PCP Prophylaxis Risk Calculator
This tool helps you understand your risk of Pneumocystis pneumonia based on your current medications and immune status. It's designed to help you and your doctor make informed decisions about prophylaxis.
When Do You Need Antibiotics to Prevent a Rare but Deadly Lung Infection?
If you’re taking high-dose steroids or other strong immunosuppressants, you might have been told you need to take an antibiotic every day-not to treat an infection, but to prevent one. That antibiotic is usually trimethoprim-sulfamethoxazole (TMP-SMX), and the infection it’s meant to stop is Pneumocystis jirovecii pneumonia, or PCP. It sounds alarming. And it should. PCP used to kill nearly half of all HIV patients before antiretrovirals became common. Today, it’s rare-but still deadly in people with weakened immune systems from medications, not viruses.
The question isn’t whether PCP is dangerous. It is. Mortality rates can hit 30-50% if it’s not caught early. The real question is: who actually needs to take daily pills for months or years to avoid it? And why do some doctors prescribe it, while others don’t, even when patients are on the same drugs?
The Drugs That Put You at Risk
Not all immunosuppressants are equal when it comes to PCP risk. Some raise the danger significantly. Others? Not so much.
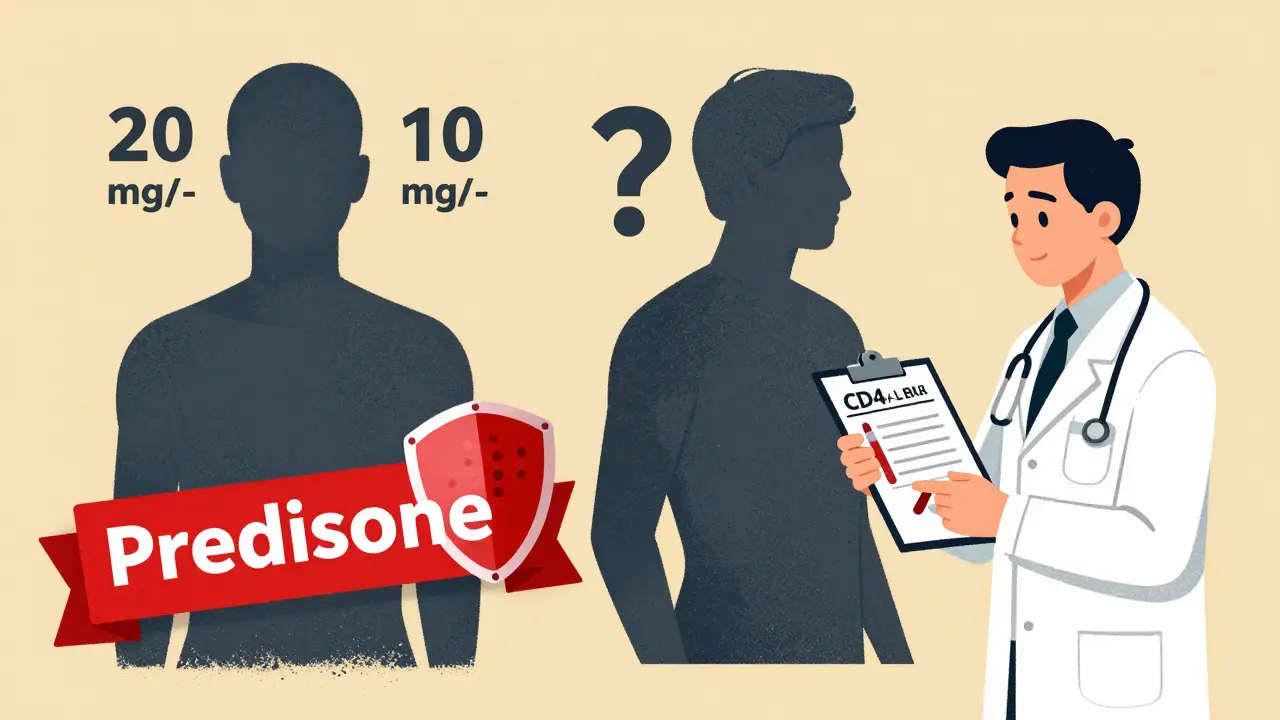
Corticosteroids like prednisone are the most common trigger. If you’re on 20 mg or more per day for four weeks or longer, guidelines from the British Columbia Renal Agency and the CDC say you should consider prophylaxis. That’s the threshold most specialists still use. But here’s the twist: new research from 2025 shows PCP cases have happened in people taking as little as 10 mg/day-especially if they’re also on another immunosuppressant. So the rule isn’t absolute. It’s a starting point.
Cyclophosphamide is another big red flag. Whether you’re taking it for vasculitis, lupus, or kidney disease, this drug wipes out white blood cells for months. Guidelines say prophylaxis should start when you begin cyclophosphamide-and continue for at least three months after you stop. Yet, studies show nearly a quarter of patients on this drug still don’t get the preventive antibiotic.
What about azathioprine or mycophenolate mofetil? Alone? Usually not enough. These drugs suppress the immune system, but not as deeply. The risk is low unless they’re combined with steroids. If you’re on mycophenolate plus prednisone at 15 mg/day? Now you’re in the gray zone. That’s where things get messy.
The Blood Test That Could Change Everything
For HIV patients, it’s simple: if your CD4 count drops below 200, you get prophylaxis. That’s been standard since the 1990s. But for people with autoimmune diseases, there’s no official rule. That’s why some doctors are starting to use CD4 counts as a tool-even for non-HIV patients.
A 2023 EULAR conference report suggested that if your CD4 count falls below 200 cells/µL, you should get prophylaxis, regardless of your drug dose. Why? Because it’s a direct measure of immune weakness. Two people could both be on 20 mg of prednisone. One has a CD4 count of 450. The other has 180. The second person is at much higher risk. Using CD4 counts could cut unnecessary prophylaxis by up to 35%, according to early data.
But here’s the catch: not every clinic checks CD4 counts for rheumatology or nephrology patients. It’s not routine. So if you’re on immunosuppressants and haven’t had a CD4 test in the last six months, ask for one. It might be the missing piece.
The Prophylaxis That Works-And the Side Effects You Can’t Ignore
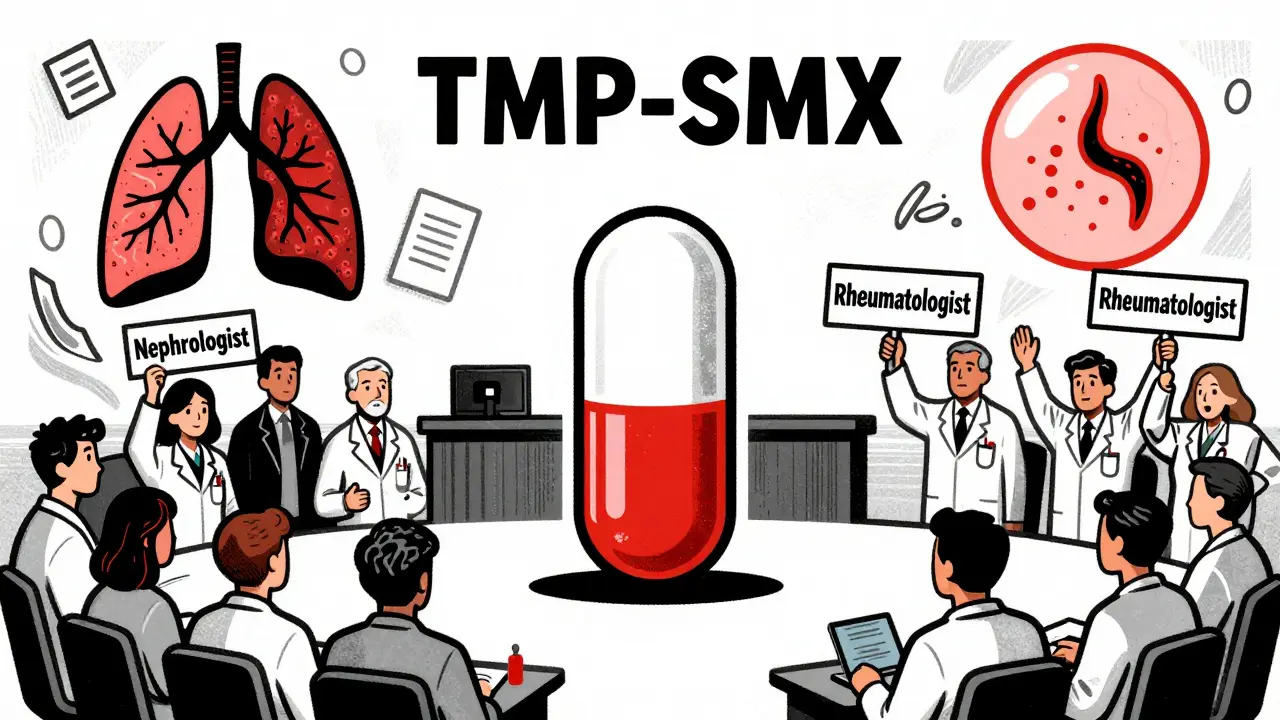
Trimethoprim-sulfamethoxazole (TMP-SMX) is the gold standard. One double-strength tablet daily. Cheap. Effective. And it’s been used for decades with proven results. But it’s not easy to tolerate.
About 20-30% of people can’t take it. Why? Rash, itching, nausea, liver enzyme spikes, or low blood counts. One patient in Perth told me she broke out in hives after three days and had to stop. Another developed severe nausea that made her miss work for a week. These aren’t rare side effects. They’re common.
If you can’t take TMP-SMX, alternatives exist-but they’re worse. Dapsone can cause anemia. Atovaquone is expensive. Aerosolized pentamidine requires monthly clinic visits and can trigger coughing fits. And if you’re on mycophenolate? Avoid dapsone. It can crush your bone marrow even harder.
And here’s something few doctors mention: long-term antibiotic use doesn’t cause antibiotic resistance in Pneumocystis. The fungus hasn’t developed resistance to TMP-SMX. But patients worry. Reddit threads are full of people terrified they’ll become “superbug carriers.” That fear is real. But the science says: no, you won’t. The resistance you hear about is in staph or E. coli-not PCP.
The Big Contradiction: No Cases, But Still Prescribed?
In 2018, researchers followed 316 patients on high-risk immunosuppressants for nearly two years. Nearly 40% didn’t get prophylaxis. Zero got PCP. Meanwhile, 2.2% of patients had serious side effects from the preventive antibiotics every year. That’s about one in 45 people getting sick from the treatment, not the infection.
That study shook the field. It didn’t say prophylaxis is useless. It said: maybe we’re overtreating. Maybe the risk is lower than we thought. Maybe the side effects are worse than the disease.
That’s why some rheumatologists now say: “Only give it if you have two risk factors.” Like: high-dose steroids and low CD4 count and recent CMV infection. If you only have one? Maybe skip it. Monitor. Test your blood. Watch for fever or cough.
But nephrologists and transplant teams? They still prescribe it like clockwork. Why? Because in their world, PCP kills fast-and they’ve seen it happen. One case can cost $50,000 in hospital bills. Prophylaxis costs $200 a year. For them, it’s not about whether it’s needed-it’s about avoiding a disaster.
What You Should Do Right Now
If you’re on immunosuppressants, here’s your action plan:
- Check your steroid dose. Are you on ≥20 mg prednisone daily for more than four weeks? If yes, talk to your doctor about prophylaxis.
- Ask for your CD4 count. If it’s below 200, prophylaxis is strongly recommended-even if you’re not on high-dose steroids.
- Review your drugs. Are you on cyclophosphamide? Then you need it. On azathioprine alone? Probably not.
- Discuss side effects. If you’ve had a rash or nausea before, tell your doctor. Don’t just quit the pill-ask for alternatives.
- Don’t assume you’re safe. Even if you feel fine, PCP doesn’t cause symptoms until it’s advanced. That’s why prevention matters.
And if your doctor says, “You don’t need it”-ask why. What’s your CD4 count? Are you on other drugs? How long have you been on steroids? A good answer should include numbers, not just opinions.
The Bottom Line: It’s Not One-Size-Fits-All
There’s no universal rule for PCP prophylaxis in non-HIV patients. That’s frustrating. But it’s also true. The risk depends on your drugs, your blood counts, your age, your other illnesses, and even your doctor’s specialty.
What’s clear: PCP is rare, but deadly. TMP-SMX works. But it’s not harmless. The goal isn’t to give everyone a pill. It’s to give the pill to the people who will truly benefit-and spare the rest from side effects they don’t need.
If you’re on immunosuppressants, don’t wait for your doctor to bring it up. Ask. Test. Understand. Your lungs might thank you years from now.
Do I need PCP prophylaxis if I’m on prednisone at 10 mg/day?
Not automatically. The standard threshold is 20 mg/day for four weeks or more. But if you’re on 10 mg/day and also taking another immunosuppressant like mycophenolate, or if your CD4 count is below 200, your risk increases. Talk to your doctor about combining your drug list with your blood test results to make a personalized call.
Can I stop PCP prophylaxis if I lower my steroid dose?
Yes, often you can. If you’ve been on prophylaxis because of high-dose steroids and you’ve tapered below 20 mg/day for at least four weeks, your doctor may consider stopping it-especially if your CD4 count is normal and you’re not on other high-risk drugs. But don’t stop on your own. Always check with your provider first.
Is TMP-SMX safe during pregnancy?
Yes, TMP-SMX is generally considered safe during pregnancy for PCP prevention, especially after the first trimester. However, aerosolized pentamidine and oral atovaquone should be avoided in the first trimester due to potential risks to the fetus. Always discuss your pregnancy status with your doctor before starting or continuing any prophylaxis.
Why do some doctors prescribe prophylaxis and others don’t?
Specialty differences matter. Nephrologists and transplant doctors follow strict protocols because they’ve seen PCP kill patients after transplants. Rheumatologists are more cautious because studies show low PCP rates even without prophylaxis in autoimmune patients. There’s no national guideline for non-HIV cases, so practice varies widely. Ask your doctor what evidence they’re using to make their decision.
Does taking PCP prophylaxis increase antibiotic resistance?
No, not for Pneumocystis jirovecii. The fungus has not developed resistance to TMP-SMX. The rise in antibiotic resistance you hear about-like MRSA or resistant E. coli-is unrelated. This is a targeted prevention for a specific fungus, not broad-spectrum use. The fear of resistance is understandable, but the data doesn’t support it in this case.
What if I can’t tolerate TMP-SMX?
There are alternatives: dapsone (but avoid if you’re on mycophenolate), atovaquone (expensive), or monthly aerosolized pentamidine (requires clinic visits). Each has trade-offs. Dapsone can cause anemia. Atovaquone is costly. Pentamidine can irritate your lungs. Your doctor should help you pick the best option based on your health history, not just the first alternative listed.



Juan Reibelo
January 24, 2026 AT 16:11Amelia Williams
January 25, 2026 AT 20:09Viola Li
January 27, 2026 AT 18:36Patrick Gornik
January 28, 2026 AT 10:27Sawyer Vitela
January 29, 2026 AT 14:19Kat Peterson
January 30, 2026 AT 20:51Luke Davidson
February 1, 2026 AT 16:49Jenna Allison
February 3, 2026 AT 02:06siva lingam
February 3, 2026 AT 10:00blackbelt security
February 5, 2026 AT 00:04venkatesh karumanchi
February 6, 2026 AT 00:41Elizabeth Cannon
February 6, 2026 AT 22:54Izzy Hadala
February 6, 2026 AT 23:42