G6PD Medication Safety Checker
Check if a medication is safe for people with G6PD deficiency. Enter the name of a drug below to see if it's known to cause hemolysis.
When you have G6PD deficiency, even a common medication can trigger a dangerous drop in red blood cells. This isn’t a rare condition-it affects about 400 million people worldwide. In some places, like parts of Africa, the Mediterranean, and Southeast Asia, as many as 1 in 5 people carry the gene. The problem isn’t the deficiency itself. It’s what happens when you take certain drugs. One wrong pill can send your hemoglobin crashing-sometimes in under 48 hours. You could end up in the hospital needing blood transfusions. But here’s the good news: hemolysis prevention is almost always possible-if you know what to avoid and how to act.
What Happens When G6PD Deficiency Meets the Wrong Drug
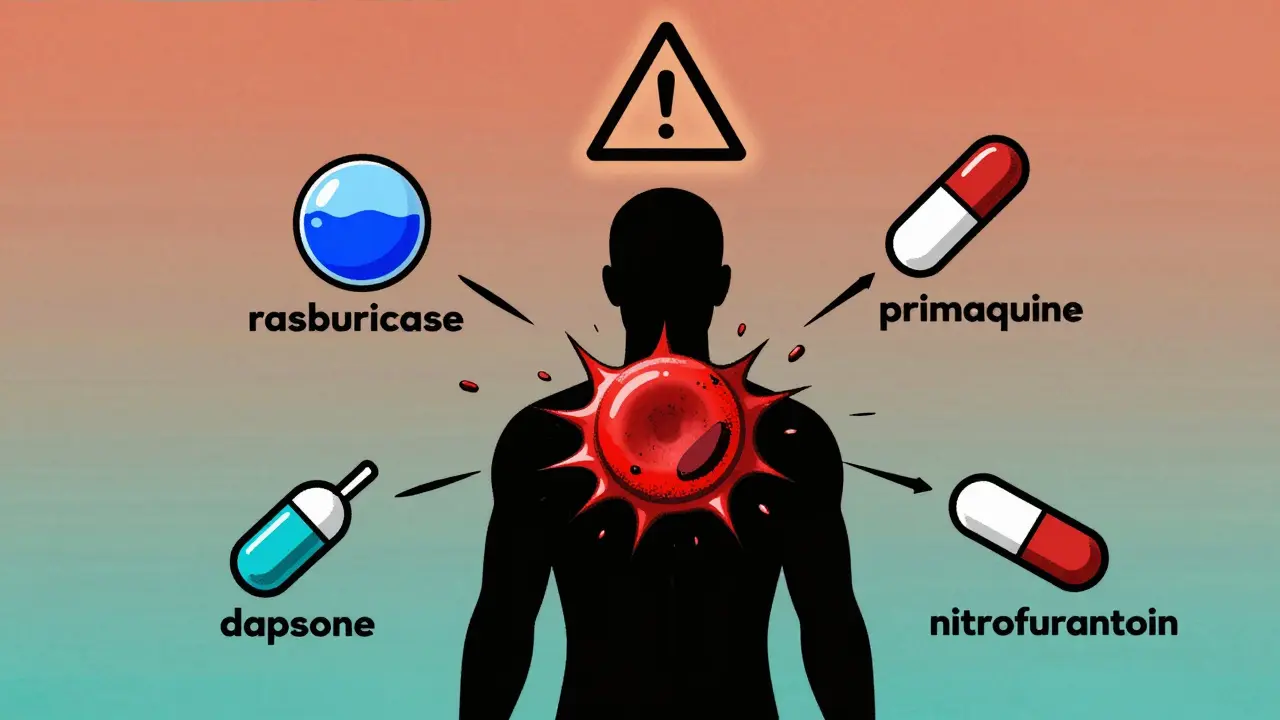
Your red blood cells need protection from everyday oxidative stress. Glucose-6-phosphate dehydrogenase (G6PD) is the enzyme that keeps that protection active. Without enough of it, your cells can’t fight off damage from certain chemicals. When you take a medication that causes oxidative stress, your red blood cells start breaking apart. That’s hemolysis. It doesn’t happen slowly. It can hit fast and hard. A person with severe G6PD deficiency might see their hemoglobin drop from 14 g/dL to under 6 g/dL in less than a week after taking a trigger drug. Symptoms include dark urine, extreme fatigue, yellowing skin, shortness of breath, and rapid heartbeat. In extreme cases, kidney failure or death can follow. The risk isn’t theoretical. In 2021, a 28-year-old man in the U.S. received rasburicase for tumor lysis syndrome without being tested for G6PD deficiency. His hemoglobin fell to 3.1 g/dL. He needed 10 units of blood over three days.The 5 Medications That Are Most Dangerous
Not all drugs are risky. But some are deadly for people with G6PD deficiency. These five are the biggest threats:- Rasburicase: Used to treat tumor lysis syndrome. The FDA issued a Black Box Warning in January 2023 because it causes hemolysis in 100% of G6PD-deficient patients. There is no safe dose. Always test before use.
- Methylene blue: Given for methemoglobinemia. It causes severe hemolysis in 95% of deficient patients. Even small doses can be catastrophic. Alternative treatments like ascorbic acid exist.
- Primaquine: Used to kill dormant malaria parasites. It triggers hemolysis in 100% of Class I and II G6PD patients. WHO updated its guidelines in 2023 to require testing before any dose.
- Dapsone: Used for leprosy and some skin conditions. At doses above 50 mg daily, it causes hemolysis in 80% of people with G6PD deficiency. Lower doses may be tolerated-but only under strict monitoring.
- Nitrofurantoin: A common antibiotic for UTIs. While not always listed as high-risk, it’s been linked to hemolytic episodes in multiple case reports since 2020. Avoid unless no alternatives exist.
These aren’t just warnings on labels. These are real, documented emergencies. A nurse in Ohio posted on Reddit in July 2023 about giving methylene blue to a patient who hadn’t been tested. Hemoglobin dropped from 14.2 to 5.8 in 48 hours. Three units of blood were needed.
Safe Alternatives You Can Actually Use
You don’t have to live in fear. Many common medications are completely safe. Here’s what you can use instead:- Chloroquine: For malaria prevention. Safe in all G6PD deficiency classes. Used by WHO for decades.
- Tafenoquine: A newer drug for radical cure of malaria. Approved in 2018, but only if G6PD testing is done first. It’s effective-but not without a test.
- Artemisinin-based combination therapies (ACTs): The gold standard for treating malaria today. Safe for all G6PD levels.
- Atovaquone-proguanil (Malarone): Recommended by the CDC for travelers with G6PD deficiency. 95% of deficient travelers using this avoided hemolysis in a 2021 study.
- Penicillins, cephalosporins, and macrolides: Common antibiotics like amoxicillin, cephalexin, and azithromycin are all safe. No need to avoid them.
Many people think they have to avoid all antibiotics or painkillers. That’s not true. Acetaminophen (paracetamol) is safe. Ibuprofen is safe. Aspirin is generally safe in low doses. The danger lies in specific oxidative agents-not all drugs.

Testing: When and How It Matters
The biggest mistake? Waiting until after a crisis to test. Once hemolysis starts, your enzyme levels drop. Testing during or right after an episode gives false negatives. You need to wait at least three months for accurate results. The best time to test is before any new medication is prescribed-or at birth. In regions with high G6PD prevalence, newborn screening is now standard. The fluorescent spot test gives results in 15 minutes, with 98.7% accuracy. It’s cheap, fast, and reliable. In the U.S., only 12 states require newborn G6PD testing. But if you’re of African, Mediterranean, or Southeast Asian descent, ask for it. Even if you’re asymptomatic, you could be carrying the gene. And if you’re a woman, don’t assume you’re safe. About 15% of female carriers experience hemolysis due to X-chromosome inactivation patterns.What Your Doctor Might Not Tell You
Many doctors don’t know the full list of risky drugs. A 2022 survey of 1,247 G6PD-deficient patients found that 68% had at least one hemolytic episode-and 42% said their providers didn’t know the restrictions. Some drug labels list warnings based on tiny amounts of evidence. For example, sulfonylureas like glyburide (used for diabetes) carry G6PD warnings in 92% of global package inserts. But there are only 17 documented cases since 1965. That doesn’t mean they’re safe-but it means the risk is likely low. Still, if you’re unsure, ask for alternatives. The University of California San Francisco built a system that flags high-risk drugs in electronic health records. When a doctor tries to prescribe primaquine to a G6PD-deficient patient, the system auto-suggests chloroquine instead. In a 12-month pilot, inappropriate prescribing dropped by 89%.
What You Can Do Right Now
If you’ve never been tested:- Ask your doctor for a G6PD test-especially if you’re from a high-prevalence region or have unexplained anemia.
- Get your results in writing. Save them in your phone and wallet.
- Make a list of safe and unsafe medications. Keep it updated.
- Wear a medical alert bracelet that says “G6PD Deficiency.”
- Before any new prescription, ask: “Is this safe for someone with G6PD deficiency?”
If you’ve had a hemolytic episode:
- Wait at least three months before getting tested again.
- Review every medication you’ve taken in the past year. Cross-reference with the WHO’s 2024 Essential Medicines List.
- Ask your pharmacist to run a G6PD safety check on your entire medication list.
There’s no cure for G6PD deficiency. But you don’t need one. Prevention works. In Thailand, after hospitals made G6PD testing mandatory before giving primaquine, hemolytic crises dropped from 15.2% to 0.3%. In Saudi Arabia, universal newborn screening cut hospital admissions by 78%.
You’re not helpless. You just need to be informed. And now you are.
What’s Coming Next
The future looks better. In January 2024, the FDA approved the first point-of-care G6PD test that gives results in 8 minutes. That’s a game-changer for emergency rooms and clinics without labs. Researchers are also testing N-acetylcysteine (NAC) as a protective agent. Early studies show it reduces hemolysis by 75% when given with primaquine. Phase I trials for enzyme replacement therapy are set to begin in late 2024. The goal isn’t just to avoid death. It’s to make G6PD deficiency a non-issue. By 2035, experts believe preventable deaths from this condition could be eliminated in places with good healthcare access.Can G6PD deficiency be cured?
No, G6PD deficiency cannot be cured. It’s a genetic condition. But it doesn’t need to be. With proper medication avoidance and testing, people with G6PD deficiency live normal, healthy lives. Prevention, not cure, is the key.
Is G6PD deficiency only a problem for men?
No. While it’s more common in men because the gene is on the X chromosome, women can be affected too. About 15% of female carriers experience hemolysis due to random X-chromosome inactivation. Never assume you’re safe just because you’re female.
Can I take vitamin C or other supplements?
Yes. Vitamin C (ascorbic acid) is safe and even helpful. It’s used as an alternative to methylene blue for treating methemoglobinemia in G6PD-deficient patients. Most common supplements like vitamin D, B-complex, and magnesium are also safe. Avoid high-dose synthetic antioxidants unless approved by your doctor.
What should I do if I accidentally take a risky medication?
Stop the medication immediately. Seek medical help right away. Symptoms like dark urine, extreme fatigue, or rapid heartbeat mean you may be having hemolysis. Blood tests will check your hemoglobin and reticulocyte count. Early treatment can prevent kidney damage or worse.
Are there any foods I need to avoid?
Yes. Fava beans (broad beans) are a well-known trigger. Eating them-even in small amounts-can cause hemolysis in some people with G6PD deficiency, especially those with Mediterranean variants. Also avoid tonic water (contains quinine) and naphthalene (mothballs). Most other foods are safe.



Donny Airlangga
January 9, 2026 AT 02:40This is the kind of post that saves lives. I work in ER and saw a guy come in with hemoglobin at 3.8 after getting rasburicase. No one checked his G6PD status. He didn’t even know what it was. This needs to be in every medical school curriculum.
Thank you for laying this out so clearly.
Prakash Sharma
January 10, 2026 AT 19:02India needs to make G6PD testing mandatory at birth. We’ve got millions of carriers here and doctors still prescribe primaquine like it’s aspirin. My cousin died in 2019 because a rural clinic gave him primaquine for ‘malaria symptoms’ without testing. No one even knew what G6PD stood for.
This isn’t just medical-it’s a social justice issue.
swati Thounaojam
January 10, 2026 AT 20:30just got tested last year. never knew i had it. now i have a note on my phone. saved my life already when my doc tried to prescribe nitrofurantoin.
Aubrey Mallory
January 12, 2026 AT 17:36As a nurse who’s seen this firsthand, I’m furious that this isn’t standard protocol everywhere. We had a patient in ICU last month-same story. Methylene blue, no test, hemoglobin dropped in 36 hours. We gave her three units. She’s fine now, but she shouldn’t have ever gotten that drug in the first place.
Doctors need to stop assuming. Test first. Always.
Dave Old-Wolf
January 13, 2026 AT 11:49Wait so if I’m from the US and my grandma was from Nigeria, should I get tested even if I’ve never had symptoms?
My mom says I’ve always been pale but never thought much of it. Is this something I should ask my doctor about tomorrow?
Molly Silvernale
January 14, 2026 AT 09:25It’s eerie, isn’t it?-how a single enzyme, invisible, silent, can be the difference between life and a transfusion cart rolling down the hallway at 3 a.m. We think of medicine as control, as mastery-but here, it’s humility. A genetic whisper, a biochemical ghost, and a doctor who didn’t ask the right question.
Prevention isn’t just clinical-it’s sacred. And yet, we still treat it like an afterthought.
Maybe the real cure isn’t in labs. Maybe it’s in listening.
And remembering that someone’s ancestor survived malaria… so their blood could one day betray them.
Ken Porter
January 15, 2026 AT 17:55Why is this even a thing? If you’re gonna have a genetic disorder, why not just get rid of it? We’ve got CRISPR. Why are we still playing Russian roulette with antibiotics?
Manish Kumar
January 16, 2026 AT 11:19Let’s be real-G6PD deficiency isn’t a disease. It’s an evolutionary adaptation. The same gene that makes you vulnerable to drugs also protects you from malaria. That’s why it’s so common in Africa, South Asia, the Mediterranean. It’s not a flaw-it’s a shield.
But modern medicine? We’ve lost the context. We see a defect. We don’t see the survival story written in your DNA.
So yes, avoid the drugs. But also honor the fact that your ancestors outlived plagues because of this. You’re not broken. You’re battle-tested.
And if your doctor doesn’t get that? Find a new one.
Also, fava beans are a trap. Don’t eat them. Even if you think you’re fine. I ate them once in 2017. Woke up with tea-colored urine. Took three days to recover. Don’t be like me.
Kristina Felixita
January 17, 2026 AT 07:28As a mom of two kids with G6PD, I want to say thank you for this. We live in a small town in Ohio. No one here knows what it is. I carry a printed list of safe/unsafe meds in my purse. My kids wear medical bracelets. We’ve had to argue with pharmacists who said 'it's just a minor thing.'
It's not minor. It's life or death.
Also-yes, vitamin C is safe. I give mine daily. And no, I don't use any supplements with 'antioxidant' on the label unless I've checked them myself. I’ve learned the hard way.
Keep sharing this. We need more voices like yours.
Joanna Brancewicz
January 17, 2026 AT 14:12Primaquine-induced hemolysis is a Class 1 adverse event with high morbidity. The pharmacokinetic profile of the drug in G6PD-deficient individuals results in unmitigated oxidative stress on erythrocyte membranes, leading to intravascular hemolysis and potential acute kidney injury secondary to hemoglobinuria.
Standard of care requires genotypic or phenotypic confirmation prior to administration. Failure to comply constitutes a breach of duty.
Evan Smith
January 19, 2026 AT 03:16So let me get this straight… we’ve got a test that takes 15 minutes, costs like $5, and prevents hospitalizations… but we still let people get poisoned because someone forgot to check?
Someone’s getting fired. Or at least should be.
Also, can we make this a tattoo? ‘G6PD Deficient - NO PRIMAQUINE, NO METHYLENE BLUE’? I’d get it.
Lois Li
January 20, 2026 AT 11:21My daughter was diagnosed at birth in California. We’re lucky. But I’ve seen parents in online groups panic because their doctor told them ‘it’s not a big deal.’ It is. It’s a big deal. I keep a laminated card in my wallet with the safe meds list. I’ve emailed it to every pediatrician, pharmacist, and ER nurse I’ve ever met.
We’re not asking for special treatment. We’re asking for basic respect. Please, if you’re a provider-ask the question. Even if it’s awkward. Even if they’re white. Even if they’re from Nebraska.
It could save a life.