Calcium Channel Blocker Interaction Risk Checker
Check Your Medication Risk
Select your calcium channel blocker and other medications to see potential interaction risks.
Calcium channel blockers (CCBs) are one of the most commonly prescribed classes of heart medications. Millions of people take them every day for high blood pressure, chest pain, or irregular heartbeats. But what most patients don’t realize is that these drugs don’t just work on their own-they’re deeply affected by what else they’re taking. Even something as simple as grapefruit juice or a common antibiotic can turn a safe dose into a dangerous one. The real issue isn’t the drug itself-it’s how your body processes it, and who else is in the mix.
How Calcium Channel Blockers Work (and Why It Matters)
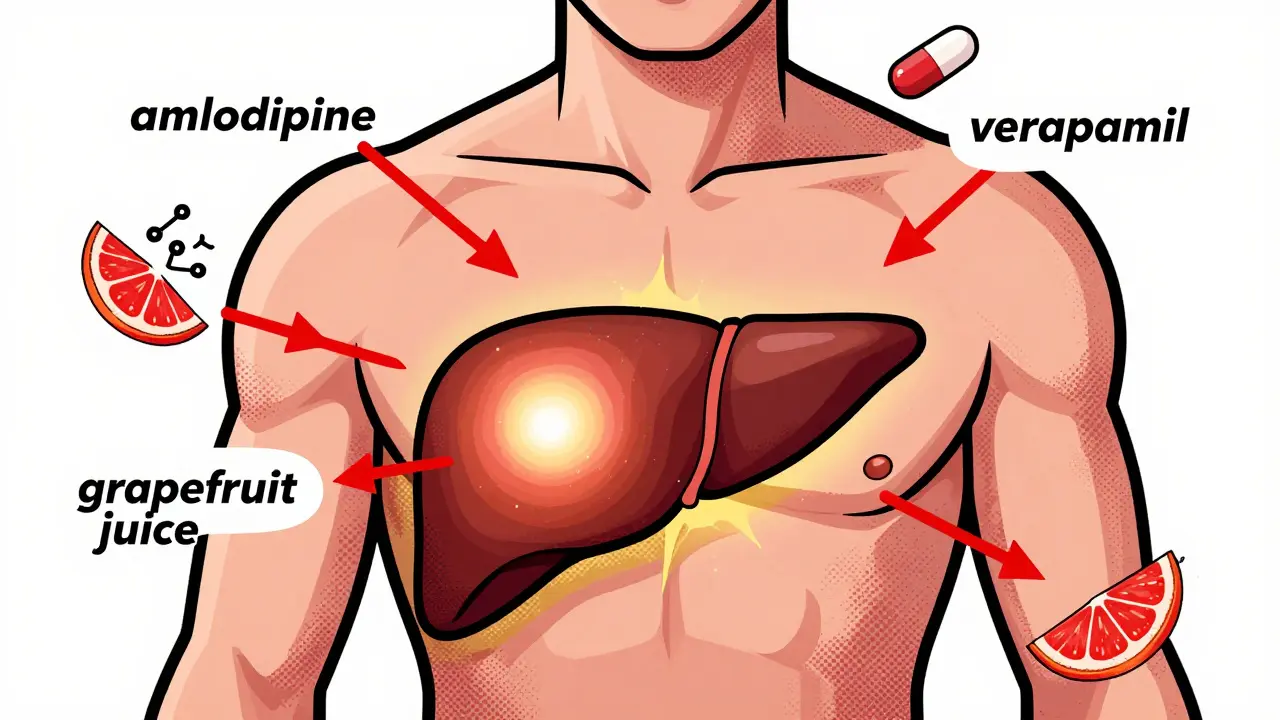
Calcium channel blockers are a class of medications that block calcium from entering heart and blood vessel cells, which relaxes arteries and reduces blood pressure. They’re divided into two main groups: dihydropyridines (DHPs) like amlodipine, nifedipine, and felodipine, and non-dihydropyridines (non-DHPs) like verapamil and diltiazem.DHPs mostly affect blood vessels. They’re great for lowering blood pressure without slowing the heart too much. That’s why amlodipine is the most prescribed CCB-it works well, lasts long, and doesn’t mess with heart rhythm. Non-DHPs like verapamil and diltiazem hit both the heart and blood vessels. They’re used for arrhythmias and angina, but they’re trickier to manage because they slow down the heart’s electrical signals.
The big difference? Amlodipine has a half-life of 30 to 50 hours. You take it once a day. Verapamil? Half-life is only 4 to 12 hours. You need to take it twice. That’s not just about convenience-it’s about how your liver handles them.
The Liver Is the Main Player
Almost all calcium channel blockers are broken down by the same enzyme: CYP3A4. It’s the most important drug-metabolizing enzyme in your liver. About 90% of amlodipine, nifedipine, and felodipine are processed by it. For verapamil, it’s still around 70%. That means if something interferes with CYP3A4, the drug builds up in your system-and fast.
Here’s the catch: many common drugs are CYP3A4 inhibitors. That means they block the enzyme from doing its job. Think antibiotics like clarithromycin, antifungals like itraconazole, HIV meds like ritonavir, even some cancer drugs. When you take one of these with a CCB, your body can’t clear the drug properly. Plasma levels can spike by 300% to 600%. That’s not a small change-it’s a medical emergency waiting to happen.
Real-world data backs this up. Mayo Clinic patient forums recorded 47 emergency visits in one year alone because people took their CCB with grapefruit juice. Grapefruit contains furanocoumarins, which shut down CYP3A4 in the gut. One glass of juice can do what a strong drug does. And it doesn’t matter if you take the juice hours before or after the pill-it still blocks the enzyme.
Amlodipine vs. Verapamil: The Interaction Battle
Not all CCBs are created equal when it comes to drug interactions. Amlodipine is the quiet winner here. It’s a substrate of CYP3A4, but it doesn’t inhibit the enzyme itself. That means it’s mostly affected by other drugs-but it doesn’t go around messing with them. If you’re on 5 or 6 other medications, amlodipine is your safest bet.
Verapamil and diltiazem? They’re double agents. They’re metabolized by CYP3A4, but they also inhibit it. That means they don’t just sit there and get broken down-they actively interfere with how other drugs are processed. Diltiazem can increase the levels of simvastatin by 400%. That’s why some patients on both drugs end up with severe muscle damage, or rhabdomyolysis. Verapamil also blocks P-glycoprotein, a transporter that kicks drugs out of cells. That’s why it raises digoxin levels by 50% to 75%. Digoxin is already a narrow-therapeutic-index drug. A little too much, and you get dangerous heart rhythms.
Studies show that 45% of patients on diltiazem need a dose adjustment when adding a moderate CYP3A4 inhibitor. For amlodipine? Only 12%. That’s why the American Journal of Cardiology recommends amlodipine as first-line for patients on multiple meds.

Who’s at Highest Risk?
Age matters. People over 65 are 3.2 times more likely to have severe interactions. Why? Their liver doesn’t process drugs as well. Their kidneys don’t clear metabolites as fast. And they’re more likely to be on five or more medications. According to the Aging Population Impact Report, 58% of Medicare patients take five or more drugs that can interact with CCBs.
Renal function is another big factor. If your eGFR is below 60 mL/min, you’re at higher risk. But here’s the surprise: amlodipine doesn’t need a dose adjustment even with kidney disease. Verapamil does. The FDA says cut the dose by 50% if your kidneys aren’t working well. That’s because verapamil’s metabolites hang around longer when kidneys slow down. Amlodipine? Less than 1% is excreted unchanged. It’s all liver, not kidneys.
Genetics play a role too. The Pharmacogenomics Research Network found that 27% of people have genetic variants that make CYP3A4 work slower or faster. That means two people taking the same dose of verapamil can have wildly different blood levels. One stays safe. The other ends up in the ER.
What to Do: Practical Steps for Safety
If you’re prescribed a calcium channel blocker, here’s what you need to do:
- Check every medication-prescription, over-the-counter, herbal. Even St. John’s wort can reduce CCB levels by 50%.
- Avoid grapefruit entirely if you’re on verapamil, diltiazem, or nifedipine. Amlodipine is safer, but why risk it?
- Ask your pharmacist to run an interaction check. Community pharmacists spend over 12 minutes per CCB script reviewing this. Don’t assume your doctor caught everything.
- Watch for symptoms: dizziness, fainting, swollen ankles, slow heartbeat. These aren’t just side effects-they’re signs of toxicity.
- Get your dose checked if you start or stop any new drug. Even a common painkiller like ibuprofen can affect blood pressure control.
For doctors: Start with amlodipine 2.5 mg in elderly patients or those on multiple drugs. Monitor blood pressure within 2 hours of the first dose when adding a CYP3A4 inhibitor. For non-DHPs, do an ECG. If you’re using verapamil with a strong inhibitor, consider therapeutic drug monitoring-target trough levels between 50 and 150 ng/mL.

The Future: Personalized Dosing Is Coming
Things are changing fast. In March 2023, the FDA approved CCB-Check, a tool that integrates with electronic health records to flag interaction risks in real time. Hospitals using it saw a 31% drop in hospitalizations from CCB interactions.
Research is also showing that your gut bacteria affect how CCBs are broken down. One study found that 34% of the variation in drug clearance could be explained by microbiome differences. That’s huge. It means two people with the same genes, age, and kidney function could still respond differently to the same dose-because their gut flora is different.
By 2027, personalized dosing based on liver enzymes, kidney function, genetics, and even microbiome data will likely become standard. Until then, the safest rule is simple: if you’re on a calcium channel blocker, assume every new drug or supplement could change how it works.
Bottom Line
Calcium channel blockers save lives. But they’re not harmless. Their power comes with a hidden cost: they’re vulnerable to interactions that can turn a routine dose into a life-threatening event. Amlodipine is the safest choice for most people, especially those on multiple medications. Verapamil and diltiazem are powerful-but they come with more risk. Know your drugs. Know your body. And never assume a medication is safe just because it’s common.
Can I drink grapefruit juice while taking a calcium channel blocker?
No, it’s not safe if you’re taking verapamil, diltiazem, or nifedipine. Grapefruit juice blocks the CYP3A4 enzyme in your gut, causing the drug to build up to dangerous levels. Even a single glass can increase blood levels by 200-300%. Amlodipine is less affected, but it’s still not recommended. Avoid grapefruit entirely unless your doctor confirms it’s safe.
Which calcium channel blocker has the fewest drug interactions?
Amlodipine has the fewest drug interactions among calcium channel blockers. It’s metabolized by CYP3A4 but doesn’t inhibit the enzyme itself. Studies show only 12% of patients need a dose adjustment when taking moderate CYP3A4 inhibitors, compared to 45% for diltiazem. It’s also the only CCB that doesn’t require a dose change in kidney disease, making it the preferred choice for older adults or those on multiple medications.
Why does verapamil raise digoxin levels?
Verapamil doesn’t just affect CYP3A4-it also blocks P-glycoprotein, a transporter that pushes digoxin out of cells. When this pump is blocked, digoxin builds up in the blood. Levels can rise by 50% to 75%, which can cause serious heart rhythm problems. This interaction is so dangerous that the European Heart Journal warns against combining them unless absolutely necessary and under close monitoring.
Can kidney problems affect how calcium channel blockers work?
Yes, but it depends on the drug. Amlodipine is mostly cleared by the liver, so kidney disease doesn’t require a dose change. Verapamil, however, relies on kidney clearance for its metabolites. If your eGFR is below 60 mL/min, you need a 50% dose reduction. Patients with kidney impairment are 47% more likely to have severe interactions with CCBs, especially non-DHPs.
What should I do if I start a new medication while on a calcium channel blocker?
Stop taking the new medication and contact your doctor or pharmacist immediately. Don’t wait for symptoms. Even over-the-counter drugs, herbal supplements, or antibiotics can cause dangerous interactions. Use a drug interaction checker or ask your pharmacist to review all your medications. If you’re on verapamil or diltiazem, be extra cautious-these drugs are more likely to cause problems.



