Most people with asthma or COPD rely on inhalers to breathe easier. But here’s the hard truth: if you’re not using your inhaler correctly, you might as well be breathing in air. Studies show 70 to 90% of patients get less than 30% of their medication into their lungs because of simple mistakes. That’s not just ineffective-it’s dangerous. Your inhaler isn’t broken. You just haven’t been taught how to use it right.
Why Technique Matters More Than the Device
You might think the brand or type of inhaler makes the biggest difference. It doesn’t. What matters more is whether you’re pressing the canister at the right time, breathing in deeply enough, or holding your breath long enough. A 2022 study in Respiratory Medicine found only 23% of people could coordinate pressing and inhaling with a standard metered-dose inhaler (MDI) without training. That means most people are wasting most of their medicine.
The good news? When used correctly, even the cheapest inhaler works as well as the most expensive one. The Agency for Healthcare Research and Quality found real-world effectiveness drops by 30-40% just because of bad technique-not because the drug is weak. The UK Inhaler Group says technique is the #1 factor in success, even more important than choosing between MDIs, DPIs, or soft mist inhalers.
The Three Main Types of Inhalers (and How They Work)
There are three main types of inhalers, and each works differently. Using the wrong method for your device can cut effectiveness in half-or worse.
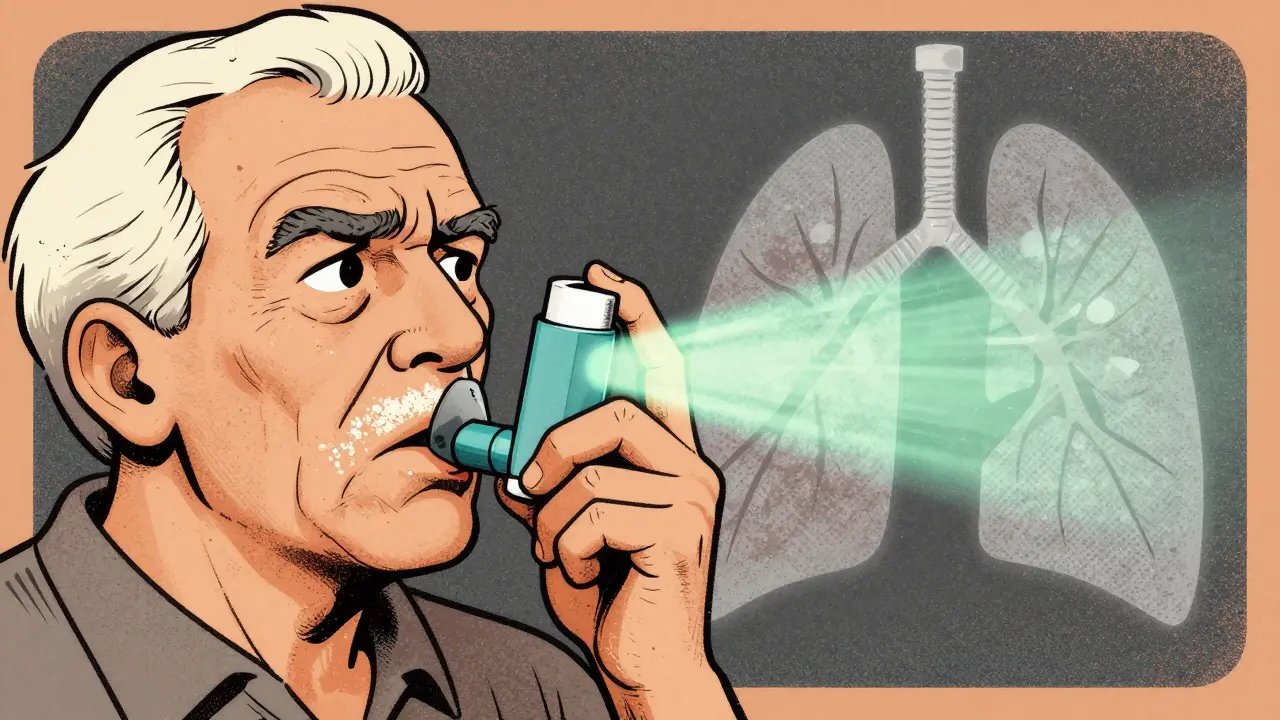
- Metered-Dose Inhalers (MDIs) - These are the canisters you shake and spray. They use a propellant to push out a puff of medicine. You have to press the canister and breathe in at the exact same time. If you’re too early or too late, most of the medicine hits your throat instead of your lungs. Common brands include ProAir HFA and Ventolin HFA.
- Dry Powder Inhalers (DPIs) - These don’t need a propellant. You breathe in fast and hard to pull the powder into your lungs. Devices like Diskus, Turbuhaler, and Ellipta rely on your breath to activate them. But if you’re too weak or too slow-common in advanced COPD-the powder won’t get where it needs to go. These are useless if you can’t take a strong, deep breath.
- Soft Mist Inhalers - These are newer, like Respimat. They create a slow-moving mist that stays in the air longer, giving you more time to inhale. You still need to coordinate, but it’s easier than with MDIs. No need to time your breath perfectly.
Here’s the catch: You can’t use a spacer with a DPI. Spacers help MDIs, but they ruin DPIs. A 2022 study in the Journal of Aerosol Medicine showed using a spacer with a DPI cuts delivery by 50-70%. If you’re told to use one, make sure you know which device you’re holding.
How to Use an MDI the Right Way (Step-by-Step)
If you’re using an MDI, here’s what you need to do. Do this every single time-even if you’ve been doing it for years.
- Remove the cap and shake the inhaler well for 5 seconds.
- Breathe out fully-away from the inhaler. Don’t exhale into it.
- Hold the inhaler upright, with the mouthpiece between your lips. Seal your lips tightly.
- Start breathing in slowly through your mouth. As you begin to inhale, press down on the canister to release one puff.
- Keep breathing in slowly for 3 to 5 seconds until your lungs are full.
- Hold your breath for 10 seconds. This lets the medicine settle in your airways.
- Breathe out slowly through your nose.
Wait 60 seconds before taking another puff. If you rush it, the second puff won’t land properly. And always rinse your mouth with water after using corticosteroid inhalers. It cuts your risk of oral thrush by 75%.
How to Use a DPI the Right Way (Step-by-Step)
DPIs are simpler in some ways-no timing needed-but harder in others. You need strong breath power.
- Load the dose as instructed (some need you to slide a lever, others twist a base).
- Breathe out fully-away from the device. Never exhale into the mouthpiece.
- Put the mouthpiece in your mouth and seal your lips.
- Inhale quickly and deeply-like you’re trying to suck a thick milkshake through a straw.
- Hold your breath for 10 seconds.
- Breathe out slowly.
Don’t shake a DPI. Don’t open the capsule. Don’t try to blow into it. These are common mistakes. A 2023 survey by the COPD Foundation found 31% of users reported powder getting stuck in their throat, causing coughing. That’s usually because they didn’t inhale fast enough.
Why Spacers Are a Game-Changer (But Only for MDIs)
A spacer is a tube that attaches to your MDI. It holds the puff of medicine so you don’t have to time your breath perfectly. The Global Initiative for Asthma (GINA) recommends spacers for everyone using MDIs-even adults.
Without a spacer, only 8-30% of the medicine reaches your lungs. With a spacer? That jumps to 40-60%, matching DPI efficiency. And it cuts down on throat irritation and hoarseness.
Here’s how to use one:
- Attach the spacer to your MDI.
- Shake the inhaler.
- Press the canister once.
- Breathe in slowly through your mouth until your lungs feel full.
- Hold your breath for 10 seconds.
Spacers are especially helpful for kids, older adults, and anyone with shaky hands. They’re cheap, reusable, and often covered by insurance. If you’re still using an MDI without one, you’re making your condition harder to control.
Common Mistakes (And How to Fix Them)
These errors are everywhere-and they’re killing your results.
- Not shaking the MDI - 45% of users skip this. Shake it for 5 seconds before every puff. The medicine settles at the bottom.
- Exhaling into the device - 27% do this. Always breathe out away from the inhaler. Moisture ruins powder and dilutes spray.
- Not holding your breath - 63% don’t hold for 10 seconds. That’s the most important step. It lets the medicine stick to your airways instead of being breathed out.
- Using multiple inhalers without training - The European Respiratory Society warns this causes 35-50% less effectiveness. If you have two devices, ask your doctor to show you the difference.
- Storing inhalers too hot - Keep them between 20-25°C. Above 30°C, the medication loses 15-20% potency. Don’t leave them in your car or by the sink.
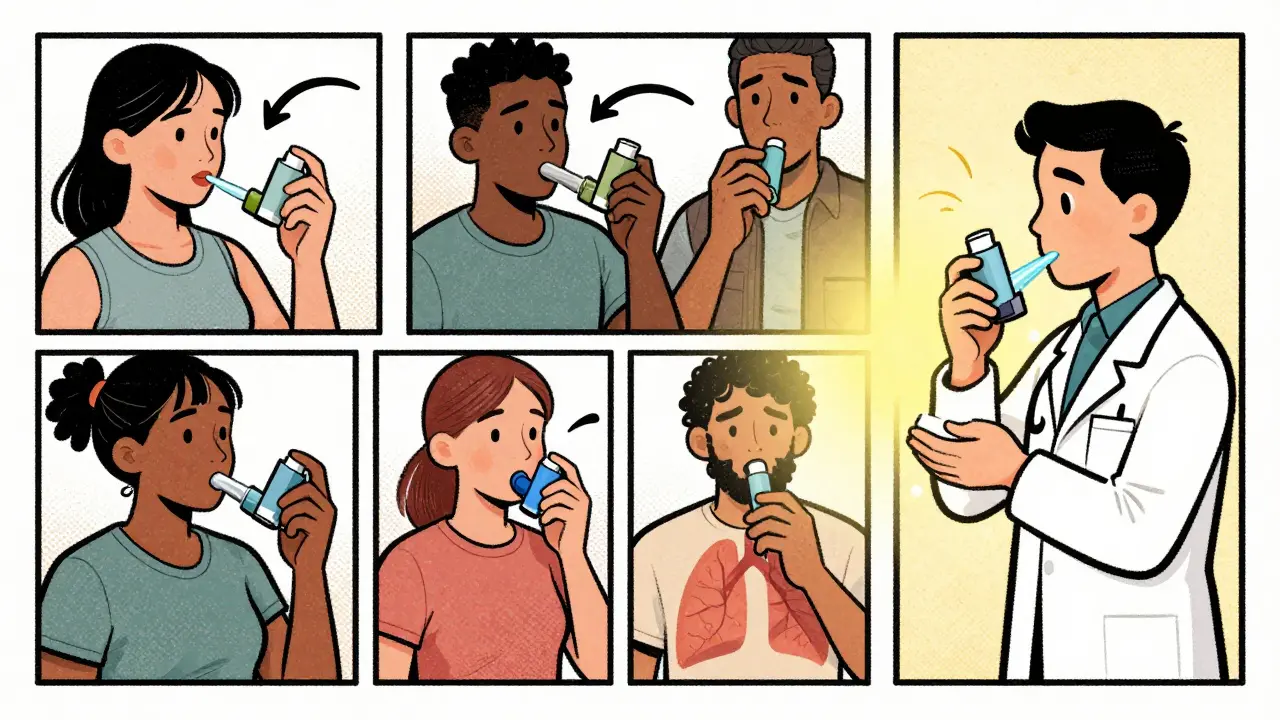
Who Struggles the Most (And What to Do)
Older adults, especially over 65, have a harder time with DPIs because they can’t generate enough airflow. The National Asthma Council Australia found 62% of seniors struggle with DPIs. If you’re older or have severe COPD, stick with an MDI and spacer.
Children under 6 can’t coordinate inhalation with MDIs. Use a spacer with a mask. If you’re a caregiver, ask for a demonstration at your next appointment.
People with arthritis or shaky hands struggle with MDIs. Talk to your doctor about switching to a DPI or a soft mist inhaler. Or ask about a breath-actuated MDI-these release medicine automatically when you inhale. They’re coming to market soon.
What to Do If Your Inhaler Doesn’t Work
If you’re using your inhaler correctly and still having symptoms, it’s not your fault. It’s probably not the inhaler. It might be:
- Your diagnosis needs rechecking
- You need a different medication
- You’re missing another trigger (like smoke, pollen, or cold air)
- You’re not using your maintenance inhaler daily
Don’t just take more puffs. That won’t help-and it can hurt. Go back to your doctor. Ask them to watch you use your inhaler. Most won’t offer unless you ask. But you deserve to breathe better.
What’s Changing in 2026
The future is getting smarter. Smart inhalers with built-in sensors-like Propeller Health-are now FDA-approved. They track when you use your inhaler and even detect if your technique is off. A 2022 study in Annals of Internal Medicine found they’re 92% accurate.
By 2025, 40% of inhalers are expected to have digital tracking. That means your doctor will know if you’re skipping doses or using it wrong. It’s not about being watched-it’s about getting better care.
Even better? Breath-actuated MDIs are in Phase 3 trials. These release medicine automatically when you inhale. No timing needed. They’ll be available soon.
But here’s the reality: No smart device fixes bad technique. The best technology in the world won’t help if you don’t know how to use it. That’s why training matters more than ever.
Get It Checked-Now
Don’t wait until your next appointment. Ask your pharmacist or nurse to watch you use your inhaler today. Most have demo models. Bring your device. Do it in front of them. If they don’t offer, ask: "Can you watch me use my inhaler? I want to make sure I’m doing it right."
It takes three tries to get it right. Most people need three sessions with a healthcare provider to master technique. Don’t assume you know how. You probably don’t.
And if you’ve been using your inhaler wrong for years? You’re not alone. On Reddit’s asthma community, 42% of users said they only learned proper technique after multiple doctor visits. One user wrote: "I’ve been using my inhaler wrong for 10 years."
It’s not too late. Start today. Breathe better tomorrow.
Can I use my inhaler without shaking it?
No. Shaking your metered-dose inhaler (MDI) for 5 seconds before each puff ensures the medicine and propellant are properly mixed. Skipping this step means you might get too much propellant and not enough medicine-or vice versa. About 45% of users skip shaking, which is one of the most common reasons inhalers seem ineffective.
Is it okay to use a spacer with a dry powder inhaler?
No. Spacers are designed for metered-dose inhalers (MDIs) only. Using a spacer with a dry powder inhaler (DPI) blocks the airflow needed to lift the powder into your lungs. Studies show this reduces medication delivery by 50-70%. Always check your device type before attaching anything.
Why does my inhaler make me cough?
Coughing after using an inhaler usually means the medicine is hitting your throat instead of your lungs. This happens with DPIs if you don’t inhale fast enough, or with MDIs if you don’t coordinate the puff with your breath. It can also happen if you don’t rinse your mouth after corticosteroid inhalers. Try slower, deeper breaths and always rinse with water after use.
How long should I hold my breath after using an inhaler?
Hold your breath for 10 seconds after inhaling the medicine. This gives the medication time to settle in your airways instead of being exhaled. Studies show this increases lung deposition by 20-30%. If you can’t hold it for 10 seconds, do as long as you can-every extra second helps.
Can I use my inhaler if it’s cold or left in the sun?
Store your inhaler between 20-25°C. If it’s too hot (above 30°C), the medication loses 15-20% of its potency. If it’s too cold, the propellant may not work properly. Don’t leave it in your car, near a heater, or in a cold bathroom. Keep it in your pocket or a cool, dry drawer.
What if I miss a dose of my maintenance inhaler?
If you miss a dose of your daily controller inhaler (like an inhaled corticosteroid), don’t double up next time. Just take your next dose as scheduled. Missing one dose won’t cause an attack-but skipping regularly will. Use reminders, phone alarms, or smart inhalers to stay on track.
Do I need to clean my inhaler?
Yes, but only the mouthpiece. For MDIs, rinse the plastic mouthpiece under warm water once a week. Let it air dry completely before using. Never rinse the metal canister or put it in the dishwasher. For DPIs, wipe the mouthpiece with a dry cloth. Don’t get them wet. Moisture clogs powder devices.
How do I know if my inhaler is empty?
Most inhalers have a dose counter. If yours doesn’t, write the start date on the canister and estimate how many puffs you use per day. A standard MDI has 120 or 200 puffs. For example, if you use 4 puffs a day, it will last 30 days. Don’t rely on how it feels-empty inhalers can still spray.


Shanahan Crowell
January 3, 2026 AT 04:51OMG I just realized I’ve been using my inhaler wrong for 8 years… I never shook it, never held my breath, and I thought the spacer was optional?!?!?!! I’m going to the pharmacy today to get one-no excuses anymore. Breathe better, people!! 🙌
Ian Detrick
January 4, 2026 AT 01:26It’s wild how something so simple-timing your breath-can be the difference between managing your condition and constantly wheezing. We treat inhalers like magic wands, but they’re precision tools. The real tragedy? Most doctors don’t demonstrate proper use because they assume patients ‘just know.’ We need mandatory inhaler demos at every Rx pickup.
Ian Ring
January 5, 2026 AT 15:38Interesting piece-though I must say, the emphasis on technique is spot on. I’ve seen too many patients with severe COPD, using expensive DPIs, yet unable to generate sufficient inspiratory flow. The solution? MDI + spacer. It’s not glamorous, but it works. And yes, always rinse after corticosteroids-oral thrush is no joke. 😔
JUNE OHM
January 7, 2026 AT 02:41They don’t want you to know this-but the real reason inhalers are so ineffective? Big Pharma doesn’t profit from spacer sales. They push expensive devices, not free plastic tubes. And don’t get me started on the ‘smart inhalers’-that’s just surveillance disguised as healthcare. You’re being tracked, folks. 🕵️♀️
Philip Leth
January 8, 2026 AT 19:30Man, I’m Nigerian, and we don’t even have access to half this stuff. My cousin uses an MDI without a spacer, and he just coughs it all out. No one teaches him. No one checks. We need global education-not just for Americans with insurance. This info should be on YouTube in 10 languages.
Palesa Makuru
January 10, 2026 AT 16:26Let’s be real-most people can’t even follow a 7-step process. You’re telling me a 72-year-old with arthritis and dementia is supposed to hold their breath for 10 seconds? This is elitist nonsense. The system is broken. If your treatment requires perfect execution, it’s not a treatment-it’s a privilege.
Lori Jackson
January 10, 2026 AT 16:52Technique is paramount, but let’s not ignore the pharmacokinetic reality: even with perfect technique, MDIs have suboptimal lung deposition due to oropharyngeal deposition kinetics. The real advancement lies in nebulized formulations or breath-actuated devices-those are the future. Spacers are a band-aid, not a solution. And yes, I’ve published on this in JACI.
Sarah Little
January 10, 2026 AT 20:25Actually, the 70-90% statistic is outdated. A 2023 meta-analysis in Thorax showed improved technique after digital training tools-so it’s not that people are dumb, it’s that healthcare systems fail to educate. Also, DPIs aren’t useless for COPD patients-you just need to assess inspiratory flow first. Not all patients are created equal.
innocent massawe
January 11, 2026 AT 12:06Thanks for this. I’ve been using my inhaler wrong since I was 16. I thought the coughing meant it was working. Now I know it means I’m wasting medicine. I’ll go to my clinic tomorrow. 🙏
erica yabut
January 12, 2026 AT 14:42Ugh. Another ‘just breathe better’ lecture. Meanwhile, my neighbor’s kid has asthma and can’t afford the $400 inhaler, let alone a spacer. This article reads like a luxury magazine for people who have access to healthcare. Tell me again how ‘technique matters’ when you can’t even buy the damn thing?
Tru Vista
January 12, 2026 AT 15:19MDI = 30% lung delivery? Nah. That’s old data. New studies show 45-50% with spacer. Also, you said hold breath 10 sec-what if you have COPD and can’t? Just say ‘as long as possible.’ And don’t forget to clean the mouthpiece. 😴
Vincent Sunio
January 13, 2026 AT 06:58While the article contains several factual assertions, it lacks rigorous citation for the 2022 Respiratory Medicine study referenced. Moreover, the assertion that technique is ‘the #1 factor in success’ contradicts recent Cochrane reviews which place medication adherence and environmental triggers as equally significant variables. Furthermore, the recommendation to use spacers universally is not endorsed by all international guidelines. Precision in language is not optional in medical communication.
Kerry Howarth
January 14, 2026 AT 09:08You’re not alone. I used to do it wrong too. I thought shaking was for ‘mixing the taste.’ Turns out it’s for mixing the medicine. I’m a nurse-got trained last year. Now I demo it for every patient. It takes 90 seconds. It changes lives. You got this.
Tiffany Channell
January 14, 2026 AT 11:17Smart inhalers are a scam. They track your usage, sell your data to insurers, and then raise your premiums because you ‘missed doses.’ You think your doctor cares if you breathe better? No-they care if your numbers look good on the dashboard. Don’t fall for the surveillance trap.