When your feet feel like they’re wrapped in sandpaper, or your hands buzz with a constant electric sting, it’s not just discomfort-it’s peripheral neuropathy. This isn’t a single disease, but a symptom of nerve damage that affects over 20 million people in the U.S. alone. For many, it starts quietly-a tingling in the toes, a numbness that doesn’t go away. But left unchecked, it can lead to falls, sleepless nights, and the slow loss of independence. The good news? We know more now than ever about what causes it, how to slow it down, and how to manage the pain-without relying on risky opioids.
What Exactly Is Peripheral Neuropathy?
Peripheral nerves are your body’s wiring. They stretch from your spinal cord to your fingers, toes, and organs, sending signals for movement, touch, and temperature. When these nerves get damaged, the messages get scrambled. You might feel pain where there’s no injury, or lose sensation entirely-like walking barefoot on hot pavement without realizing it.
This isn’t rare. In fact, it’s one of the most common neurological conditions. About 75% of cases are polyneuropathy, meaning damage across many nerves, usually symmetrically in the hands and feet. The rest are mononeuropathy (one nerve affected, like carpal tunnel) or multiple mononeuropathies. Symptoms typically start in the feet and creep upward. People describe it as burning, stabbing, or a deep ache that won’t quit.
The Top Causes You Can’t Ignore
Not all nerve damage is the same. The cause changes everything about how you treat it.
- Diabetes is the biggest culprit-responsible for about 30% of all cases. Half of all people with diabetes will develop some level of nerve damage over time. High blood sugar slowly poisons the nerves and cuts off their blood supply. The Diabetes Control and Complications Trial proved that keeping HbA1c below 7% reduces nerve damage progression by 60%.
- Vitamin B12 deficiency affects roughly 8% of cases. This is often overlooked. Older adults, vegans, and people on long-term acid reflux meds are at higher risk. Simple blood tests can catch this early.
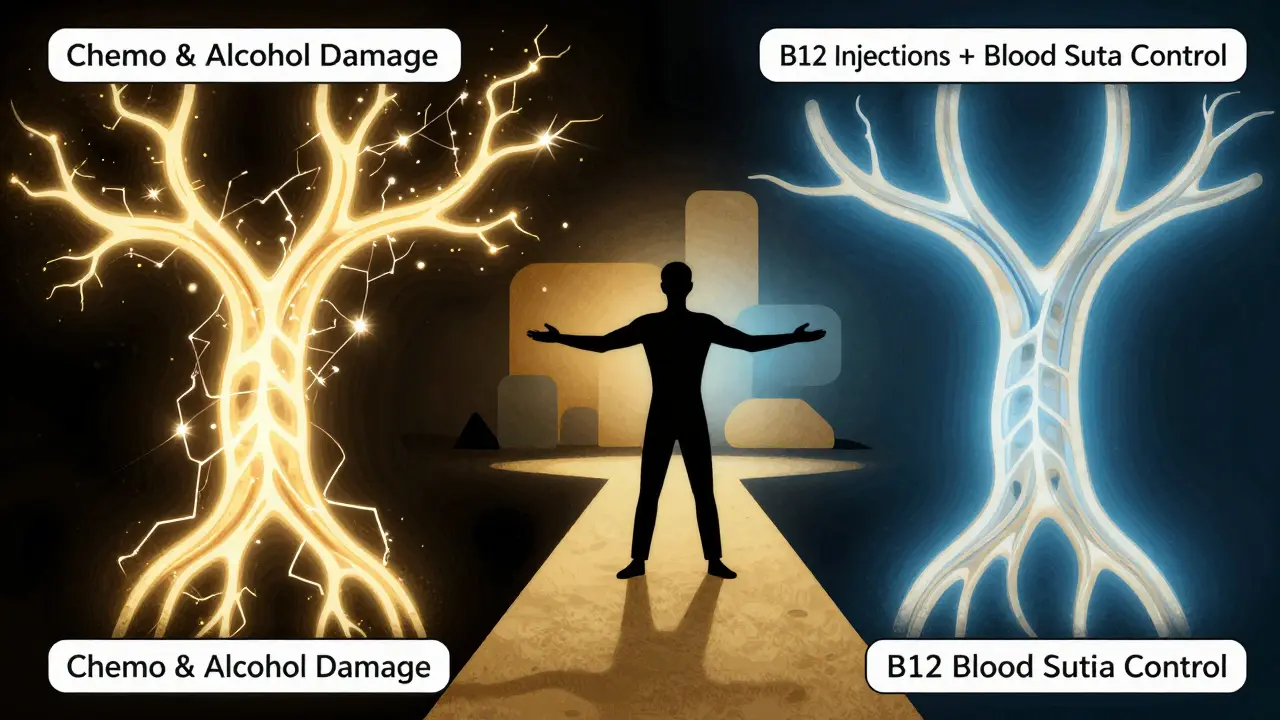
- Chemotherapy causes neuropathy in 30-40% of cancer patients using drugs like vincristine or paclitaxel. It’s called “chemo brain” for the nerves-your hands and feet go numb, sometimes permanently.
- Alcohol abuse damages nerves directly and often goes hand-in-hand with poor nutrition, worsening B12 and thiamine deficiencies.
- Autoimmune diseases like Guillain-Barré or lupus can attack the nervous system. Infections like Lyme disease or shingles can also trigger nerve inflammation.
- Idiopathic means “no known cause.” About 20% of cases fall into this category. Even after full testing, doctors can’t pinpoint why the nerves are damaged.
It’s critical to find the root cause. Treating the pain alone only fixes half the problem. If diabetes is the driver, you need blood sugar control. If it’s B12, you need injections-not painkillers.
How Pain Management Really Works (Not What You Think)
Most people reach for ibuprofen or acetaminophen first. But those won’t help much. Neuropathic pain doesn’t respond to regular painkillers. It needs targeted treatments.
Here’s what actually works, backed by clinical data:
- Pregabalin (Lyrica): Reduces pain by 50% in about 37% of users. Dose: 150-600 mg daily. Side effects? Dizziness, weight gain, brain fog. Many stop after the first few weeks.
- Duloxetine (Cymbalta): An antidepressant that works for nerve pain. 35% of users get 50% pain relief. Common side effects: nausea, fatigue, dry mouth. It can help if depression or anxiety is also present.
- Amitriptyline: An old-school tricyclic antidepressant. It gives 50% pain relief to 41% of patients. But 75% report dry mouth, and 60% feel drowsy. It’s cheap, but tough to tolerate.
- Scrambler therapy: A non-drug option. Electrodes send “non-pain” signals to the brain, overriding the pain. Mayo Clinic data shows 85% of patients got 50% pain reduction after 10 sessions. No side effects. Cost: $1,200-$1,500 per full course.
- Spinal cord stimulation: For severe, unresponsive cases. A small device implanted near the spine interrupts pain signals. 65% of patients report half the pain gone. Used when everything else fails.
Here’s the reality: Medications work for some, not all. And side effects are often worse than the pain. That’s why many patients stop taking them within 3 months. The American Academy of Neurology lists pregabalin and duloxetine as first-line options-but they’re not magic bullets.
Non-Medication Strategies That Actually Help
You don’t need a prescription to improve your quality of life.
- Physical therapy: Focuses on balance, strength, and gait. After 12 weeks of targeted exercises, patients improve their “timed up and go” test by 25%. That means fewer falls. One study showed a 30% drop in fall risk.
- Custom orthotics: If your feet are numb, you can’t feel if your shoe is too tight or has a pebble inside. Therapeutic shoes and custom inserts reduce pressure points and prevent ulcers. 82% of users report high satisfaction.
- Foot care: Check your feet twice a day. Look for cuts, blisters, redness. Wash and dry thoroughly. Never go barefoot. Diabetics who do this reduce foot ulcer risk by 85%.
- Scrambler therapy: Already mentioned, but worth repeating-it’s one of the few treatments with near-zero side effects and high success rates.
- Qutenza patch: FDA-approved in 2020. A high-dose capsaicin patch applied once every 3 months. One 30-minute session can reduce pain for months. Works best for foot pain.
These aren’t “alternative” ideas-they’re standard care. Many patients who avoid drugs entirely do better long-term because they focus on prevention and daily habits.
What Doesn’t Work (And Why You Should Avoid It)
There’s a lot of noise out there.
- Opioids: They help only 30% of neuropathic pain cases and carry a 15% addiction risk over time. The American Diabetes Association and Harvard Health both warn against them. They don’t fix the nerve damage-just mask the pain, often dangerously.
- Over-the-counter pain relievers: Ibuprofen or Tylenol? They reduce pain by only 10-15% in neuropathy. Not worth the stomach or liver risk.
- Unregulated supplements: “Nerve support” blends with alpha-lipoic acid or B vitamins? Some may help if you’re deficient. But if you’re not, they do nothing. And they’re not regulated. Stick to doctor-approved doses.
The key is this: Don’t treat the symptom without treating the cause. If you have diabetes, control your blood sugar. If you’re low on B12, get injections. Everything else is just band-aiding.
What’s New in 2026?
The field is moving fast.
- Genomics project: Launched in January 2023, the Neuropathy Genomics Project aims to identify genetic markers for over 50 types of nerve damage by 2026. This could lead to personalized treatments.
- Gene therapy: Early trials for Charcot-Marie-Tooth disease show 20% improvement in nerve signal speed after 6 months. Still experimental, but promising.
- Wearable nerve stimulators: Devices in development (expected FDA submission in Q2 2024) aim to deliver gentle electrical pulses through the skin, offering continuous relief. Early trials show 40% pain reduction.
- AI diagnostics: Tools trained on nerve conduction data could cut diagnosis time from 18 months to under 6 months by 2025. That’s huge-because early treatment improves outcomes by 40%.
These aren’t sci-fi. They’re real, and they’re coming. But for now, the best tools are still the ones we’ve had for years: blood sugar control, B12 checks, physical therapy, and smart pain management.
Real Talk: What Patients Actually Say
Reddit’s r/neuropathy has 12,500 members. Their stories are raw:
- “Lyrica cut my foot pain from 8/10 to 3/10-but I couldn’t drive for weeks. Worth it?” - u/SarahJ72, June 2023
- “Cymbalta helped the pain but made me sick. My doctor didn’t warn me. I quit after 2 weeks.” - u/DaveM45, August 2023
- “I got custom shoes. Changed my life. No more blisters. No more fear of walking.” - Anonymous, Healthgrades review
One theme repeats: people feel dismissed. It takes an average of 18 months to get diagnosed. Doctors often mistake it for arthritis or aging. But the data doesn’t lie: early intervention saves mobility.
Final Thoughts: It’s Manageable, Not Inevitable
Peripheral neuropathy doesn’t have to mean a life of pain and isolation. For diabetics, tight glucose control is the single most powerful tool. For others, identifying the cause-whether it’s B12, alcohol, or an autoimmune trigger-is step one.
There’s no cure yet. But there are proven ways to slow it, manage it, and live well with it. You don’t need to suffer silently. Talk to your doctor about nerve testing. Ask about physical therapy. Explore non-drug options. And above all-don’t wait. The first six months after symptoms start are the most critical.
Can peripheral neuropathy be reversed?
In some cases, yes-if the cause is treatable. For example, nerve damage from vitamin B12 deficiency often improves within 4-8 weeks of injections. Diabetic neuropathy can stabilize if blood sugar stays below 7% HbA1c for years. But once nerve fibers are destroyed, they don’t fully regrow. The goal is to stop progression and manage symptoms.
Is peripheral neuropathy only caused by diabetes?
No. While diabetes is the most common cause-accounting for about 30% of cases-there are over 100 known causes. These include vitamin deficiencies, alcohol abuse, chemotherapy, autoimmune diseases, infections like Lyme or shingles, and inherited conditions. About 20% of cases have no identifiable cause (idiopathic).
Why do over-the-counter painkillers not work for neuropathy?
Neuropathic pain isn’t caused by inflammation or tissue injury-it’s caused by misfiring nerves. Drugs like ibuprofen or Tylenol target inflammation and general pain, but they don’t calm overactive nerve signals. That’s why medications like pregabalin or duloxetine, which target nerve activity, are far more effective.
How long does it take to see improvement from treatment?
It depends on the cause. For B12 deficiency, improvement can happen in 4-8 weeks. With diabetes, it takes 3-6 months of stable blood sugar to see nerve symptoms improve. Medications like pregabalin may help in weeks, but physical therapy and lifestyle changes often take 8-12 weeks to show clear results.
Can I prevent peripheral neuropathy if I have diabetes?
Yes, significantly. Keeping HbA1c below 7% for at least 5 years reduces the risk of developing neuropathy by 60%. Daily foot checks, avoiding alcohol, managing blood pressure, and staying active also help. Early, consistent control is the best prevention.