Bronchodilator Comparison Tool
Select your conditions and preferences to find the best bronchodilator option:
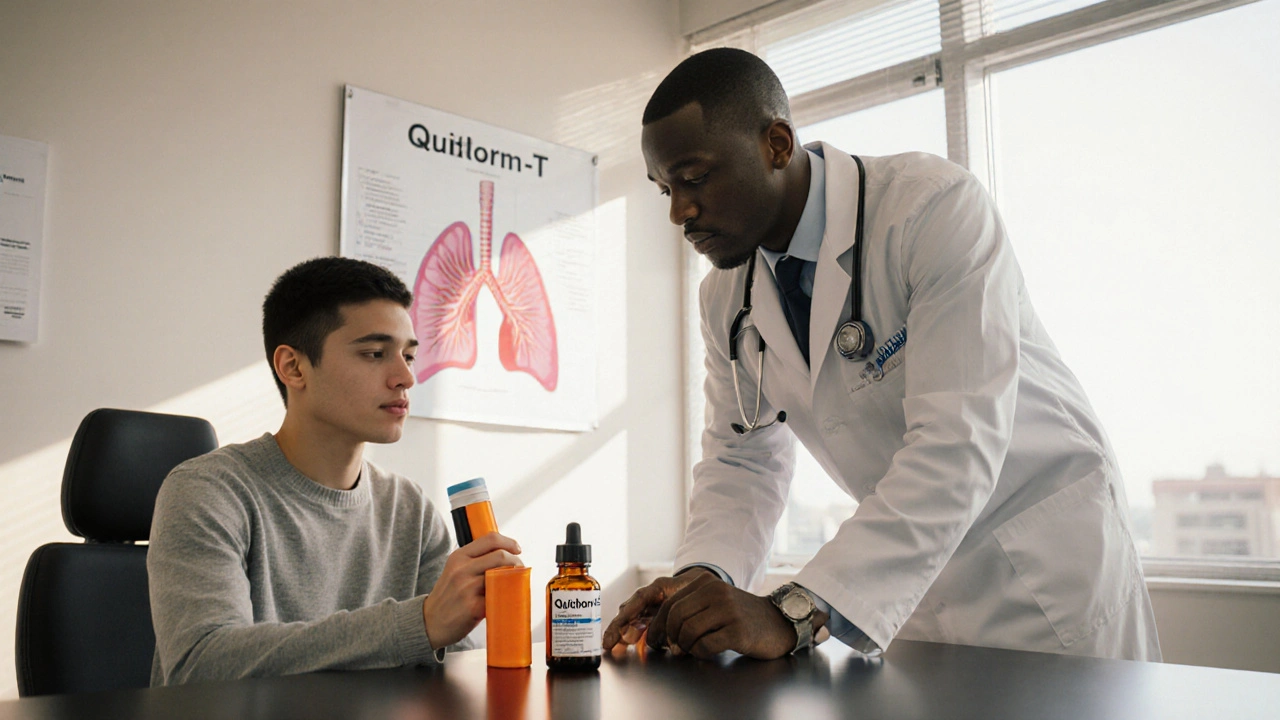
When you’re juggling asthma or COPD, picking the right inhaler or tablet can feel like a high‑stakes gamble. Quibron‑T is a brand‑name tablet that delivers theophylline, a methylxanthine bronchodilator that relaxes airway muscles and improves breathing. But is it the best fit for you, or do faster‑acting options like Albuterol or anti‑inflammatory pills such as Montelukast make more sense? This guide breaks down the key factors, runs a side‑by‑side table, and helps you decide which route matches your lifestyle, symptom pattern, and safety needs.
TL;DR
- Quibron‑T (theophylline) works slowly, needs blood‑level monitoring, and is best for chronic control when inhalers aren’t enough.
- Albuterol and Salbutamol give fast relief for sudden attacks but don’t treat underlying inflammation.
- Montelukast targets leukotriene‑driven inflammation, useful for exercise‑induced asthma.
- Ipratropium is a short‑acting anticholinergic good for COPD flare‑ups.
- Long‑acting beta‑agonists (LABA) like Salmeterol or Formoterol pair with inhaled steroids for steady control.
How Quibron‑T Works
Theophylline belongs to the methylxanthine class, the same family as caffeine. It relaxes the smooth muscle in the bronchi by inhibiting phosphodiesterase, which raises cyclic AMP levels and keeps airway passages open. Unlike rescue inhalers, its effect builds over several hours, offering a baseline level of bronchodilation. Because blood concentrations can fluctuate with diet, age, liver function, and other meds, doctors often order periodic serum level checks (usually targeting 10‑20 µg/mL) to stay in the therapeutic window.
Key Decision Factors
Before swapping a tablet for an inhaler-or adding a new pill-ask yourself these questions:
- Speed of relief needed: Do you need seconds‑fast relief for sudden breathlessness, or are you looking for a maintenance backbone?
- Monitoring comfort: Are you okay with regular blood tests and dose adjustments?
- Side‑effect tolerance: Theophylline can cause nausea, insomnia, or heart palpitations; other drugs have different profiles.
- Drug interactions: Theophylline interacts with antibiotics, anticonvulsants, and many heart meds. Inhaled steroids, LABA, or leukotriene blockers have fewer systemic clashes.
- Cost and convenience: Tablets may be cheaper than inhalers for some patients, but insurance coverage varies.
Comparison Table
| Medication | Class | Onset (minutes) | Duration (hours) | Typical Use | Monitoring Needed? | Common Side‑effects |
|---|---|---|---|---|---|---|
| Quibron‑T | Methylxanthine (Theophylline) | 30-60 | 6-12 | Maintenance for asthma/COPD when inhalers insufficient | Serum level checks | Nausea, insomnia, tachycardia |
| Albuterol | Short‑acting beta‑agonist (SABA) | 5-15 | 4-6 | Rescue inhaler for acute bronchospasm | No | Tremor, jitteriness, palpitations |
| Montelukast | Leukotriene receptor antagonist | 60-120 | 24+ | Daily control, especially exercise‑induced asthma | No | Headache, abdominal pain, mood changes |
| Ipratropium | Short‑acting anticholinergic | 15-30 | 4-6 | COPD exacerbation, adjunct to SABAs | No | Dry mouth, cough, urinary retention |
| Salmeterol | Long‑acting beta‑agonist (LABA) | 15-30 | 12 | Maintenance, always paired with inhaled steroid | No (but watch for overuse) | Throat irritation, rare cardiac effects |
When to Choose Quibron‑T
Quibron‑T shines in three scenarios:
- Patients on multiple inhalers who still have day‑time wheeze despite optimal inhaled steroid/LABA combos.
- Rural or low‑resource settings where daily inhaler technique education is hard to maintain.
- Individuals with a documented “theophylline‑responsive” phenotype-often confirmed after a trial of short‑acting bronchodilators fails to fully control symptoms.
Because theophylline metabolism slows with age and in liver disease, older adults (especially >65) need careful dosing. If you’re already on a medication like ciprofloxacin or erythromycin, the risk of a sudden rise in serum theophylline is real, so a clinician may steer you toward an inhaled route instead.
Alternative Options Overview
Here’s a quick rundown of the most common alternatives you’ll encounter:
- Albuterol (or Salbutamol): The go‑to rescue inhaler. Works within minutes, easy to self‑administer via metered‑dose inhaler or nebulizer.
- Montelukast: Oral pill taken once daily, especially useful if you have allergic rhinitis or asthma triggered by exercise.
- Ipratropium: Often prescribed as a twice‑daily inhalation for COPD-adds a bronchodilator that works via a different pathway than beta‑agonists.
- Salmeterol / Formoterol: LABA agents that provide 12‑hour coverage but must be paired with an inhaled corticosteroid (ICS) like Budesonide or Fluticasone for safety.
- Inhaled corticosteroids (ICS): The backbone of chronic asthma control, reducing airway inflammation over weeks.
Each alternative carries its own trade‑off between speed, convenience, and side‑effect burden. Your personal health profile-especially heart health, liver function, and susceptibility to allergic triggers-will tip the scales.
Pros & Cons Summary
| Medication | Pros | Cons |
|---|---|---|
| Quibron‑T | Oral, long‑acting baseline bronchodilation; useful when inhaler technique is poor; relatively cheap. | Requires blood level monitoring; narrow therapeutic index; side‑effects like insomnia and arrhythmia. |
| Albuterol | Rapid relief; no blood tests; short half‑life reduces systemic exposure. | Only symptom relief, no anti‑inflammatory effect; tachyphylaxis with overuse. |
| Montelukast | Once‑daily oral; good for exercise‑induced and allergic asthma. | Less effective for acute bronchospasm; potential mood changes. |
| Ipratropium | Effective for COPD; works via a different mechanism. | Inhaled only; can cause dry mouth; slower onset than SABAs. |
| Salmeterol | Long‑acting control; reduces daily symptom load. | Must be combined with an inhaled steroid; risk of asthma‑related death if misused. |

Frequently Asked Questions
Do I need regular blood tests while taking Quibron‑T?
Yes. Theophylline has a narrow therapeutic window, so clinicians usually check serum levels every 3‑6 months or after any dose change. The target range is 10‑20 µg/mL.
Can I use Quibron‑T and an inhaled steroid together?
Absolutely. In fact, many treatment plans combine a low‑dose theophylline tablet with an inhaled corticosteroid to cover both baseline bronchodilation and inflammation.
What foods affect theophylline levels?
High‑caffeine drinks, grapefruit juice, and large amounts of fatty foods can slow theophylline metabolism, raising blood concentrations. Stick to moderate caffeine and avoid grapefruit while on Quibron‑T.
Is Quibron‑T safe for pregnant women?
Theophylline crosses the placenta and may cause fetal tachycardia. Most guidelines advise using inhaled options during pregnancy unless the benefit outweighs the risk.
How does Quibron‑T compare cost‑wise to inhalers?
Generally, tablets are cheaper per dose than metered‑dose inhalers, especially if you don’t have private insurance coverage for inhalers. However, add‑on costs for blood tests and potential side‑effect management can narrow the gap.




Roberta Giaimo
September 30, 2025 AT 14:06Thanks for the clear breakdown 😊
Tom Druyts
October 9, 2025 AT 08:06Really appreciate the effort you put into this guide. It’s awesome to have everything from theophylline to LABAs laid out side‑by‑side. For anyone juggling inhalers and pills, having a quick visual reference can save a lot of confusion. If you’re new to asthma management, start with the rescue options and then think about maintenance. Keep pushing forward, you’ve got this!
Julia C
October 18, 2025 AT 02:06The article feels like it’s trying too hard to be exhaustive, yet it glosses over the real danger of theophylline toxicity. Everyone knows that the therapeutic window is razor‑thin, and the piece barely mentions that a single missed dose can swing you into arrhythmia territory. Also, the claim that tablets are cheaper ignores the hidden cost of regular blood draws. It’s almost as if the author wants you to ignore the fact that many patients end up in the ER because of sudden spikes. I can’t shake the feeling they’re downplaying the risk to sell a cheap alternative. Plus, the table formatting looks like a copy‑paste job from some 90s brochure. If you’re going to recommend a drug that needs constant monitoring, you should highlight the logistics more clearly.
John Blas
October 26, 2025 AT 19:06I can’t believe they left out the cost analysis!
Darin Borisov
November 4, 2025 AT 13:06From an epistemological standpoint, the discourse surrounding quinidine analogs such as Quibron‑T necessitates a paradigmatic reevaluation of bronchodilatory pharmacodynamics within the context of polypharmacy. The intricate interplay between phosphodiesterase inhibition and the consequent accrual of intracellular cAMP delineates a mechanistic pathway that diverges fundamentally from beta‑adrenergic agonism. Moreover, the pharmacokinetic variability imposed by hepatic cytochrome P450 isoenzymes, particularly CYP1A2, engenders a stochastic element that mandates therapeutic drug monitoring to circumvent supratherapeutic excursions. This is further compounded by the fact that dietary constituents-caffeine and theobromine-exert competitive inhibition, thereby modulating bioavailability in a manner that is often underappreciated in clinical curricula. The lacuna in patient education regarding such interactions perpetuates a milieu of inadvertent toxicity. In addition, the socioeconomic stratification inherent to inhaler versus oral administration introduces a cost‑benefit analysis that must be contextualized within health economics frameworks. While the inhaler delivery system obviates the need for serum monitoring, it imposes recurring acquisition costs that may be prohibitive for underserved populations. Conversely, the tablet modality, albeit ostensibly economical, incurs ancillary expenses tied to laboratory assays and potential hospitalizations due to adverse events. It is imperative, therefore, that prescribers adopt a holistic algorithmic approach, integrating pharmacogenomic profiling, comorbid hepatic insufficiency, and patient adherence patterns. The extant literature, albeit fragmented, underscores a trend toward personalized medicine that eschews a one‑size‑fits‑all doctrine. Consequently, the decision matrix should prioritize longitudinal outcome metrics, such as exacerbation frequency and quality‑adjusted life years, over simplistic dichotomies of “fast‑acting” versus “slow‑acting.” Ultimately, the clinician’s fiduciary duty extends beyond mere symptom mitigation; it encompasses the stewardship of therapeutic resources in a manner that is both ethically sound and scientifically rigorous.
Sean Kemmis
November 13, 2025 AT 07:06The guide is fine but it downplays the risk of theophylline. Blood tests are a hassle and the side effects can be nasty; still, many just ignore that.
Nathan Squire
November 22, 2025 AT 01:06Tom, good point about starting with rescue options. Just a heads‑up: theophylline levels can jump after a course of antibiotics like ciprofloxacin, so keep an eye on that interaction. It’s also worth noting that while tablets are cheap, the cumulative cost of monitoring can add up. If you’re on a tight schedule, an inhaled steroid plus a low‑dose LABA might be a cleaner solution.
satish kumar
November 30, 2025 AT 19:06Julia, while your concerns are valid, the article does mention monitoring frequency-every 3‑6 months-so it’s not entirely omitted. Moreover, the claim that tablets are cheaper overlooks insurance formularies where inhalers may be reimbursed at a lower copay. One could argue that the author presented a balanced view, albeit succinctly.
Matthew Marshall
December 9, 2025 AT 13:06Darin’s deep dive is impressive, but for most patients the key takeaway is simple: if you can’t manage inhalers, consider a low‑dose theophylline with careful monitoring.
Lexi Benson
December 18, 2025 AT 07:06John’s note on cost is spot on-without factoring in monitoring, the cheap tablet can become pricey.
Vera REA
December 27, 2025 AT 01:06This guide does a solid job of laying out the pros and cons of each class. I especially like the clear list of side‑effects, which can be a quick reference for patients. It might be helpful to add a short section on how lifestyle factors-like caffeine intake-affect theophylline metabolism. Overall, a useful resource for anyone navigating asthma or COPD treatment options.
John Moore
January 4, 2026 AT 19:06Vera, I agree that the side‑effect table is handy. To build on that, consider adding a decision flowchart-visual learners will appreciate a quick path from symptom pattern to recommended therapy.