PML Risk Calculator for Immunosuppressants
How to Use This Tool
Enter your specific treatment details below to estimate your risk of Progressive Multifocal Leukoencephalopathy (PML) from immunosuppressants. This tool is based on clinical data from the article. Remember: always discuss results with your healthcare provider.
Important: This calculator provides an estimate based on published data. It should not replace professional medical advice. PML risk is complex and influenced by multiple factors not captured here.
Imagine taking a medication that controls a serious disease like multiple sclerosis or Crohn’s - but it also quietly turns your own immune system against your brain. That’s the hidden danger of Progressive Multifocal Leukoencephalopathy (PML), a rare but deadly brain infection triggered by common immunosuppressants. It doesn’t happen often, but when it does, it changes everything - fast.
What Exactly Is PML?
PML isn’t a new disease. It was first described in 1958, but it’s only in the last 20 years that we’ve connected it clearly to modern drugs. At its core, PML is caused by the John Cunningham (JC) virus - a virus that lives quietly in about 50 to 70% of adults without causing harm. Your immune system keeps it locked down. But when powerful drugs suppress your immune response, that virus wakes up, attacks the cells that make the protective coating around your nerve fibers (oligodendrocytes), and destroys them. The result? Patchy, progressive damage across your brain.
The symptoms don’t come on suddenly like a stroke. They creep in: weakness on one side of your body, trouble speaking clearly, blurred vision, loss of coordination, or even personality changes. These are often mistaken for a flare-up of the original disease - like a multiple sclerosis relapse. That’s why PML is so dangerous. By the time it’s recognized, it’s often advanced.
Which Immunosuppressants Carry the Highest Risk?
Not all immunosuppressants are equal when it comes to PML risk. Some are far more dangerous than others. The drug with the strongest link is natalizumab (brand name Tysabri), used for multiple sclerosis and Crohn’s disease. Through 2011, over 82,000 people were treated with Tysabri worldwide. Of those, 102 developed PML - a rate of about 0.12%. But that number hides a much bigger risk for certain people.
If you’ve taken another immunosuppressant before - like azathioprine, methotrexate, or mitoxantrone - and you’re JC virus antibody positive, and you’ve been on natalizumab for more than two years? Your risk jumps to 4.1 cases per 1,000 patients. That’s more than 30 times higher than the average. The FDA and Cleveland Clinic both warn that prior immunosuppressant use is one of the biggest red flags.
Other high-risk drugs include:
- Fingolimod (Gilenya): 0.4 cases per 1,000 patient-years
- Dimethyl fumarate (Tecfidera): 0.2 cases per 1,000 patient-years
- Rituximab (Rituxan): 0.8 cases per 1,000 patient-years
- Ibrutinib (Imbruvica): 0.3% overall risk in blood cancer patients
Meanwhile, drugs like interferon beta and glatiramer acetate have never been linked to a single confirmed case of PML. That’s why many neurologists now recommend them as first-line options for patients with high PML risk factors.
How Is Risk Measured - and Why It’s Not Perfect
Doctors use one main tool to predict PML risk: the JC virus antibody test. If you’re positive, you’ve been exposed. If you’re negative, your risk is extremely low - but not zero. About 2 to 3% of people test negative even though they carry the virus. That’s the false-negative problem. One Reddit user, u/MSWarrior2023, described how their neurologist found early PML lesions on an MRI despite a negative JC test. That’s not rare. It’s a known gap.
Even more precise is the JC virus antibody index. This isn’t just a yes/no result - it measures how much antibody your body has made. An index above 1.5 means your risk of PML after 48 months on natalizumab is nearly 11%. Below 0.9? Less than 0.1%. That’s why many clinics now track this index every six months.
But here’s the catch: lymphopenia - low white blood cell count - also raises risk. A 2020 study found patients with lymphocyte counts under 0.8 x 10⁹/L had over four times higher risk of PML. Yet, most risk tools don’t include this. That’s a blind spot.
What Happens When PML Strikes - And How It’s Managed
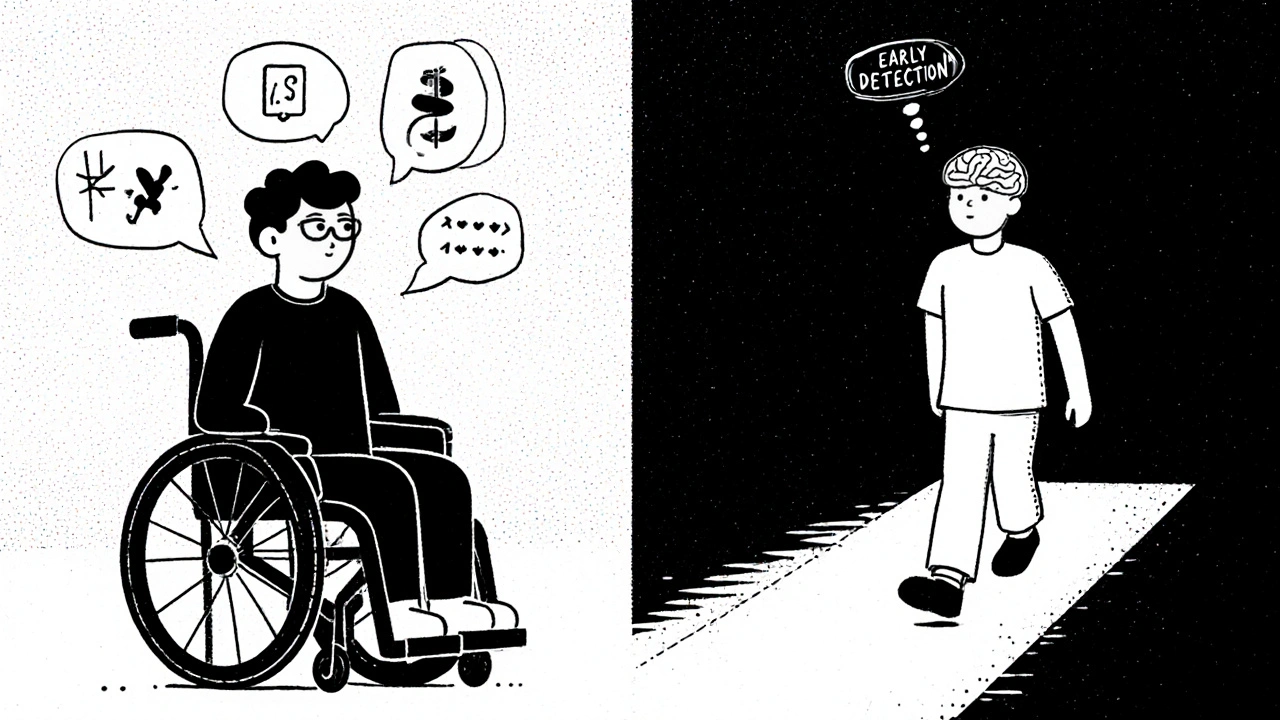
PML is fatal in 30 to 50% of cases. Survivors often live with permanent brain damage: paralysis, speech loss, vision problems. But early detection changes everything.
The key is regular brain MRIs. Every 3 to 6 months, patients on high-risk drugs should get a scan using diffusion-weighted imaging. This technique can spot PML lesions before symptoms appear. Neurologists need special training to tell these lesions apart from MS plaques - it takes 15 to 20 hours of focused learning. Not every clinic does this well. Community practices lag behind academic centers, where 92% have formal PML monitoring protocols.
If PML is caught early and the drug is stopped immediately, survival improves. But then comes another threat: immune reconstitution inflammatory syndrome (IRIS). In 50 to 60% of cases, when the immune system starts recovering, it attacks the damaged brain tissue - causing dangerous swelling. That’s treated with steroids like methylprednisolone. One patient, u/NatalizumabSurvivor, shared that stopping Tysabri at the first sign of symptoms and managing IRIS with steroids helped them regain 90% of their motor function after six months.
What Patients Are Really Feeling
Behind every statistic is a person living in fear. On the National Multiple Sclerosis Society’s forum, 78% of 214 respondents said they felt extreme anxiety about PML. More than half said they’d stop their medication after two years, even if it was working well. That’s the emotional cost of risk.
Some patients switch therapies entirely. Since 2015, prescriptions for natalizumab have dropped 22% in patients with prior immunosuppressant use. Meanwhile, drugs like ocrelizumab have grown in popularity - not because they’re perfect, but because their PML risk profile is much lower.
And yet, many patients still choose natalizumab. Why? Because for some, it’s the only thing that stops their MS from raging. The choice isn’t just medical - it’s deeply personal.
What’s Changing - And What’s Coming
The good news? Things are improving. In 2024, a new T-cell therapy called DIAVIS showed a 68% reduction in PML mortality in a small pilot study. Immune checkpoint inhibitors like pembrolizumab are also being tested - with promising results in a third of patients.
The Cleveland Clinic is now running a Phase II trial (NCT05678901) testing maraviroc, an HIV drug, to prevent PML in high-risk natalizumab patients. Early data suggests it may block the JC virus from entering brain cells.
By 2030, experts predict PML risk from natalizumab could drop to just 0.5 cases per 1,000 patient-years - thanks to better testing, smarter monitoring, and new treatments. That might bring it back as a first-line option for select patients.
What You Should Do Right Now
If you’re on an immunosuppressant - especially natalizumab, fingolimod, or rituximab - here’s what matters:
- Know your JC virus status. Get tested. If you’re positive, ask for the antibody index.
- Track your treatment time. Risk climbs after 24 months. Talk to your doctor about alternatives if you’re approaching that mark.
- Get regular MRIs. Ask if your clinic uses diffusion-weighted imaging. If not, push for it.
- Report even small changes. Slurred speech, blurry vision, new weakness - don’t wait. Call your neurologist immediately.
- Ask about your lymphocyte count. If it’s below 0.8 x 10⁹/L, your risk is higher than standard tools suggest.
PML is rare. But it’s real. And for those on high-risk drugs, awareness isn’t just helpful - it’s life-saving.
Can you get PML from any immunosuppressant?
No. PML is linked to specific drugs that strongly suppress cell-mediated immunity, especially monoclonal antibodies like natalizumab and rituximab, or oral agents like fingolimod. Common immunosuppressants like prednisone or low-dose methotrexate carry very low or no documented risk. The highest risk comes from drugs that target immune cells directly in the brain or bloodstream.
Is PML curable?
There’s no cure for PML, but early detection and stopping the triggering drug can lead to survival and recovery. About half of patients die, and many survivors have lasting neurological damage. New treatments like T-cell therapy and immune checkpoint inhibitors are showing promise in improving outcomes, but they’re still experimental.
How often should I get an MRI if I’m on natalizumab?
Most guidelines recommend a brain MRI every 3 to 6 months if you’re on natalizumab - especially if you’re JC virus positive or have taken prior immunosuppressants. The scan must include diffusion-weighted imaging to catch early PML lesions before symptoms appear. Don’t assume your regular MS MRI is enough - ask specifically for PML screening protocols.
Can a negative JC virus test be wrong?
Yes. About 2 to 3% of people who test negative for JC virus antibodies actually carry the virus. This is called a false-negative result. That’s why doctors also look at other risk factors - like prior immunosuppressant use, treatment duration, and lymphocyte count. Never rely on a single test to rule out PML risk.
Should I stop my medication if I’m worried about PML?
Don’t stop your medication without talking to your doctor. Stopping abruptly can cause your original disease to flare badly. Instead, ask for a full risk assessment: your JC virus status, antibody index, treatment time, lymphocyte count, and MRI history. Together, you can decide whether to continue, switch, or pause treatment - safely.
Are there alternatives to natalizumab with lower PML risk?
Yes. Drugs like interferon beta, glatiramer acetate, and teriflunomide have no confirmed PML cases. Ocrelizumab has a much lower risk than natalizumab - around 0.01 cases per 1,000 patient-years. Many patients switch to these options after 2 years on natalizumab, especially if they have prior immunosuppressant use. Your neurologist can help weigh disease control against PML risk.


Alex Grizzell
October 28, 2025 AT 07:05Just got my annual MRI and my neuro told me my JC index is 1.7. I’m on Tysabri for 30 months. I’m not panicking but I’m definitely thinking about switching. This post nailed it - awareness saves lives.
John Bob
October 28, 2025 AT 22:33Let’s be real - the FDA and pharma companies are hiding the real numbers. They want you scared enough to keep paying for MRIs and blood tests but not scared enough to stop taking the drug. PML isn’t rare - it’s just underreported. And don’t get me started on how they call it ‘rare’ when it’s 1 in 800 for some people. That’s not rare. That’s negligence.
Mickey Murray
October 29, 2025 AT 23:04My ex-wife had PML from Rituximab. She was 34. She’s in a wheelchair now. The doctors said ‘it’s rare’ - then they sent us the bill for $400k. You think you’re getting treatment? You’re gambling with your brain. And no, your neurologist doesn’t care as much as you think they do.
Tiffanie Doyle
October 31, 2025 AT 08:28OMG this is so important!! I just got my JC test back and I’m positive 😳 I’ve been on Tecfidera for 18 months. I’m gonna ask for an index next visit. Thank you for sharing this!! 💪❤️
james landon
November 2, 2025 AT 07:20Bro I’ve been on Gilenya for 4 years and I’m fine. Why are we acting like this is a death sentence? My cousin had MS and just went on steroids and now he’s hiking in Colorado. Stop scaring people.
Rodrigo Ferguson
November 2, 2025 AT 15:21One must interrogate the epistemological foundations of the so-called ‘PML risk stratification.’ The JC antibody index is a proxy variable derived from serological assays with known false-negative rates, yet it is treated as an ontological truth by clinical institutions. Moreover, the conflation of lymphopenia as a secondary variable - rather than a primary biomarker - represents a fundamental failure of medical reductionism. One must question: Who benefits from this incomplete risk model? The pharmaceutical-industrial complex, naturally.
George Johnson
November 3, 2025 AT 23:47So let me get this straight - we’re supposed to get an MRI every 3 months, check our white blood cells, track our antibody index, and still pray to the medical gods that we don’t turn into a human pincushion? And if we do? Well, at least we got a fancy MRI report before we lost our speech. Classic.
Jenn Clark
November 5, 2025 AT 22:35I’ve been on interferon beta for 6 years and I’ve never had a relapse. I wish I’d known about the low-risk options earlier. It’s not glamorous, but it’s safe. And that’s worth something.
giri pranata
November 7, 2025 AT 03:15From India - we don’t have access to most of these tests or drugs. But I read this and shared it with my cousin in the US. She’s on Tysabri. Now she’s asking for her index. Small things matter. Thanks for writing this.
L Walker
November 7, 2025 AT 14:42Interesting. But you didn’t mention the 2023 meta-analysis from Lancet Neurology that showed a 3.1% PML incidence in patients with prior mitoxantrone exposure - even without JC+ status. The data’s there. It’s just not in the FDA’s marketing materials.
Also - your list of ‘low-risk’ drugs omits dimethyl fumarate’s association with PML in patients with prolonged lymphopenia. That’s a critical omission.