When you take CBD oil along with your prescription meds, you might not realize you're playing a high-stakes game with your liver enzymes. It's not just about feeling relaxed-it's about whether your blood thinner, seizure medicine, or antidepressant is working the way it should. The science is clear: CBD doesn't just sit there. It actively interferes with how your body breaks down dozens of common medications, and that interference can lead to dangerous sedation, overdose, or treatment failure.
How CBD Disrupts Your Medications
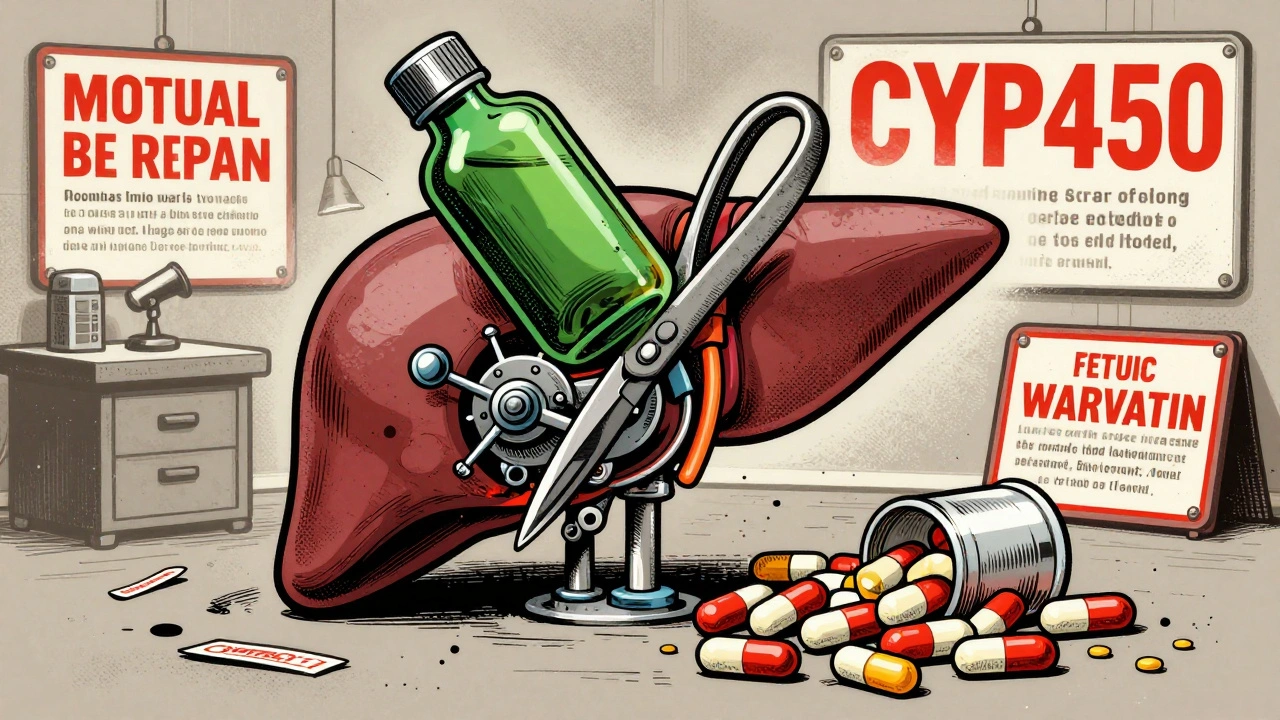
Your liver uses a family of enzymes called CYP450 to break down about 80% of all prescription drugs. Think of them like tiny molecular scissors that chop up medications so your body can get rid of them. CBD doesn’t just pass through-it slams on the brakes. It binds tightly to key enzymes like CYP2C9, CYP2C19, and CYP3A4, blocking them from doing their job. When those enzymes are inhibited, your meds don’t get broken down as quickly. That means they build up in your bloodstream, sometimes to toxic levels.
Take clobazam, a common anti-seizure drug. When taken with CBD, its active metabolite-N-desmethylclobazam-can spike by 60%. That’s not a small bump. In real patients, that’s the difference between feeling calm and being so drowsy you can’t get out of bed. One epilepsy patient on Reddit reported his clobazam levels jumped from 600 ng/mL to over 1,050 ng/mL after starting CBD. His neurologist had to cut his dose in half just to keep him alert.
Warfarin is another big red flag. This blood thinner has a razor-thin safety margin. Too little, and you risk a clot. Too much, and you bleed internally. A patient on PatientsLikeMe saw his INR-his blood clotting measure-jump from 2.5 to 5.8 in just ten days after adding CBD oil. That’s nearly triple the upper limit of safety. He needed emergency vitamin K to reverse it.
Which Medications Are Most at Risk?
Not all drugs are affected equally. The biggest dangers come from medications metabolized by CYP2C9, CYP2C19, CYP2D6, and CYP3A4. Here’s who’s most vulnerable:
- CYP2C9: Warfarin, phenytoin, ibuprofen, losartan
- CYP2C19: Clobazam, diazepam, omeprazole, clopidogrel
- CYP2D6: Amitriptyline, fluoxetine, codeine, metoprolol
- CYP3A4: Fentanyl, simvastatin, cyclosporine, many cancer drugs
These aren’t obscure drugs. They’re daily prescriptions for millions. The FDA’s own label for Epidiolex-the only FDA-approved CBD drug-warns explicitly about interactions with clobazam and valproate. That’s not a footnote. It’s a warning sign.
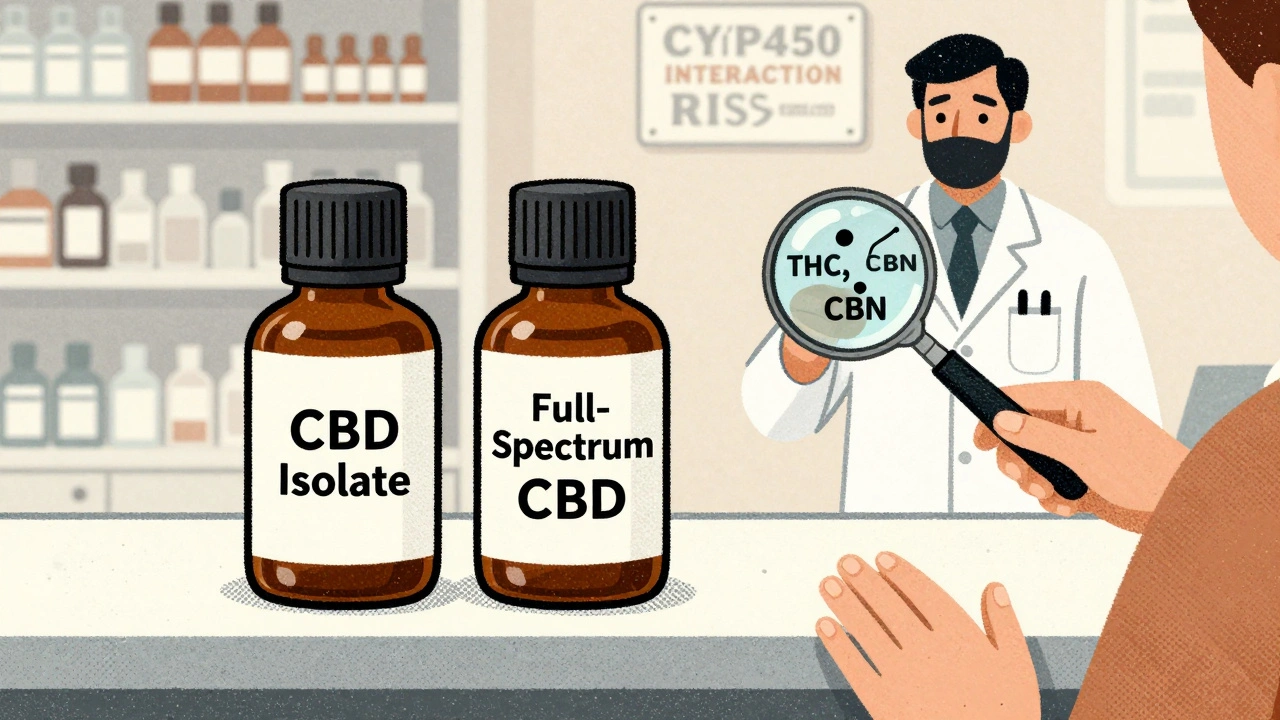
Even more concerning? Many CBD products contain more than just CBD. THC, CBG, CBN-other cannabinoids-also inhibit CYP enzymes. THC hits CYP2C19 hard. CBN hits CYP2B6. And the metabolites? They’re just as active. One study found that THC-COO-Gluc, a major breakdown product of THC, is a potent inhibitor too. So even if your CBD oil claims to be “THC-free,” your body might still be processing compounds that interfere with your meds.
Why Sedation Happens-and Why It’s Dangerous
Sedation isn’t just “feeling sleepy.” It’s brain fog, slowed breathing, impaired coordination, and in extreme cases, respiratory depression. When CBD slows the breakdown of sedatives like benzodiazepines (diazepam, clonazepam) or opioids (fentanyl, oxycodone), those drugs linger longer and hit harder.
A 2023 study of 217 medical cannabis users found that 34% experienced increased sedation when combining CBD with their prescriptions. But the real shocker? Among those taking CYP2C19-metabolized drugs, over half reported extreme drowsiness. That’s not coincidence. That’s pharmacology.
And here’s the twist: some people see sedation as a bonus. One chronic pain patient on Healthgrades said CBD let his doctor cut his fentanyl dose by 40%. He didn’t feel withdrawal, and his pain stayed controlled. That’s not luck. It’s CYP3A4 inhibition working in his favor. But that’s the exception-not the rule. You can’t predict who will benefit and who will overdose.

The Problem with Unregulated CBD Products
Here’s where it gets worse: most CBD products aren’t regulated. A 2022 JAMA Network Open study found that 42% to 121% of the CBD listed on the label was actually in the bottle. That means you think you’re taking 25 mg, but you might be getting 10 mg-or 30 mg. No one’s checking. No one’s testing. And no one’s telling you what else is in there.
And yet, 45% of CBD users in the U.S. take it alongside prescription drugs, according to the National Institute on Drug Abuse. That’s millions of people mixing untested, unregulated substances with life-saving medications. The FDA has sent 15 warning letters to CBD companies for failing to include interaction warnings on labels. That’s not oversight. That’s damage control.
What You Should Do
If you’re on any prescription medication and thinking about CBD-or already using it-here’s what to do:
- Talk to your doctor or pharmacist before starting. Don’t assume it’s safe because it’s “natural.”
- Know your meds. Check if yours are metabolized by CYP2C9, CYP2C19, CYP2D6, or CYP3A4. A quick Google search of your drug name + “metabolized by” will tell you.
- Ask for therapeutic drug monitoring. For drugs like warfarin or clobazam, your doctor can check blood levels before and after starting CBD. That’s the only way to know if something’s off.
- Start low, go slow. If you’re already on a sensitive medication, begin with 5 mg of CBD per day and wait at least a week before increasing. Watch for dizziness, fatigue, or unusual bleeding.
- Separate doses. Take your CBD and your prescription meds at least 3-4 hours apart. It won’t stop inhibition, but it might reduce peak concentrations.
- Consider alternatives. CBG and CBDV show less CYP inhibition in early studies. They’re not proven, but they might be safer options if you need a cannabinoid without the risk.
What’s Being Done About It
Experts aren’t ignoring this. The American Society of Health-System Pharmacists now advises avoiding CBD with drugs that have a narrow therapeutic index-meaning the difference between effective and toxic is tiny. The University of Maryland runs a 12-hour CME course for doctors on managing these interactions. Over 1,200 clinicians have taken it.
The European Medicines Agency now requires all cannabinoid medicines to include CYP450 interaction data on their labels. In the U.S., the NIH is funding a major study (NCT04893224) to measure exactly how CBD affects warfarin levels. Results are expected by late 2024.
And the market is responding. The CBD-drug interaction testing industry is projected to grow from $127 million in 2023 to nearly $500 million by 2028. That’s because clinics and pharmacies are realizing they can’t afford to guess anymore.
The Bottom Line
CBD isn’t harmless. It’s a powerful biological modifier. It changes how your body handles medicine. That can be helpful-or deadly. There’s no universal safe dose. There’s no “it’s just CBD” excuse. If you’re on a prescription, you’re at risk.
The good news? These interactions are predictable. They’re measurable. And they’re manageable-if you’re informed. Don’t rely on anecdotal stories or marketing claims. Talk to your provider. Get your levels checked. Track your symptoms. Your safety isn’t optional.
What you’re doing with CBD isn’t just wellness. It’s pharmacology. Treat it like it.
Can CBD oil replace my prescription medication?
No. CBD is not a substitute for prescribed medications like anticonvulsants, blood thinners, or antidepressants. While it may help with symptoms like anxiety or pain, it does not have the same proven therapeutic effect as FDA-approved drugs. Stopping your medication without medical supervision can lead to serious health consequences, including seizures, strokes, or worsening mental health conditions.
How long does CBD stay in my system and affect my medications?
CBD can remain detectable in your bloodstream for 2 to 5 days, depending on your dose, frequency, and metabolism. But its inhibitory effects on liver enzymes can last even longer-up to a week or more after your last dose. This means even if you take CBD every other day, it can still interfere with your medications daily. Don’t assume skipping a day makes it safe.
Is full-spectrum CBD more dangerous than isolate?
Yes, generally. Full-spectrum CBD contains THC, CBN, and other cannabinoids, all of which inhibit CYP450 enzymes. THC inhibits CYP2C19, and CBN affects CYP2B6 and CYP2C9. Even small amounts can add to the overall inhibitory effect. CBD isolate is cleaner, but it still blocks key enzymes. Neither is risk-free when combined with prescription drugs.
Can I use CBD if I’m on antibiotics or birth control?
Birth control pills are metabolized by CYP3A4, which CBD strongly inhibits. This can reduce the effectiveness of hormonal contraceptives, increasing the risk of unintended pregnancy. Some antibiotics, like clarithromycin, also interact with CYP3A4. Combining them with CBD can raise blood levels of both drugs, increasing side effects like nausea, dizziness, or liver stress. Always check with your doctor before combining CBD with any new medication.
Are there any CBD products that are safer for people on medications?
There are no CBD products guaranteed to be safe with medications, but some show less CYP inhibition in early research. CBG and CBDV appear to have weaker effects on liver enzymes than CBD or THC. However, these are not widely available, and clinical data is limited. The safest approach is to avoid CBD entirely if you’re on critical medications-or use it only under close medical supervision with regular blood tests.
What should I do if I feel overly sleepy after starting CBD?
Stop taking CBD immediately and contact your doctor. Excessive sedation can be a sign of drug accumulation, especially if you’re on benzodiazepines, opioids, or antiepileptics. Your doctor may order a blood test to check medication levels and adjust your doses. Do not wait for symptoms to worsen. Sedation can progress to respiratory depression, which is life-threatening.



Gareth Storer
December 5, 2025 AT 12:56So let me get this straight - you’re telling me the same stuff I’ve been using to chill after work is quietly sabotaging my blood thinner like a silent assassin in my liver? Thanks, Big CBD.
And the worst part? I paid $80 for a bottle that says ‘100% Pure’ - turns out it’s just THC and wishful thinking with a side of FDA warning letters.
Next time I’ll just drink whiskey. At least I know what it’s doing to me.
Pavan Kankala
December 7, 2025 AT 03:42They don’t want you to know this - but the FDA, Big Pharma, and the CBD industry are all in bed together. Why? Because if people realized how much control these enzymes have, they’d stop taking pills altogether.
CBD isn’t the problem - it’s the truth. The system wants you dependent on meds that get broken down by enzymes they don’t want you to understand.
They call it ‘interaction.’ I call it liberation.
They banned cannabis for decades. Now they’re scared it works too well.
Wake up.
They’re poisoning you with prescriptions and selling you CBD as the villain. Classic.
Martyn Stuart
December 7, 2025 AT 20:34Important note: CBD’s inhibition of CYP450 is dose-dependent, reversible, and clinically significant - especially with chronic use.
That said, not everyone will experience interactions - but the risk is real enough that it warrants caution, particularly with narrow-therapeutic-index drugs like warfarin, clobazam, or cyclosporine.
Always disclose CBD use to your pharmacist - they’re trained to catch these interactions, and they’re often the first line of defense.
Also: ‘THC-free’ doesn’t mean ‘enzyme-safe.’ Even trace contaminants or metabolites can contribute.
And yes - separating doses by 3–4 hours helps slightly, but doesn’t eliminate inhibition. It’s like turning down the volume on a fire alarm - the alarm’s still on.
Bottom line: If your med has a black box warning or requires blood monitoring, assume CBD is a co-conspirator.
Check your drug’s metabolism on drugs.com or RxList. It’s a 30-second google search that could save your life.
Jessica Baydowicz
December 8, 2025 AT 14:10Y’all. I was skeptical too - until I started using CBD for anxiety and my doc found my Lexapro levels had doubled.
Turns out I was basically self-administering a higher dose without knowing it. Scary stuff.
But here’s the good news: once I told my doctor, we adjusted my dose, I switched to a low-dose isolate, and now I’m feeling like my old self again - calm, clear, and not half-asleep at my desk.
You don’t have to give up CBD - just don’t go rogue. Talk to someone who knows what they’re doing. You’re worth the conversation.
And yes - your pharmacist is your new bestie. Go say hi.
Love you all. Stay safe, stay informed. 💪
Shofner Lehto
December 8, 2025 AT 21:07Let’s not romanticize this. CBD isn’t magic. It’s a biochemical modulator with real pharmacokinetic consequences. The fact that people treat it like herbal tea while on anticoagulants or antiepileptics is alarming.
The FDA approved Epidiolex because they had to - not because it’s safe for everyone. The label warnings exist for a reason.
And no, ‘natural’ doesn’t mean ‘safe.’ Arsenic is natural.
Stop using anecdotal Reddit stories as medical advice. Your liver doesn’t care how ‘holistic’ you feel.
Get your levels checked. Talk to your prescriber. Or keep gambling with your health - I’m not your mom.
But I am your conscience.
Emmanuel Peter
December 10, 2025 AT 17:50Everyone’s freaking out about CBD and CYP450, but nobody’s talking about how SSRIs and statins are basically poison pills that need constant monitoring anyway.
Why are we acting like CBD is the first thing to mess with your liver?
Alcohol? Cigarettes? Grapefruit? Those are the real villains.
And don’t even get me started on how many people take ibuprofen daily and never think twice.
So yeah - CBD inhibits enzymes. So does coffee. So does stress. So does sleep deprivation.
Maybe the problem isn’t CBD - maybe it’s that we’ve turned our bodies into chemical soup and now we’re surprised when something else gets in the mix.
Let’s fix the system, not blame the supplement.
Ollie Newland
December 11, 2025 AT 15:40As a pharmacist who’s seen three patients bleed out from INR spikes after ‘just trying CBD’ - let me tell you: this isn’t theoretical.
One guy thought ‘it’s just hemp oil’ - turned out his bottle had 18% THC and a lab report that looked like a toddler drew it.
He didn’t know CYP2C9 was his liver’s SWAT team.
Now he’s on a new warfarin regimen, wears a medical alert bracelet, and swears he’ll never touch another tincture without a blood test.
Don’t be him.
Check your meds. Ask your doc. Get a PT/INR if you’re on warfarin.
It’s not paranoia - it’s protocol.
Rebecca Braatz
December 12, 2025 AT 03:49Guys - I know this feels like a scary science lesson, but here’s the empowering part: YOU HAVE POWER HERE.
You can ask for blood tests. You can ask your doctor to check your meds’ metabolism. You can switch to CBG. You can start with 5mg and wait.
Knowledge isn’t just power - it’s peace of mind.
I used to think CBD was my magic bullet for chronic pain - until I realized I was just masking the real issue and risking my heart meds.
Now I’m working with a functional medicine doc, tracking my symptoms, and feeling better than ever - without the hidden dangers.
You can do this. You’re not alone. And your health is worth the effort.
Keep asking questions. Keep showing up. You’ve got this.
Michael Feldstein
December 13, 2025 AT 08:40One thing people miss: CBD’s half-life is long - up to 72 hours. So even if you take it every other day, your enzymes are still inhibited.
That’s why timing doses apart doesn’t fully solve it - the enzyme blockade is persistent.
Also - CYP3A4 inhibition isn’t just about sedation. It affects cholesterol meds, immunosuppressants, even some cancer drugs.
Bottom line: if your med has ‘CYP3A4’ in its metabolism profile, assume CBD is a wildcard.
And yes - I’ve seen people get away with it. But I’ve also seen the ones who didn’t.
Play it smart. Not lucky.
jagdish kumar
December 15, 2025 AT 08:33The truth is hidden in plain sight.
CBD is not the enemy.
The system is.
They made us dependent on pills. Then they sold us CBD as a ‘safe’ alternative - but only if we don’t question why the pills were needed in the first place.
It’s not about enzymes.
It’s about control.
Benjamin Sedler
December 16, 2025 AT 11:56So CBD inhibits enzymes - but what about the fact that every single prescription drug has a 30% failure rate in some populations?
Why are we blaming the supplement instead of the fact that medicine is basically a coin flip?
And why are we treating CBD like it’s the only thing that interacts with drugs?
My grandma takes grapefruit every morning and her blood pressure med. No one screams. But CBD? Oh no - it’s a public health crisis.
Double standard.
Also - I’ve been taking CBD with my antidepressant for two years. No issues. So your ‘science’ doesn’t apply to everyone.
Maybe stop fearmongering and start listening to real people?
zac grant
December 18, 2025 AT 09:27Let’s keep it real: if you’re on a medication with a narrow therapeutic index - warfarin, clobazam, cyclosporine - CBD is a risk you can’t afford to ignore.
But if you’re on metoprolol or omeprazole? The risk is low to moderate.
Most people won’t have issues - but the ones who do? They’re the ones who didn’t ask.
Don’t be the exception. Get your levels checked. Talk to your pharmacist. Use a reputable brand with a COA.
It’s not about fear. It’s about responsibility.
And yeah - CBG and CBDV look promising for the future. Less inhibition. More potential.
Stay curious. Stay cautious.
Carolyn Ford
December 19, 2025 AT 11:25Wow. Just… wow.
You people are so easily scared by a plant.
Let me guess - you also think sunlight causes cancer because of UV rays?
Or that water is dangerous because you can drown in it?
CBD inhibits enzymes? So does grapefruit. So does turmeric. So does green tea.
And yet - we’re not having a national panic about ‘turmeric and statin interactions.’
Why? Because Big Pharma doesn’t profit from turmeric.
This isn’t science.
This is corporate fear-mongering disguised as public health.
And you’re falling for it.
Wake up.
The real danger? Believing everything you read online.
Especially from people who get paid to scare you.
Martyn Stuart
December 21, 2025 AT 09:01Benjamin - your argument is a classic false equivalence.
Yes, grapefruit inhibits CYP3A4 - but we have clear warnings on grapefruit juice bottles.
We don’t have those on CBD products.
And grapefruit doesn’t contain 100+ other cannabinoids, terpenes, and contaminants - most of which are untested for drug interactions.
Also - turmeric’s curcumin inhibits CYP3A4 too - but at doses of 4–8 grams per day.
CBD? At 25mg. That’s 320x more potent on a per-milligram basis.
So no - this isn’t about corporate fear-mongering.
It’s about the fact that CBD is a potent, unregulated, pharmacologically active compound - and people are treating it like a vitamin.
And that’s dangerous.
Not because it’s evil.
Because it’s powerful.
And power without oversight? That’s not freedom.
That’s negligence.