When eye pressure stays too high for too long, it can quietly damage the optic nerve - and that’s glaucoma. Medications and laser treatments help many people, but for others, surgery becomes the next step. Two main paths exist: the classic trabeculectomy and the newer, less invasive MIGS procedures. Each has clear strengths, risks, and best-use cases. Understanding the differences isn’t just about medical jargon - it’s about choosing the right path to protect your vision.
What Trabeculectomy Really Does
Trabeculectomy isn’t new. It was developed in the 1960s and remains the most reliable way to drop eye pressure significantly. The surgery creates a tiny channel under the white part of the eye (sclera), allowing fluid to drain out and form a small blister-like pocket (a bleb) under the eyelid. This bleb acts like a pressure valve, helping the eye stay at a safer pressure level.Typically, this surgery lowers pressure by 30% to 50%. In 85% to 90% of cases, patients reach their target pressure within the first year. That’s why it’s still the go-to for advanced glaucoma, especially when pressure needs to be kept below 15 mmHg. It’s also the choice for younger patients who need long-term control.
But it’s not simple. The procedure takes about an hour. Afterward, recovery is slow and demanding. You’ll need weekly checkups for months. The bleb can leak, scar over, or get infected. About 10% to 15% of patients experience a leak in the first few weeks. A rare but serious risk is endophthalmitis - an infection inside the eye - which happens in 0.5% to 2% of cases long-term. If the bleb fails, you might need another surgery. That’s why it’s not the first option anymore.
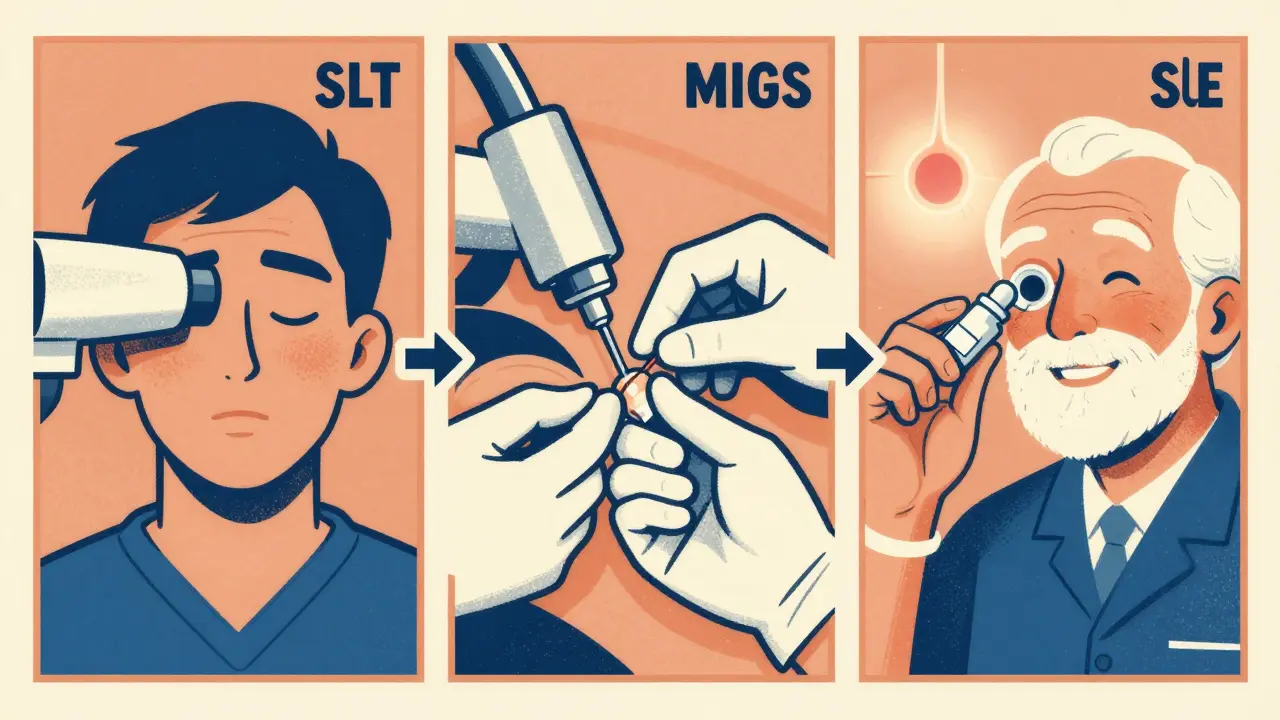
How MIGS Changed the Game
Minimally Invasive Glaucoma Surgery (MIGS) started gaining traction around 2012 with the FDA approval of the iStent. Since then, dozens of new devices have come out. These procedures use tiny incisions - often less than 1.5 millimeters - and are designed to be safer and faster.MIGS doesn’t aim to drop pressure as low as trabeculectomy. Instead, it typically lowers pressure by 20% to 30%. That’s enough for many people with mild to moderate glaucoma, especially if their target pressure is 15-18 mmHg. The real win? Most MIGS procedures are done at the same time as cataract surgery. So if you’re already having cataracts removed, you can tackle both problems in one go.
Common MIGS devices include:
- iStent inject: Two tiny stents placed in the eye’s natural drainage system. Lowers pressure by 25%-30%.
- Hydrus Microstent: A small scaffold that opens up the drainage channel. Works well with cataract surgery.
- Xen Gel Stent: A soft, 6mm tube that drains fluid to the surface of the eye. More effective than other MIGS but still safer than trabeculectomy.
- GATT (Gonioscopy-Assisted Transluminal Trabeculotomy): A thread is threaded through the drainage system to open it up. Can reduce pressure by 30%-35%.
Complication rates for MIGS are under 5%. Most patients are back to normal activities in just 1-2 weeks. No bleb means no risk of infection from a leak. No long-term monitoring either - follow-ups usually end after 1-2 months.
Cost and Accessibility
Cost varies widely. Trabeculectomy averages around $4,200 per eye. MIGS procedures cost more upfront - Xen stents run about $6,300. Tube shunts (another type of traditional surgery) range from $5,000 to $7,500. Why the difference? MIGS devices are high-tech implants with proprietary designs. Insurance usually covers them, but out-of-pocket costs can vary depending on your plan and where you live.Access to MIGS has grown fast. In the U.S., about 65% of standalone glaucoma surgeries now use MIGS. That’s up from under 10% just a decade ago. The trend is clear: doctors are moving these procedures earlier in the treatment plan.
Where Laser Fits In
Before surgery, most patients try laser treatment. Selective Laser Trabeculoplasty (SLT) is now the first-line option for open-angle glaucoma. It’s quick - takes 5 to 10 minutes - and has no downtime. SLT uses a laser to gently stimulate the drainage system, improving fluid outflow. The 2023 LiGHT trial showed SLT was just as effective as daily eye drops at controlling pressure over three years. About 75% of patients maintained safe pressure without needing more treatment.SLT can be repeated if pressure rises again. It’s safe, cheap, and non-invasive. That’s why many doctors now recommend SLT before even thinking about MIGS or trabeculectomy.
Choosing the Right Path
There’s no one-size-fits-all. Your best option depends on three things: how advanced your glaucoma is, your target pressure, and your overall health.- Early-stage glaucoma: Start with SLT. If that wears off, try a MIGS procedure - especially if you’re having cataract surgery too.
- Moderate glaucoma: MIGS is often ideal. It reduces medications (on average, 1.5 to 2 fewer eye drops) and avoids major surgery risks.
- Advanced glaucoma: Trabeculectomy or a tube shunt is usually needed. You need pressure below 15 mmHg, and MIGS won’t get you there.
- Failed MIGS: Trabeculectomy remains the next step.
Recovery time matters too. If you’re active, work with your hands, or can’t take weeks off, MIGS is a better fit. If you’re older and have other eye conditions, trabeculectomy might offer more lasting results.
What the Experts Say
Dr. Joel Schuman, chair of ophthalmology at NYU Langone, says: “For most open-angle glaucoma, SLT is the first thing I reach for.” He points to the LiGHT trial data - the evidence is strong. But he also acknowledges trabeculectomy still has a place. “It’s the gold standard for patients who need very low pressure,” he says.Mass Eye and Ear, which performed over 400 glaucoma surgeries in 2023, agrees. They see MIGS as a fast-growing field, but they still rely on trabeculectomy for advanced cases. The key takeaway? The treatment pathway is changing. We’re not waiting until the last resort anymore.
What’s Next?
New developments are already here. Direct Selective Laser Trabeculoplasty (DSLT) treats the entire drainage system automatically, without touching the eye. It’s slightly less effective than traditional SLT but easier to perform. Suprachoroidal shunts - devices placed behind the eye - are being tested as standalone options. These aren’t mainstream yet, but they show where the field is heading: more precision, less trauma, earlier intervention.The bottom line: Glaucoma surgery isn’t about picking the most advanced tech. It’s about matching the tool to the problem. SLT first. MIGS for moderate cases. Trabeculectomy for the tough ones. And always, always - monitor pressure. Because once vision is lost, it can’t be brought back.
Is MIGS better than trabeculectomy?
It depends. MIGS is safer, has faster recovery, and is ideal for mild-to-moderate glaucoma. But it doesn’t lower pressure as much. Trabeculectomy drops pressure more - often below 15 mmHg - which is critical for advanced cases. So MIGS wins on safety; trabeculectomy wins on power. The right choice depends on your pressure goals and disease stage.
Can I avoid surgery altogether?
Yes, for many people. SLT (selective laser trabeculoplasty) is now the first-line treatment for open-angle glaucoma. It’s non-invasive, takes minutes, and works as well as eye drops. About 75% of patients maintain safe pressure for at least three years. If SLT wears off, MIGS is often the next step - not full surgery.
How long does recovery take after glaucoma surgery?
For MIGS, most people return to normal activities in 1-2 weeks. For trabeculectomy, expect 4-6 weeks of restrictions - no heavy lifting, no bending over, no eye rubbing. Follow-up visits are frequent for 3-6 months. The longer recovery is the price for the stronger pressure drop.
Do I still need eye drops after surgery?
Often, yes - but fewer. After MIGS, most people reduce their eye drops by 1.5 to 2. After trabeculectomy, some stop entirely, but many still need one or two to maintain pressure. The goal isn’t always to eliminate drops, but to reduce them enough to improve comfort and reduce side effects.
Are there risks of blindness from glaucoma surgery?
The risk is very low, but it exists. Trabeculectomy carries a 0.5%-2% long-term risk of endophthalmitis - a serious eye infection that can lead to vision loss. MIGS has a risk under 0.5%. Both procedures are far safer than letting glaucoma go untreated. The bigger risk isn’t surgery - it’s waiting too long to act.



Freddy King
February 17, 2026 AT 17:00Trabeculectomy’s bleb is basically a biological pressure relief valve - elegant in its crudeness. The fact that it’s still the gold standard after 60 years says more about our lack of innovation than its superiority. MIGS is the future, but we’re stuck in a reimbursement-driven inertia loop. Insurance won’t cover MIGS as standalone unless you’ve failed 3 drops, 2 lasers, and a blind faith in hope. Classic.
And don’t get me started on SLT. The LiGHT trial? Brilliant. But in the real world, most docs still push drops because they’re easier to bill and easier to forget about. We’ve turned glaucoma into a subscription service.