
Acne Treatment Selector
Recommended Treatment
Why This Works For You
Treatment Comparison Overview
Quick Takeaways
- Benzoyl peroxide is fast‑acting but can dry skin; it’s ideal for mild to moderate acne.
- Salicylic acid exfoliates pores and suits oily skin, with lower irritation risk.
- Retinoids (adapalene, tretinoin) remodel skin cells, great for preventing new lesions but need a prescription for stronger forms.
- Azelaic acid offers antibacterial and brightening benefits, useful for sensitive or rosacea‑prone skin.
- Tea tree oil provides a natural, low‑cost option, yet its potency varies between products.
What Is Benzoyl Peroxide?
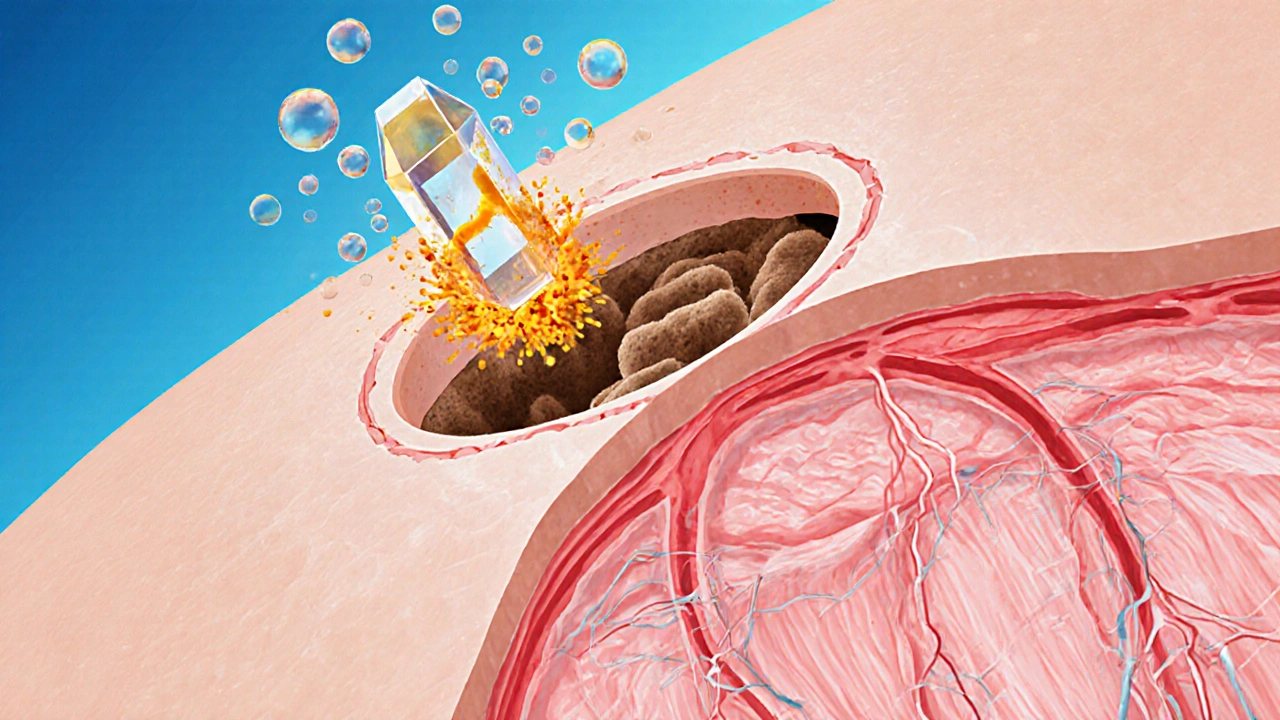
Benzoyl peroxide is a synthetic, oil‑soluble compound that releases oxygen to kill acne‑causing bacteria and reduce inflammation. First approved for acne in the 1960s, it remains a staple in over‑the‑counter (OTC) acne kits worldwide. Typical concentrations range from 2.5% to 10%, with higher strengths delivering quicker results but also more skin dryness.
The way it works is simple: oxygen bursts inside the clogged pore, creating an environment where Cutibacterium acnes (formerly Propionibacterium acnes) can’t survive. This bacterial knock‑down often leads to visible improvement within a week, especially on inflamed pimples.
Popular Alternatives to Benzoyl Peroxide
While benzoyl peroxide is effective for many, several other actives target acne from different angles. Below are the most widely used alternatives, each with its own strengths and drawbacks.
Salicylic Acid
Salicylic acid is a beta‑hydroxy acid (BHA) that dissolves the glue‑like material holding dead skin cells together. By unclogging pores, it prevents comedones before they become inflamed. Concentrations between 0.5% and 2% are common in cleansers and toners. Users often report smoother skin with less redness compared to benzoyl peroxide, making it a go‑to for oily or combination skin.
Retinoids (Adapalene, Tretinoin, etc.)
Retinoids are vitaminA derivatives that speed up cell turnover, pushing trapped keratin out of pores before it can become a pimple. Adapalene 0.1% is available OTC in many countries, while stronger agents like tretinoin require a prescription. Benefits include long‑term acne control and reduction of post‑inflammatory hyperpigmentation, though the initial “purging” phase can be irritating.
Azelaic Acid
Azelaic acid offers antibacterial, keratolytic, and melanin‑inhibiting actions. At 15%-20% concentrations it tackles both inflammatory lesions and the redness that follows. It’s tolerated well on sensitive skin and is often recommended for patients who develop irritation from benzoyl peroxide or retinoids.
Tea Tree Oil
Tea tree oil is a natural essential oil extracted from Melaleuca alternifolia. Its terpinen‑4‑ol component has documented antimicrobial effects against acne bacteria. Products typically contain 5%-10% oil in a carrier base. Because the concentration can vary, results are less predictable, but the low cost and natural label appeal to many.
Prescription Antibiotics
When acne flares become severe, dermatologists may prescribe oral antibiotics such as doxycycline or topical clindamycin. These suppress bacterial growth and reduce inflammatory mediators. However, resistance concerns limit long‑term use, and they’re generally paired with a comedolytic like benzoyl peroxide or a retinoid to maintain effectiveness.
How the Treatments Stack Up
| Attribute | Benzoyl Peroxide | Salicylic Acid | Retinoids | Azelaic Acid | Tea Tree Oil |
|---|---|---|---|---|---|
| Primary Action | Antibacterial, anti‑inflammatory | Keratin loosening, pore unclogging | Cell turnover acceleration | Antibacterial, anti‑keratin, brightening | Antimicrobial (natural) |
| Typical OTC Strength | 2.5%-10% | 0.5%-2% | 0.1% (adapalene) | 15%-20% | 5%-10% (in carrier) |
| Onset of Visible Results | 3-7days | 1-2weeks | 2-4weeks (purging first) | 2-3weeks | Varies, often >4weeks |
| Typical Side Effects | Dryness, peeling, redness | Mild irritation, dryness | Dryness, irritation, photosensitivity | Mild tingling, dryness | Allergic rash, occasional irritation |
| Cost (average 30‑day supply) | $10‑$20 | $8‑$15 | $25‑$45 (prescription) | $30‑$60 | $5‑$12 |
| Best For | Mild‑to‑moderate inflammatory acne | Oily skin, non‑inflamed comedones | Persistent breakouts, post‑acne marks | Sensitive skin, rosacea‑prone | Natural‑product lovers, low‑budget |
Reading the table, you can see that no single product dominates every category. Benzoyl peroxide shines on speed and antibacterial power, but the dryness it brings can push some people toward gentler options like azelaic acid or tea tree oil.
Choosing the Right Treatment for You
Start by asking three simple questions:
- Is my breakout mainly red, inflamed pimples or clogged blackheads?
- How does my skin react to drying or peeling products?
- Do I need a fast fix or a long‑term solution for scars?
If the answer leans toward inflamed lesions and you can handle a bit of dryness, benzoyl peroxide vs alternatives often tips in favor of benzoyl peroxide. If you’re prone to irritation or have a lot of non‑inflamed comedones, consider salicylic acid first. For those who want to prevent future breakouts and improve texture, a retinoid-either a low‑dose OTC adapalene or a prescription option-will likely be the better bet.
Practical Tips & Common Pitfalls
- Start low, go slow. Begin with the lowest effective concentration (2.5% for benzoyl peroxide) and increase only if tolerated.
- Apply to clean, dry skin. Moisture can dilute the active and reduce its antibacterial effect.
- Use a non‑comedogenic moisturizer after the treatment to offset dryness.
- Never mix benzoyl peroxide with strong retinoids in the same step; alternate mornings and evenings to avoid excessive irritation.
- Sun protection is a must, especially when using retinoids or benzoyl peroxide, as both can increase photosensitivity.
- Give any new product at least 4-6weeks before deciding it’s ineffective; acne cycles need time to show change.
Mini FAQ
Can I use benzoyl peroxide and salicylic acid together?
Yes, but keep the concentrations low and apply them at different times of day. For example, benzoyl peroxide in the morning and salicylic acid in the evening helps avoid excess irritation.
Why does my skin feel tight after using benzoyl peroxide?
Benzoyl peroxide releases oxygen, which can strip natural oils. Using a lightweight, fragrance‑free moisturizer restores barrier function and eases the tight feeling.
Is benzoyl peroxide safe for teenage skin?
It’s one of the most studied acne agents and is safe for teens when used as directed. Starting with a 2.5% formula minimizes irritation while still delivering results.
What should I do if I develop a rash from benzoyl peroxide?
Stop the product immediately, rinse with cool water, and apply a soothing barrier cream (e.g., 2.5% zinc oxide). If the rash persists for more than 48hours, consult a dermatologist.
Are natural alternatives like tea tree oil as effective as benzoyl peroxide?
Tea tree oil can reduce bacterial load, but its potency varies between brands. For moderate to severe acne, benzoyl peroxide is generally faster and more reliable.
Next Steps
If you’re ready to try benzoyl peroxide, start with a 2.5% gel, apply a thin layer once daily, and pair it with a gentle moisturizer. Keep a simple log of how your skin reacts for the first two weeks - note any redness, dryness, or breakout changes. Should irritation become a problem, switch to salicylic acid or azelaic acid before moving to a retinoid regimen.
For persistent or cystic acne, schedule a visit with a dermatologist. They can combine benzoyl peroxide with prescription antibiotics or recommend a tailored retinoid plan.
Remember, consistency beats occasional over‑the‑counter heroics. Pick the ingredient that matches your skin’s needs, stick with it, and give it time. The right choice will gradually clear the pores and keep new breakouts at bay.




Sierra Bagstad
October 9, 2025 AT 23:28Benzoyl peroxide operates by releasing molecular oxygen within the follicular lumen, thereby creating an environment hostile to Cutibacterium acnes. The oxidative burst disrupts bacterial cell walls, leading to rapid bacterial clearance. Simultaneously, the peroxide exerts a mild keratolytic effect that helps to desquamate the follicular epithelium. Because the compound is oil‑soluble, it penetrates sebum‑filled pores efficiently. Clinical studies consistently demonstrate visible reduction of inflammatory lesions within three to seven days of twice‑daily application at 2.5 % concentration. However, the same oxidative mechanism also strips sebum, which accounts for the characteristic dryness and peeling. To mitigate barrier disruption, a non‑comedogenic moisturizer should be applied after the peroxide has dried. Users with low tolerance may prefer the 2.5 % formulation before escalating to higher strengths. Overall, the risk‑benefit profile remains favorable for mild‑to‑moderate inflammatory acne.
Alan Kogosowski
October 10, 2025 AT 00:51When evaluating the comparative efficacy of benzoyl peroxide versus its pharmacologic cousins, one must first acknowledge the historical persistence of peroxide in the dermatologist’s armamentarium. Its inception in the 1960s was not merely a fortuitous discovery but rather a calculated response to the burgeoning need for an agent capable of addressing the anaerobic physiology of Cutibacterium acnes. The mechanistic underpinnings involve a redox reaction wherein the peroxide liberates nascent oxygen, thereby oxidizing bacterial protein structures and compromising membrane integrity. Concomitantly, the oxidative milieu provokes a transient inflammatory cascade that paradoxically accelerates the resolution of existent papules by recruiting phagocytic cells to the site. In contrast, salicylic acid functions principally as a beta‑hydroxy acid, dissolving intercellular adhesions within the stratum corneum and facilitating comedonal extrusion without a direct bactericidal action. Retinoids, on the other hand, modulate gene expression through nuclear retinoic acid receptors, expediting keratinocyte turnover and thereby precluding follicular occlusion at a cellular level. Azelaic acid occupies a niche between these modalities, offering antimicrobial activity akin to peroxide while also possessing mild keratolytic properties and a notable pigmentation‑modulating effect. The natural alternative, tea tree oil, contains terpinen‑4‑ol, which has demonstrated in vitro efficacy against acneiform bacteria but suffers from variability in concentration and stability across commercial preparations. From an economic standpoint, benzoyl peroxide remains one of the most cost‑effective options, with a typical thirty‑day supply ranging between ten and twenty dollars, whereas prescription‑strength retinoids can exceed forty dollars per month. Patient adherence, however, is frequently undermined by the xerotic side effects inherent to peroxide, a factor that must be counterbalanced by the judicious use of barrier‑repair moisturizers. Clinical guidelines therefore advocate a stepwise approach: initiate therapy with the lowest effective peroxide concentration, assess tolerance over a four‑to‑six‑week interval, and then consider adjunctive agents if lesion count persists. It is also prudent to counsel patients against the simultaneous application of potent retinoids and high‑strength peroxide, as the combinatorial irritation risk escalates exponentially. Moreover, photoprotection cannot be overstated; both peroxide and retinoids sensitize the epidermis to ultraviolet radiation, necessitating daily broad‑spectrum sunscreen usage. In summation, while no single agent universally outperforms the others across all acne phenotypes, benzoyl peroxide remains unparalleled in its rapid bactericidal onset for inflammatory lesions. Thus, the clinician’s task is to individualize therapy, calibrating potency, adjuncts, and supportive skincare to harmonize efficacy with tolerability.
Ben Lee
October 10, 2025 AT 02:14I've found that pairing a low‑strength benzoyl peroxide gel with a gentle moisturizer works well for most people. If your skin is on the oily side, you can stay with a 2.5 % formula in the morning and add a BHA at night. This routine addresses both the bacterial load and the clogged pores without over‑loading the barrier. Consistency is key; give it at least a month before deciding if it’s effective.
David Brice
October 10, 2025 AT 03:38I get why you love the science, but seriously, if you keep slappin' peroxide on raw skin without a moisturizer, you're just invitin' a flare‑up. Start with a pea‑sized dab, let it dry, then lock in moisture – that's how you avoid the hellish peeling. If you ignore the dryness, you'll end up with more breakouts than before, so get it together!
Zachary Schroer
October 10, 2025 AT 05:01Benzoyl peroxide is cheap 🙄 its results are fast 😎 tea tree oil is cheap too but slower 😐
Mina Berens
October 10, 2025 AT 06:24Tea tree oil can be a fun budget option 😊
Moritz Bender
October 10, 2025 AT 07:48From a pharmacodynamic perspective, benzoyl peroxide exhibits a dose‑dependent oxidative burst that targets the lipophilic microenvironment of the pilosebaceous unit, whereas salicylic acid’s β‑hydroxy acid functionality mediates keratolysis via desmosomal disruption. In terms of comedogenesis inhibition, retinoids engage nuclear retinoic acid receptors (RARs) to modulate gene transcription of keratinocyte differentiation markers, thereby curtailing hyperkeratinization. Azelaic acid provides a tri‑modal mechanism-antimicrobial, anti‑inflammatory, and melanin‑inhibitory-making it a versatile candidate in mixed‑type acne pathophysiology. For clinicians seeking a cost‑effective yet efficacious regimen, initiating therapy with a 2.5 % benzoyl peroxide gel, followed by a non‑comedogenic emollient, remains a pragmatic protocol.
florence tobiag
October 10, 2025 AT 09:11Honestly, the whole “cheapest wins” narrative is, frankly, a myth, because, while benzoyl peroxide is inexpensive, it also, paradoxically, can precipitate barrier disruption, which, in turn, may exacerbate inflammatory cascades, and, let’s not forget, that the variability in formulation purity across generic brands is, undeniably, a hidden variable that can skew outcomes; therefore, one must, indeed, scrutinize the excipient list before declaring any one agent the unequivocal champion.
Terry Washington
October 10, 2025 AT 10:34Enough with the lukewarm compromises! Benzoyl peroxide is the juggernaut of acne warfare, annihilating bacteria with surgical precision, while the so‑called “natural alternatives” are nothing but placebo palliatives for the lazy. If you’re not willing to endure a little dryness, you’re simply not serious about clear skin. Ignite your regimen, embrace the antiseptic blaze, and watch those papules vanish like smoke in a gale.
Claire Smith
October 10, 2025 AT 11:58While the fervor expressed is noted, it is essential to acknowledge that dermatological therapeutics must balance efficacy with tolerability. Over‑emphasizing aggressive measures without consideration of individual skin barrier integrity may lead to adverse outcomes, which contravenes evidence‑based practice standards.
Émilie Maurice
October 10, 2025 AT 13:21Your post contains several factual inaccuracies and several grammatical errors; it should be revised for clarity and correctness.
Ellie Haynal
October 10, 2025 AT 14:44Oh my gosh, this whole debate feels like a soap opera, and I'm totally here for the drama! 😱 The clash between peroxide and the “gentle” alternatives is the ultimate plot twist, and I can’t wait to see who wins the final episode of flawless skin.