What’s on Your Prescription Label-and Why It Matters
Every time you pick up a new prescription, you’re handed a small piece of paper that could save your life. But most people glance at it, toss it in their bag, and hope for the best. That’s dangerous. Prescription labels aren’t just paperwork-they’re your roadmap to safe, effective medication use. If you misread one line, you could end up taking too much, too little, or the wrong drug entirely. The good news? You don’t need a medical degree to understand it. You just need to know what to look for.
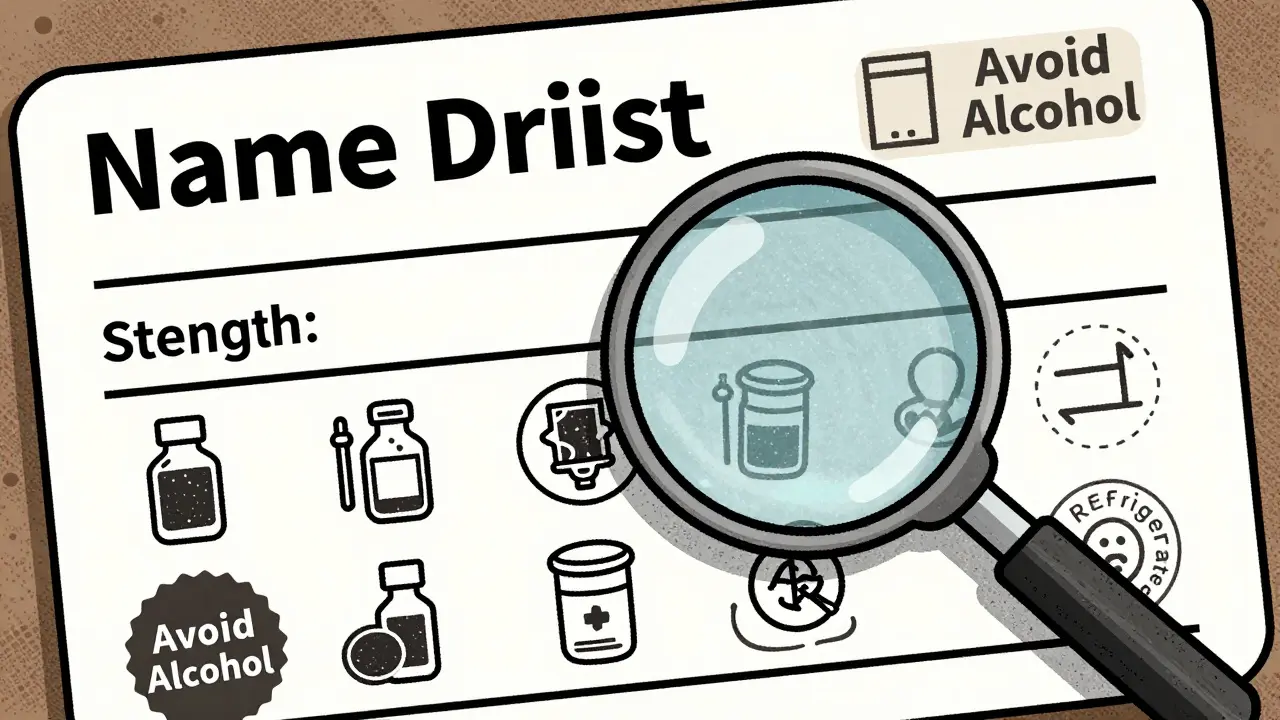
The 12 Key Parts of a Prescription Label
Every prescription label has the same basic structure, no matter which pharmacy you use. Here’s what’s actually on it, and what each part means.
- Your full name-This isn’t just for show. It stops someone else in your household from accidentally taking your medicine. Always double-check that it’s spelled exactly right.
- Medication name-You’ll see both the brand name (like Lipitor) and the generic name (like atorvastatin). In Australia, the generic name is usually listed first. Knowing both helps you recognize the drug if your pharmacy switches brands.
- Prescription number (Rx#)-This is your prescription’s ID. Use it when calling for refills or asking questions. It’s faster than giving your name every time.
- Prescriber’s name-This tells you who ordered the medicine: your doctor, nurse practitioner, or even a dentist. If you’re unsure why you’re taking it, this is who to follow up with.
- Medication strength-This tells you how much of the drug is in each pill, drop, or teaspoon. If your last prescription was 10 mg and this one is 20 mg, that’s a big change. Don’t assume it’s a mistake-call the pharmacy to confirm.
- Quantity dispensed-How many pills, milliliters, or grams did you get? If you were told you’d get 30 pills but only got 20, something’s off.
- Discard or expiration date-Medicines lose power over time. Most are good for one year from when they were filled. After that, they might not work-or could even become unsafe.
- Instructions-This is the most misunderstood part. “Take one tablet twice daily” doesn’t mean “take it when you wake up and when you go to bed.” It means every 12 hours. “Take with food” means eat something before or right after. Vague terms like “as needed” or “daily” cause confusion for nearly 8 out of 10 people.
- Refill info-How many more times can you get this without a new prescription? If it says “0 refills,” you need to see your doctor again.
- Auxiliary labels-These are the small stickers: “Avoid alcohol,” “May cause drowsiness,” “Refrigerate.” They’re not optional. Ignoring them can lead to side effects or make the drug useless.
- Drug Identification Number (DIN)-In Australia, this eight-digit code tells you exactly which version of the drug you have. It’s used by pharmacists to track safety recalls.
- Pharmacy contact info-Name, phone number, address. Keep this. If you have questions, this is who to call-not Google.
Why People Keep Getting It Wrong
It’s not your fault. Prescription labels are written by pharmacists for pharmacists, not for patients. A study by the National Institutes of Health found that 79% of people misread at least one instruction on their label. The biggest confusion? “Twice daily.” Many think it means “every 12 hours.” Others assume it means “morning and night,” which is often correct-but not always. If your doctor wants the drug evenly spaced, you need to know that.
People with low health literacy are 2.3 times more likely to make mistakes-even when the language is simple. And it’s not just about reading. If you’re stressed, tired, or in pain, your brain doesn’t process details well. That’s why it’s so important to ask for help.

How to Check Your Label Before You Take Anything
Before you swallow any pill, follow this simple 7-step check:
- Is your name on it? If it’s your partner’s name, don’t take it. Call the pharmacy immediately.
- Does the drug name match what your doctor said? If you were told you’re getting “blood pressure medicine,” but the label says “antibiotic,” stop. Ask.
- Is the strength the same as last time? If your last bottle was 5 mg and this one is 10 mg, it’s not a mistake-it’s a change. But you need to know why.
- Do you understand the instructions? If you’re unsure what “twice daily” means, ask the pharmacist to explain it in plain terms. Say: “Can you tell me exactly when to take this?”
- Are there any special warnings? “Avoid sunlight,” “Don’t drive,” “Take with food”-these aren’t suggestions. They’re safety rules.
- Is the expiration date still valid? If it’s expired, don’t take it. Throw it out or return it to the pharmacy for safe disposal.
- Do you know who to call with questions? Save the pharmacy’s number in your phone. Don’t wait until you feel sick to look it up.
What to Do If Something Doesn’t Look Right
Pharmacies make mistakes. Not often-about 1 in 5,000 prescriptions-but it happens. If the pill looks different from your last bottle, if the label has a typo, or if the instructions don’t match what your doctor told you-don’t guess. Call the pharmacy right away. Most will recheck your file and fix it at no cost.
Don’t be shy. Pharmacists expect these questions. In fact, they’re trained to answer them. A 2022 survey showed that patients who asked questions before leaving the pharmacy had 28% higher adherence rates. That means they took their meds correctly, got better faster, and avoided hospital visits.
What’s Changing on Prescription Labels
Labels are getting better. In Australia and the U.S., new rules require clearer language. “Take once a day” is now preferred over “qd.” “Every 12 hours” is clearer than “twice daily.” Some pharmacies now include QR codes on labels that link to short video instructions in plain language.
By 2025, most Australian pharmacies will offer digital label access through their apps. You’ll be able to see your meds, watch how to take them, set reminders, and even get alerts if a new drug interacts with something you’re already taking.
But technology won’t fix everything. The biggest problem isn’t the label-it’s the gap between what’s written and what’s understood. That’s why your voice matters. If something’s unclear, say so.
Final Tip: Make It a Habit
Don’t wait until you feel sick to check your labels. Make reviewing them part of your routine. Keep your prescriptions in one place. Write down the names and times you take them. If you’re on multiple meds, use a pill organizer. And always-always-ask your pharmacist to walk you through your new prescription before you leave the counter.
It takes two minutes. But those two minutes could keep you out of the hospital.
What should I do if I can’t read the label?
Ask your pharmacist for a large-print version or an audio explanation. Most pharmacies offer this for free. You can also request a written summary in plain language. Never guess what the label says-always get help.
Can I trust the generic version of my medication?
Yes. Generic drugs contain the same active ingredient as brand-name versions and are regulated to work the same way. The only differences are in fillers, color, or shape. If your generic looks different but has the same name and strength, it’s safe. Always check the DIN to confirm.
What if my prescription says ‘as needed’?
‘As needed’ means take it only when you have symptoms, not on a schedule. But it doesn’t mean ‘take as much as you want.’ There’s always a maximum daily limit listed somewhere on the label. If it’s not clear, ask your pharmacist for the exact number of doses allowed per day.
Why does my label have a barcode?
The barcode lets the pharmacy scan your prescription to confirm it’s the right drug, right strength, and right patient. It’s a safety check built into the system. You don’t need to do anything with it-just make sure the pharmacy scans it when you pick up your medicine.
What happens if I take expired medicine?
Most expired medicines don’t become dangerous-they just lose strength. But some, like antibiotics or insulin, can become ineffective or even harmful. Never take expired medicine if it’s for a serious condition. Return it to your pharmacy for safe disposal.
Can I split pills if the dose is too high?
Only if the pill has a score line (a groove down the middle) and your doctor or pharmacist says it’s safe. Not all pills can be split safely-some are time-released or coated. Never split pills without checking first.
How do I know if a new medication interacts with my other drugs?
Your pharmacist checks for interactions when filling your prescription. But if you’re taking new supplements, over-the-counter drugs, or herbal remedies, tell them. Many interactions happen because patients don’t mention everything they’re taking. Always update your pharmacist about changes.



