter bioequivalence standards for these drugs (90%-111% instead of 80%-125%). But because small changes in blood levels can matter, consistency is key. If you’re stable on a brand, your doctor might recommend staying on it. If you’re starting treatment, generics are safe and effective. The key is to use the same generic version consistently - don’t switch back and forth between manufacturers.
What’s Next?
The future of generics is bright - but not without challenges. The FDA is working to speed up approvals, reduce delays, and improve oversight of overseas manufacturing. New biosimilars - generics for complex biologic drugs like insulin and cancer treatments - are starting to appear. These could bring the same cost savings to treatments that currently cost $100,000 a year.
But the biggest hurdle isn’t science. It’s perception. Until more people understand that a white pill can be just as powerful as a blue one, the myth will persist. And with it, unnecessary spending.
You don’t need to pay more to get the same medicine. You just need to know that the system works - and trust it.


Monte Pareek
December 18, 2025 AT 11:22Let me cut through the noise here - generics aren't just 'as good' they're the same damn thing. The FDA doesn't play games. Same active ingredient same bioequivalence same clinical outcomes. That 2019 JAMA study with 3.5 million patients? That's not a fluke. That's the system working. People panic because the pill looks different but the chemistry doesn't care about color or shape. Your body only responds to the molecule. Stop paying for branding and start saving your damn money.
Connie Zehner
December 20, 2025 AT 02:36Ugh I switched to generic levothyroxine and my heart started racing like I drank 5 espressos 😫 I told my doctor and they said 'it's fine' but I KNOW something was off. I went back to brand and now I'm fine. So no it's not always the same. Don't tell me what my body feels 😤
Kitt Eliz
December 21, 2025 AT 08:39YESSSSS this is such an important conversation 🙌 Generic drugs are the unsung heroes of healthcare! 💪 90% of prescriptions? 23% of costs? That’s not just smart - that’s revolutionary. And for NTI meds? Consistency is KEY. Stick with one pharmacy, one manufacturer, and don’t let the system shuffle your pills like a deck of cards. Your thyroid doesn’t care about marketing - it cares about stability. 💊❤️
Kelly Mulder
December 21, 2025 AT 20:35It is profoundly disingenuous to assert, with absolute certainty, that generics are ‘just as good’ - when, in fact, the bioequivalence standard permits a 20% variance in absorption. That is not ‘the same.’ That is statistically permissible deviation. And when one is managing a condition such as epilepsy or anticoagulation - where a 10% fluctuation can precipitate catastrophic outcomes - to dismiss patient experience as ‘psychological’ is not merely negligent - it is ethically indefensible.
Henry Marcus
December 22, 2025 AT 18:44Ever wonder why the FDA approves generics from India and China but won’t let you import cheaper insulin from Canada? Coincidence? Nah. Big Pharma owns the FDA. They let generics in - but only if they’re still profitable. The real scam? You think you’re saving money - but the same companies that make the brand? They own the generic too. You’re just paying less to the same guy. 🕵️♂️💸
Kathryn Featherstone
December 23, 2025 AT 17:09I’ve been on generic blood pressure meds for 5 years. No issues. My doctor switched me because my insurance wouldn’t cover the brand anymore. I was nervous - but honestly? I didn’t notice a thing. I think people panic because they don’t understand how the system works. The science is solid. Just stick with one pharmacy if you’re on something sensitive.
Sahil jassy
December 25, 2025 AT 16:28From India here and I can confirm generics are made in same factories as brands. My cousin works in a plant that makes both. FDA inspects same way. No difference in quality. Only difference is the label. Save money. Take generic. No drama.
Janelle Moore
December 26, 2025 AT 15:03Wait so if the pills are made in China and India how do we know they’re not full of talc and rat poison? I heard the FDA doesn’t even inspect those factories properly. They just trust them. And what if the active ingredient is real but the coating is laced with something to make you dependent? Like… I don’t know… a slow-acting chemical? 🤔
anthony funes gomez
December 28, 2025 AT 02:21The myth isn’t that generics are inferior - it’s that we’ve been conditioned to equate cost with value. We believe expensive = better because capitalism told us so. But a molecule doesn’t care about your perception. It doesn’t know if you paid $5 or $500. It binds to receptors the same way. The real tragedy? We’re not just paying more - we’re internalizing the lie that we deserve to suffer for our savings. The drug works. Your belief is the only thing that doesn’t.
Marsha Jentzsch
December 29, 2025 AT 09:24My sister switched to generic antidepressants and started crying uncontrollably for 3 days. She said she felt ‘empty.’ Her doctor said it was ‘just adjustment.’ But I looked up the manufacturer - it was a company that got shut down in 2021 for falsifying records. Coincidence? I don’t believe in coincidences. They’re hiding something. And you’re all just too scared to ask the real questions.
Chris porto
December 30, 2025 AT 17:30It’s funny how we treat medicine like it’s magic. We think the brand-name pill has soul because of the logo. But the active ingredient? It’s just chemistry. No brand. No story. No marketing. Just atoms doing their job. Maybe the real issue isn’t the drug - it’s that we’ve forgotten how to trust science when it doesn’t come with a fancy box.