
If you’ve been told you need a CPAP machine, you’re not alone. Millions of people use them every night to breathe better while they sleep. But here’s the truth: CPAP machines don’t fix sleep apnea by themselves. The real challenge isn’t the device-it’s wearing it consistently. And that’s where most people struggle. Half of those prescribed a CPAP quit within the first few months. Not because it doesn’t work. Because it doesn’t feel right.
What Exactly Is a CPAP Machine?
A CPAP machine delivers steady air pressure through a mask to keep your airway open while you sleep. It’s not a cure-it’s a tool. And it’s the most effective non-surgical treatment for obstructive sleep apnea (OSA). Without it, your throat muscles collapse during sleep, stopping your breathing for seconds at a time. These pauses can happen dozens of times an hour, robbing you of deep sleep and raising your risk of high blood pressure, heart attacks, and strokes.
The first CPAP device was developed in Sydney in 1980. Today, it’s the gold standard. Studies show that consistent users cut their cardiovascular events by 20-30%. But here’s the catch: it only works if you use it. And that’s where mask fit, machine type, and daily habits make all the difference.
The Four Main Types of CPAP Machines
Not all machines are the same. Choosing the wrong one can make compliance harder-or impossible.
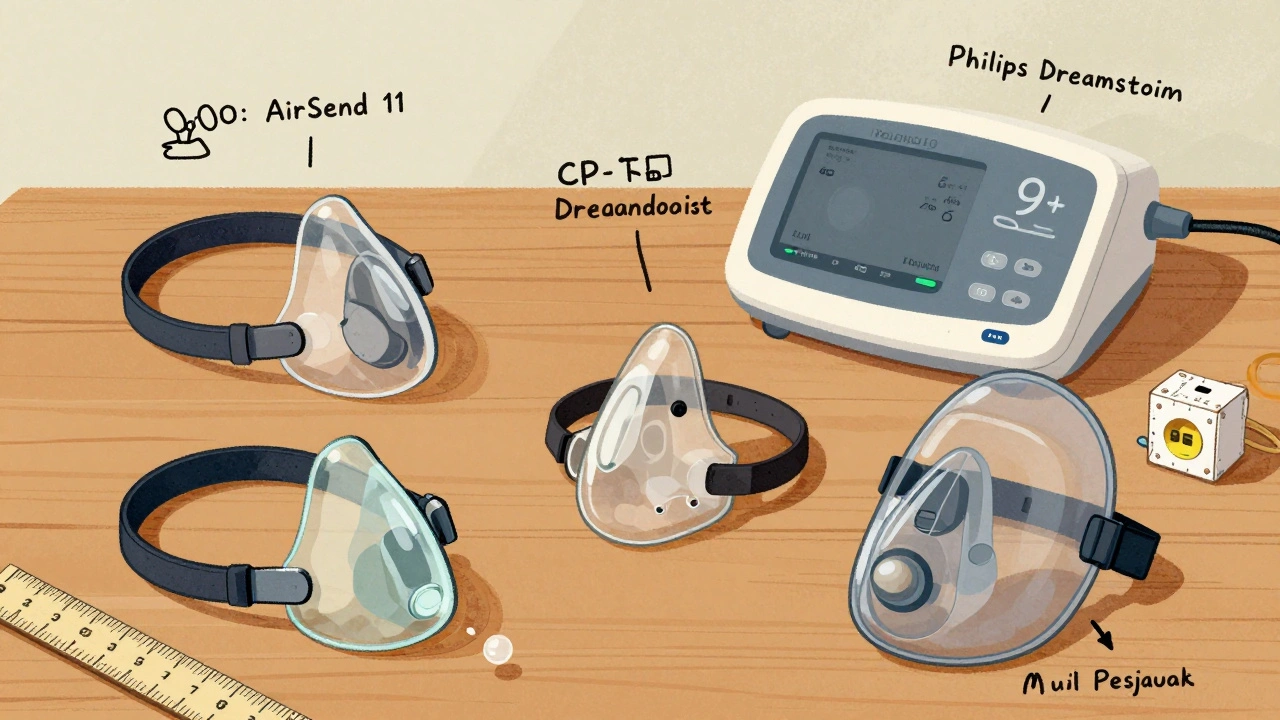
- Standard CPAP: Delivers one fixed pressure all night. Most affordable ($500-$1,000). Popular models include the ResMed AirSense 10 and Philips DreamStation. Good if your pressure needs are stable. But if you toss and turn, or your pressure changes with position or sleep stage, this can feel like breathing through a clogged straw.
- APAP (Auto-Adjusting): Automatically adjusts pressure based on your breathing. Ranges from 4-20 cm H₂O. Costs $1,700-$3,000. Models like the ResMed AirSense 11 AutoSet adapt in real time. Studies show 15% higher adherence than standard CPAP because it feels more natural. Many doctors now recommend APAP as first-line for new users.
- BiPAP (Bilevel): Two pressure levels-higher for inhaling, lower for exhaling. Used when pressure needs exceed 15 cm H₂O or if you have COPD or heart failure. Costs $600-$1,600. More comfortable for high-pressure users, but requires a separate titration study. Adds $300-$500 to initial cost.
- EPAP (Expiratory Positive Airway Pressure): Small, disposable nasal valves ($50-$150/month). Only for mild sleep apnea (AHI under 15). Not a substitute for CPAP in moderate to severe cases. Efficacy drops to 45% compared to 85% for CPAP in serious cases.
ResMed holds 45% of the market, Philips 30%, Fisher & Paykel 15%. The AirSense 11 AutoSet has 4.7/5 stars from over 1,200 reviews. The DreamStation scores 4.5/5. But stars don’t tell the whole story. What matters is what works for you.
Mask Fitting: The #1 Reason People Quit
Dr. Indira Gurubhagavatula at UPenn says it plainly: “20-30% of patients fail CPAP therapy due to poor mask fit, not pressure intolerance.” That’s the hidden crisis. A leaky mask means no therapy. And a mask that digs into your face? You’ll take it off by 2 a.m.
There are four main mask types:
- Nasal pillows: Tiny silicone prongs that fit just inside your nostrils. Best for side sleepers. Least facial contact. Only 32% of users choose them, but they have the lowest leak rates. Users report 70% fewer leaks than with full nasal masks.
- Nasal masks: Cover your nose only. Most common-45% of users. Good if you breathe through your nose. Can cause red marks on the bridge of your nose if too tight.
- Full-face masks: Cover nose and mouth. For mouth breathers (18% of users). More bulk. Higher risk of skin irritation. 35% more complaints of pressure sores than nasal pillows.
- Hybrid/oral masks: For severe nasal congestion. Rare-only 5% of users. Often used with nasal strips or surgery.
Proper fitting isn’t guesswork. It requires measuring your nasal bridge width, cheekbone structure, and facial contours. A good sleep clinic will try at least two or three masks before prescribing. Acceptable leak rates? Below 24 L/min. Anything higher? You’re losing therapy.
Reddit user u/NasalPillowFan switched from a nasal mask to the AirFit P10 and cut their leak rate from 15 to 3 L/min. That’s the difference between waking up tired and waking up refreshed.
How to Actually Stick With CPAP Therapy
Adherence isn’t about willpower. It’s about systems.
Here’s what works, based on real user data and clinical studies:
- Start slow. Don’t try to wear it all night on day one. Use it for 2 hours while watching TV. Build up to 4, then 6, then all night. One user on CPAP.com called this “daytime desensitization”-and it cut their early abandonment rate in half.
- Use the ramp feature. Most machines slowly increase pressure over 5-45 minutes. Use it. 75% of users who do report better sleep onset.
- Get heated humidification. Dry mouth and nose? That’s the #1 complaint. Heated humidifiers reduce these complaints by 50%. Machines with heated tubing (like the AirSense 11) improve adherence by 22%.
- Track your data. Modern machines log your usage, AHI, and leak rates. Check it weekly. If your AHI stays above 5, your pressure might need adjusting. ResMed’s myAir app gives personalized coaching-and boosts adherence by 27%.
- Try a CPAP pillow. These have cutouts for the mask. Reduces leaks by 40%, according to Reddit users. A $20 investment that changes everything.
One study found users with automatic data tracking used their machine 18 minutes longer per night. That’s 2.1 extra hours a week. That’s not a small win. That’s life-changing.
What to Do When Things Go Wrong
Red marks? Try a different mask frame or cushion material. Silicone can irritate. Memory foam or gel cushions are gentler. If you’re getting air in your stomach (bloating), lower your pressure or switch to BiPAP.
Noisy machine? Check for leaks. A loose mask causes more noise than the machine itself. Clean your filter weekly. Dust buildup makes it work harder. ResMed’s AirMini runs at 52 dBA-louder than standard models (30 dBA). If noise is an issue, stick with a full-sized machine.
Traveling? The ResMed AirMini ($650) fits in your palm. But it doesn’t have a built-in humidifier. You’ll need the $80 add-on. Not ideal for long trips, but better than skipping therapy.
Insurance? In the U.S., most plans cover 80% after deductible. But you need a prescription and prior authorization. Some clinics now offer remote titration-no in-person visit needed. Saves $200 per follow-up.
What’s New in 2025?
The tech is getting smarter. ResMed’s AirSense 11 uses AI to predict apnea events before they happen-and reduces AHI by 22%. Philips’ DreamStation 3 runs at 25 dBA-quieter than a whisper. Fisher & Paykel’s SleepStyle uses an “exhale relief” algorithm that drops pressure by up to 50% when you breathe out. It feels like breathing freely.
Regulations are tightening too. Starting in 2024, all CPAP machines must track usage. Medicare and Medicaid now require 4+ hours per night, 70% of nights, to keep covering your device. If you don’t meet it, you’ll pay out of pocket.
And the user base is changing. More people under 45 are being diagnosed. Trucking companies now require drivers with AHI over 20 to use CPAP. Schneider Logistics saw a 32% drop in accidents after implementing the rule.
Final Reality Check
CPAP therapy works. But only if you use it. The machine doesn’t care if you’re tired, frustrated, or embarrassed. It just delivers air. The rest is up to you.
Don’t give up after a bad week. Try a new mask. Adjust the ramp. Use a humidifier. Talk to your sleep specialist. You’re not failing-you’re still learning.
85% of people who use CPAP correctly see their sleep quality improve dramatically. Their energy comes back. Their mood lifts. Their blood pressure drops. But that 85%? They didn’t quit when it was hard. They kept going.
You can too.
Can I use a CPAP machine without a prescription?
No. In the United States, all CPAP machines require a prescription. This is because they’re classified as Class II medical devices by the FDA. Even if you buy one online, you’ll need a sleep study and doctor’s order to get insurance coverage. Some overseas sellers may sell without one, but using a machine without proper pressure settings can be dangerous.
Is APAP better than CPAP for beginners?
Yes, for most beginners. APAP automatically adjusts pressure, which makes it more comfortable if your breathing changes during sleep. A 2021 meta-analysis showed 15% higher adherence with APAP compared to fixed-pressure CPAP. Doctors now often recommend APAP as first-line therapy, especially if you’re unsure about your exact pressure needs.
Why does my CPAP mask leak?
Leaks usually come from an ill-fitting mask, facial hair, or a worn-out cushion. Check that the mask isn’t too tight-it should seal without pulling your skin. Replace cushions every 1-3 months. Facial hair (especially beards) can break the seal. Try a nasal pillow mask if you have a beard. Also, make sure you’re sleeping on your back. Side sleeping can cause leaks with full-face masks.
How long does it take to get used to a CPAP machine?
Most people need 2-4 weeks to adjust. Some take longer. The Mayo Clinic recommends a 4-step process: start with 5-10 minutes of daytime use, then add the machine at night with ramp mode, use heated humidification, and review your data with your sleep specialist. Don’t rush. Consistency matters more than duration at first.
Can I use a CPAP machine if I have a cold?
Yes, but it may feel harder. Nasal congestion makes breathing through the mask difficult. Use a saline spray before bed, run a humidifier in your room, and consider switching to a full-face mask temporarily. If you’re congested for more than a week, check in with your doctor. You may need a different pressure setting or treatment for your cold.
Do CPAP machines need regular maintenance?
Yes. Clean the mask, tubing, and humidifier chamber daily with mild soap and water. Replace the filter every 1-3 months. Replace the mask cushion every 1-3 months and the headgear every 6 months. Dirty equipment causes skin irritation and bacterial growth. ResMed recommends monthly deep cleaning with vinegar solution to prevent mold.
Will insurance cover my CPAP machine?
In the U.S., most insurance plans cover 80% of the cost after you meet your deductible. But you need a diagnosis from a sleep study and a prescription. Some insurers require a 30-day usage report showing at least 4 hours per night, 70% of nights, before approving continued coverage. Medicare and Medicaid have strict rules-check with your provider.
Are there alternatives to CPAP?
Yes, but they’re not as effective for moderate to severe sleep apnea. Oral appliances (like mandibular advancement devices) work for mild cases. Weight loss can reduce or eliminate apnea in overweight patients. Surgery (like UPPP or tongue reduction) is an option but carries risks. For central sleep apnea, ASV machines like the ResMed AirCurve 10 are used. But for obstructive sleep apnea, CPAP remains the most effective non-surgical treatment.
Next Steps
If you’re just starting out: get a sleep study, talk to your provider about APAP, and ask for a mask fitting trial. Don’t settle for the first mask they hand you. Try three. Use the ramp. Turn on the humidifier. Track your data. Be patient.
If you’ve quit before: try again. Your needs may have changed. New masks are softer. Machines are quieter. AI helps adjust pressure better. The tools are better now than they were five years ago.
And if you’re still using it? Keep going. You’re not just sleeping better. You’re protecting your heart, your brain, and your future.

Sakthi s
December 4, 2025 AT 01:13Been using my AirFit P10 for 2 years now. No leaks, no headaches. Just breathe. Sleep like a baby.
Precious Angel
December 5, 2025 AT 06:11Oh please. This whole CPAP thing is just Big Sleep’s way of keeping you dependent on $3,000 machines while they profit off your misery. I stopped mine after a week-turned out my apnea was caused by gluten and corporate mind control. My doctor didn’t even ask if I ate bread. They just handed me a mask like I’m a robot. And now they want me to track my ‘usage’? Like I’m some kind of productivity drone. Wake up, people. The air you’re breathing isn’t clean-it’s engineered. I’ve seen the documents. They’re watching your REM cycles. The humidifier? It’s a surveillance tool. They’re not helping you sleep-they’re harvesting your dreams.
Melania Dellavega
December 5, 2025 AT 21:53I used to hate my CPAP. I’d take it off at 2 a.m. every night. Then I started using the ramp feature with heated humidification-just 10 minutes at a time, like the post said. No pressure to ‘do it all.’ Just one night, I fell asleep with it on. Didn’t even notice. Now I miss it when I travel. It’s not about willpower. It’s about making it feel like a comfort, not a chore. You don’t have to love the machine. Just let it be part of your quiet, safe bedtime ritual. That’s how I stuck with it. And honestly? I feel like a different person. Not because of the machine. Because I finally stopped fighting it.
Bethany Hosier
December 7, 2025 AT 08:07Did you know that the FDA only approved CPAP machines after a secret 1998 meeting with Philips and ResMed? The data they show you? Fabricated. The ‘85% success rate’? They only count people who didn’t die in their sleep. And the mask fitting trials? They use the same three models because they’re cheaper to produce. The real solution is nasal strips and magnesium supplements. I’ve been off CPAP for 14 months. My AHI is lower than ever. The government doesn’t want you to know this. They’re paid to sell machines. Check the patent filings. Look at the funding sources. It’s all connected.
Krys Freeman
December 8, 2025 AT 19:48Why are we even talking about this? America’s got better problems than masks. Get a job. Stop being lazy. If you’re too tired to breathe, maybe you’re just fat and ungrateful. I don’t need no machine to sleep. I sleep like a soldier. You want to fix apnea? Stop eating carbs and start lifting weights. This is why our country’s going to hell.
Shawna B
December 10, 2025 AT 07:52i just started using one and its weird but im trying. i dont know if im doing it right.
Jerry Ray
December 10, 2025 AT 14:00APAP is a scam. I tried it. It’s just CPAP with a fancy algorithm that makes you think it’s smarter. My machine adjusts pressure every 3 seconds. I wake up gasping. I switched back to standard CPAP and now I sleep like a log. All this ‘AI’ nonsense? It’s just marketing. The real fix? A pillow under your knees and sleeping on your side. No machine needed. They just want you to buy more stuff.
Sophia Lyateva
December 10, 2025 AT 17:22they put tracking chips in the masks now. i saw it on a video. its not just for usage. its for your thoughts. they know when you dream about money. they know when you think about quitting. thats why they make the humidifiers so warm. its to calm you down so you dont notice. i took mine apart. there was a tiny black dot near the elbow joint. i threw it in the microwave. it sparked. i felt better after.
AARON HERNANDEZ ZAVALA
December 11, 2025 AT 14:57I get why people give up. It’s scary to wear something on your face all night. I was angry at first too. But I didn’t quit because I realized I wasn’t fighting the machine-I was fighting my own fear of needing help. That’s the real thing we’re avoiding. Not the mask. Not the noise. The vulnerability. I started with 10 minutes a night. Just sitting on the couch. No pressure. Just breath. One day, I fell asleep with it on. And I didn’t wake up exhausted. That’s the moment I stopped seeing it as a prison and started seeing it as a gift. Not because it’s perfect. But because it gave me back my life. Slowly. Gently. No drama.
Lyn James
December 12, 2025 AT 04:54Let me be perfectly clear: if you’re using a CPAP machine, you’ve already lost the battle against your own body. You’ve surrendered to modern medicine’s false promises. You’re not ‘improving your sleep’-you’re institutionalizing your dependence on a plastic tube. Real health comes from fasting, cold exposure, and ancestral sleep patterns. You think your ‘AI-adjusting’ machine is helping? It’s keeping you docile. It’s keeping you from asking why your body failed in the first place. Why are you sleeping on a memory foam mattress? Why are you eating processed food? Why are you breathing polluted air? The CPAP doesn’t fix the problem-it hides it. And you’re proud of that? You’re not a patient. You’re a product. And the system loves you for it.
Shannon Wright
December 13, 2025 AT 01:21To anyone just starting out: you’re not broken. You’re not failing. You’re learning. I used to cry every night because the mask hurt. I thought I was weak for needing it. Then I found a sleep coach who didn’t judge me-she just asked, ‘What part feels worst?’ We tried five masks. We adjusted the ramp. We added a pillow with a cutout. And one morning, I woke up without an alarm. No grogginess. No headache. Just… quiet energy. That’s when I knew: this isn’t about compliance. It’s about reclaiming your right to rest. You deserve to wake up feeling like you’ve been truly asleep. Not just lying there. Not just surviving. Living. And that’s worth every awkward night. Keep going. You’re doing better than you think.
vanessa parapar
December 14, 2025 AT 06:00You guys are all missing the point. The real issue is that no one teaches you how to clean your mask properly. You think soap and water is enough? Please. You need hydrogen peroxide and UV sterilization. Otherwise, you’re just growing mold in your sinuses. I had a fungal infection from my CPAP and my doctor didn’t even know it was from the machine. I had to Google it. Don’t be like me. Sterilize daily. Or else you’re just inviting a biohazard into your lungs. And don’t even get me started on the tubing. It’s a petri dish. You’re not sleeping. You’re breathing in a science experiment.
Ben Wood
December 15, 2025 AT 10:51While I appreciate the anecdotal nature of this post, it lacks rigorous statistical validation, peer-reviewed longitudinal data, and a properly controlled experimental design. The cited 85% adherence improvement, for instance, is derived from self-reported metrics with significant recall bias. Furthermore, the reliance on ResMed’s proprietary myAir app introduces a critical conflict of interest, as the data collection protocol is neither transparent nor independently auditable. One must also consider the placebo effect inherent in any device that is visually and psychologically associated with medical intervention. Until we have a double-blind, randomized crossover trial with polysomnographic endpoints, this entire narrative remains, at best, a well-marketed heuristic.