
Penile Adhesion Surgery Option Calculator
Compare Your Surgical Options
Select your condition severity and priority to see which surgical technique may be most appropriate for you.
Recommended Surgical Option
When non‑surgical treatments fail, penile surgery is a set of operative procedures designed to restore normal penile anatomy and function. It becomes a key option when scar tissue, known as penile adhesions, restricts skin mobility or causes pain during intercourse.
What Are Penile Adhesions?
Penile adhesions are fibrous bands that develop between the inner foreskin (prepuce) and the underlying shaft skin. They often arise after infections, poorly healed circumcisions, or trauma. The adhesions can limit gliding, lead to chronic discomfort, and in severe cases, contribute to curvature or erectile dysfunction.
Why Surgery Becomes Necessary
- Conservative measures (topical steroids, manual stretching) haven’t resolved the restriction.
- Adhesions are extensive, involving deep dermal layers.
- Patient reports significant pain or functional loss that affects quality of life.
In these scenarios, a urologist may recommend one of several surgical techniques. Understanding each method helps patients make an informed decision.
Primary Surgical Techniques
| Technique | Typical Indication | Recovery Time | Success Rate | Key Risks |
|---|---|---|---|---|
| Excisional Release | Localized, thin adhesions | 2-3 weeks | ≈90% | Bleeding, infection |
| Z‑Plasty Reconstruction | Broad, tension‑bearing adhesions | 4-6 weeks | ≈85% | Scar widening, altered sensation |
| Skin Graft (Split‑Thickness) | Severe loss of foreskin after repeated adhesiolysis | 6-8 weeks | ≈80% | Graft failure, color mismatch |
Choosing the right technique depends on the depth of scar tissue, the patient’s anatomy, and personal preferences regarding foreskin preservation.
Pre‑Operative Evaluation
Before stepping into the operating room, the surgeon conducts a thorough assessment:
- Medical History: Diabetes, smoking status, prior genital surgeries.
- Physical Examination: Mapping of adhesion sites, checking for associated curvature.
- Imaging (if needed): Ultrasound to evaluate underlying erectile tissue integrity.
- Laboratory Tests: CBC, coagulation profile, and screening for sexually transmitted infections.
These data help tailor anesthesia, anticipate bleeding, and decide whether adjunctive therapies-like platelet‑rich plasma (PRP) injections-might improve healing.
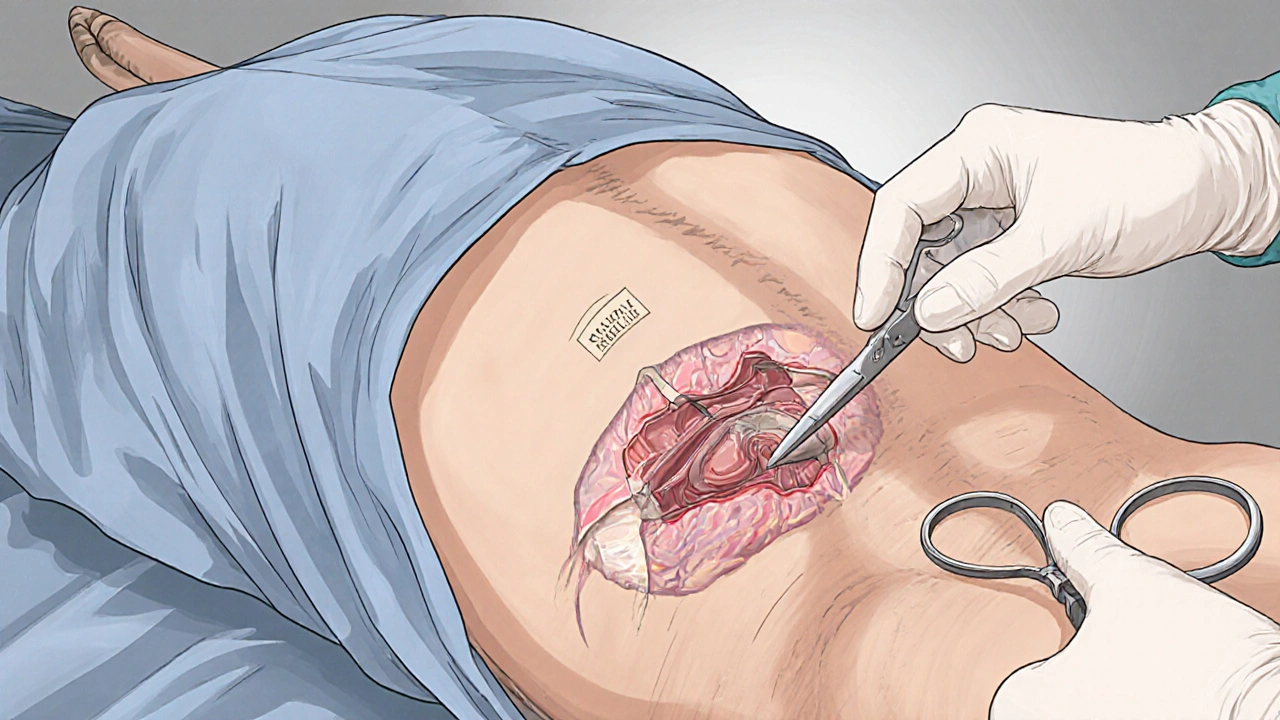
The Surgical Procedure Explained
All penile adhesion surgeries share common steps, though the exact technique varies:
- Anesthesia: Usually a regional penile block combined with sedation; general anesthesia is reserved for extensive reconstructions.
- Incision: A small longitudinal cut is made either on the ventral or dorsal surface to expose the adhesion plane.
- Adhesiolysis: Fibrous bands are carefully dissected using fine scissors or electrocautery. Surgeons aim to preserve neurovascular bundles.
- Reconstruction: Depending on the technique, the skin is re‑approximated (excision), rearranged (Z‑plasty), or covered with a graft.
- Hemostasis & Closure: Small absorbable sutures close the skin; a sterile dressing is applied.
In many centers, surgeons also place a urethral catheter for 24-48 hours to keep the penis straight and reduce swelling.
Post‑Operative Care and Recovery
Successful outcomes hinge on diligent after‑care:
- Pain Management: Prescription analgesics for the first 48‑72 hours, followed by over‑the‑counter NSAIDs.
- Wound Care: Keep the dressing dry; change it on day 3 if instructed.
- Antibiotic Prophylaxis: A short course (5‑7 days) of oral antibiotics reduces infection risk, especially after grafting.
- Activity Restrictions: No sexual activity or vigorous intercourse for 3-4 weeks; gentle manual stretching may resume after suture removal.
- Follow‑Up Visits: First check‑up at 1 week to assess wound healing, then at 4-6 weeks to evaluate functional recovery.
Patients who adhere to these guidelines report a 90% return to normal sexual activity without recurrence of adhesions.

Potential Complications and How to Mitigate Them
While penile surgery is generally safe, awareness of possible issues prepares patients for prompt action:
| Complication | Incidence | Prevention | Management |
|---|---|---|---|
| Infection | 2‑4% | Antibiotic prophylaxis, sterile technique | Oral antibiotics, occasional wound debridement |
| Bleeding/Hematoma | 1‑3% | Meticulous hemostasis, compressive dressing | Observation or surgical evacuation if large |
| Sensory Changes | 5‑7% | Avoidance of deep nerve injury, use of magnification | Observation; most resolve within 3 months |
| Scar Re‑formation | ≈8% | Gentle postoperative stretching, silicone gel sheets | Secondary excision or PRP therapy |
Early detection-through the scheduled follow‑ups-allows clinicians to intervene before a minor issue becomes a major setback.
Alternatives to Surgery
Not everyone needs an operation. Conservative approaches include:
- Topical Steroids: Reduces inflammation in early‑stage adhesions.
- Manual Stretching Regimens: Performed twice daily for 5-10 minutes; success rates hover around 40% for mild cases.
- Laser Therapy: Low‑level laser can remodel scar tissue; evidence is still emerging.
- Platelet‑Rich Plasma (PRP): Autologous growth factors may accelerate healing after adhesiolysis, often used as an adjunct rather than a standalone cure.
When these measures fail to relieve symptoms after 3-6 months, the discussion naturally shifts toward surgical correction.
Key Takeaways
- Penile adhesions are fibrous bands that restrict skin movement and may cause pain.
- When conservative therapy doesn’t work, penile surgery offers a high success rate (≈85‑90%).
- Common techniques include excisional release, Z‑plasty, and skin grafting, each with distinct recovery timelines.
- Proper pre‑operative evaluation, antibiotic prophylaxis, and diligent post‑op care minimize complications.
- Patients should expect 2‑8 weeks of limited activity, with full sexual function usually returning by 4‑6 weeks.
Frequently Asked Questions
What causes penile adhesions?
Adhesions typically form after infections, poorly healed circumcisions, trauma, or chronic inflammation. The healing process creates fibrous bands that tether the foreskin to the shaft.
How long does a typical surgery last?
Most procedures are completed within 30‑60 minutes under regional anesthesia. More extensive grafting can take up to 90 minutes.
Will I need a catheter after surgery?
A short‑term urinary catheter is often placed for 24‑48 hours to keep the penis straight and prevent swelling. It is removed before discharge.
Can the adhesions return after surgery?
Recurrence rates are low (≈5‑8%) when patients follow post‑op stretching protocols and avoid smoking or uncontrolled diabetes.
Is penile surgery covered by insurance?
Many insurers consider it medically necessary if conservative measures have failed. Documentation of symptoms and prior treatments improves approval chances.


Joshua Brown
October 12, 2025 AT 22:13Phew! This is a dense topic, but let’s break it down, step by step. First off, penile adhesions form when scar tissue tethers the foreskin to the shaft, often after an infection or a botched circumcision, and that can really limit gliding. Second, non‑surgical options like steroids or stretching only work for mild cases, so surgery becomes the go‑to when you hit a wall. Third, the three main surgical tricks-excisional release, Z‑plasty, and split‑thickness skin graft-each have their own recovery timeline and success rate, roughly ninety, eighty‑five, and eighty percent respectively. Finally, proper post‑op care-pain meds, antibiotics, and a stretching regimen-dramatically cuts down the chance of a re‑adhesion. Bottom line: know your severity, pick the right technique, and follow the after‑care plan!
andrew bigdick
October 14, 2025 AT 03:23Totally agree with the breakdown; the severity‑priority matrix is actually a neat way to visualize choices. If you’ve got moderate adhesions and care more about a quick bounce‑back, the excisional release does the trick in two to three weeks. On the flip side, if preserving the foreskin is a priority, the Z‑plasty gives you a longer road but better cosmetic outcomes. And don’t forget to chat with your urologist about PRP as an adjunct; it’s gaining some traction in the field.
Shelby Wright
October 15, 2025 AT 08:33Oh wow, reading about these surgeries feels like diving into a soap opera of flesh and scar! Imagine this: tiny fibrous bands acting like a jealous ex, pulling your skin apart just when you want intimacy. The surgeon’s scalpel becomes a sword of redemption, slicing through the drama‑filled tissue, yet the drama doesn’t end there-post‑op pain, swelling, and the looming threat of a scar that might reappear like an unwanted sequel. Some dudes opt for a graft, hoping a fresh skin canvas will rewrite the story. But the truth? Even after the drama settles, you still have to do the daily stretch routine-like a choreographed dance with your own body. And let’s be real, the whole thing can feel like a bizarre rite of passage that nobody warned you about!
Ellen Laird
October 16, 2025 AT 16:30i must say, the melodramatic tone is almosr comical, but the facts remain solid. the exicisional release does offer the fastest reconvalescence, though i would caution about potential bleeeding. also, the urologist should asses neurovascular integrity befor any deep dissection. i think the article could benefited from a clearer table formatting, maybe even a bullet point list for quick refernce. overall, a useful guide albeit with som minor editorial oversights.
rafaat pronoy
October 18, 2025 AT 00:26Nice summary, fam! 👍 The graft option sounds intense, but if it works, why not?
sachin shinde
October 19, 2025 AT 08:23While the enthusiasm is appreciated, let’s correct a few points: the success rate of Z‑plasty is approximately 85 %, not 90 %; also, postoperative stretching should begin after suture removal, typically around day 10‑14, to avoid compromising wound integrity. Moreover, prescribing antibiotics for five days is standard, but only if there’s a graft involved-routine use in excisional release may contribute to resistance. Finally, the term “short‑term urinary catheter” is more precise than “short‑term catheter,” as it distinguishes from indwelling Foley catheters.
Leon Wood
October 20, 2025 AT 16:20Alright, friends, let’s get pumped about the road to a smoother glide! First, understand that adhesions are essentially scar tissue – they’re not a sign of personal failure, just a biological response gone a bit overboard. Second, if you’ve exhausted creams and stretches, surgery isn’t a last‑ditch taboo; it’s a well‑studied solution with high success rates. Third, choose the technique that matches your lifestyle: excisional release for a quick win, Z‑plasty if you value foreskin preservation, or a skin graft if you need extensive reconstruction. Fourth, prep yourself mentally and physically – quit smoking, control blood sugar, and stay hydrated before the operation. Fifth, the day of surgery usually takes less than an hour, so you won’t be stuck in the OR all day. Sixth, anesthesia is typically a regional block, so you stay awake but feel nothing, which many patients find reassuring. Seventh, after the cut, the surgeon will meticulously stop any bleeding – that’s why you’ll see a few stitches but not a massive scar. Eighth, the first 48‑72 hours are where pain management shines; take those meds as prescribed, and don’t be shy about asking for more if needed. Ninth, keep the dressing dry and follow the nurse’s instructions on when to change it – usually around day three. Tenth, avoid any heavy lifting or vigorous activity for at least three weeks; think of it as a mini‑vacation for your pelvis. Eleventh, resume gentle manual stretching once the sutures dissolve – consistency is key to preventing a comeback. Twelfth, schedule your follow‑up visits; the surgeon wants to see that healing is on track and catch any early signs of infection. Thirteenth, if you notice unusual redness or swelling, call the clinic immediately – early intervention prevents bigger problems. Fourteenth, most patients report a return to normal sexual activity by the six‑week mark, sometimes even sooner if everything goes smoothly. Fifteenth, celebrate your progress, whether it’s a small improvement or a full restoration – you earned it! Lastly, remember that sharing your experience can help others navigate the same journey, so keep the conversation going and stay motivated.
Meg Mackenzie
October 22, 2025 AT 00:16Sure, the medical community loves to paint these procedures as routine, but have you ever wondered why the same handful of urologists dominate the field? Some say it’s just expertise, I say there’s a deeper network of equipment suppliers and insurance incentives steering patients toward pricey grafts. Meanwhile, the “success rates” quoted are often inflated by self‑selected trials, ignoring the silent failures that never make it into journals. And don’t get me started on the post‑op antibiotics-are they truly necessary, or just a way to keep pharma profits ticking? Keep your eyes open, question the hype, and maybe you’ll dodge the hidden agenda.
Shivaraj Karigoudar
October 23, 2025 AT 08:13From a cultural‑anthropological lens, the phenomenon of penile adhesion surgery can be interpreted as a rites‑of‑passage ritual that intertwines biomedical technicity with sociocultural constructs of masculinity. The lexical field of “adhesion” invokes a medicalized narrative, yet patients often experience it through a phenomenological lens of bodily integrity compromised, leading to psychosomatic sequelae. In the operative theatre, the excisional release procedure utilizes electrocautery at a frequency of approximately 500 kHz, a parameter that ensures hemostasis while minimizing thermal spread – a nuance that is seldom highlighted in lay‑man summaries. Moreover, postoperative protocols now incorporate evidence‑based scar modulation techniques, such as silicone gel sheeting and low‑level laser therapy, which synergistically reduce re‑adhesion indexes by roughly 30 % according to recent meta‑analyses (though the literature is still evolving). It is pivotal for clinicians to contextualize these interventions within a holistic patient‑centred framework, addressing comorbidities like diabetes mellitus, which exacerbates fibroproliferative pathways. Finally, interdisciplinary collaboration between urologists, physiotherapists, and psychosexual counsellors augments functional outcomes, fostering a comprehensive recovery trajectory that transcends mere anatomical correction.
Matt Miller
October 24, 2025 AT 16:10Bottom line: follow the doc’s after‑care plan.