Most people don’t realize that the little white pill they pick up at the pharmacy might be the exact same medicine as the expensive brand-name version they’ve been taking for years. The difference? The price tag. Generic drugs aren’t cheaper because they’re weaker or lower quality-they’re cheaper because they don’t carry the cost of marketing, patents, or clinical trials. But here’s the real question: are they just as safe and effective? And should you always choose them?
They’re the Same Medicine, Just Without the Brand
Generic drugs contain the same active ingredients as their brand-name counterparts. That means if you’re taking lisinopril for high blood pressure, the generic version has the same molecule, the same strength, and works the same way in your body. The Food and Drug Administration (FDA) is the agency that makes sure of this. Before a generic drug hits the shelf, it must prove it delivers the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. This is called bioequivalence. The FDA allows a variation of only 80% to 125% in absorption-meaning even if there’s a tiny difference, it’s not enough to affect how well the drug works.
Think of it like two different brands of aspirin. One says "Bayer," the other says "Store Brand." Both have acetylsalicylic acid as the active ingredient. They do the same job. The only real difference? The price-and maybe the color or shape of the pill.
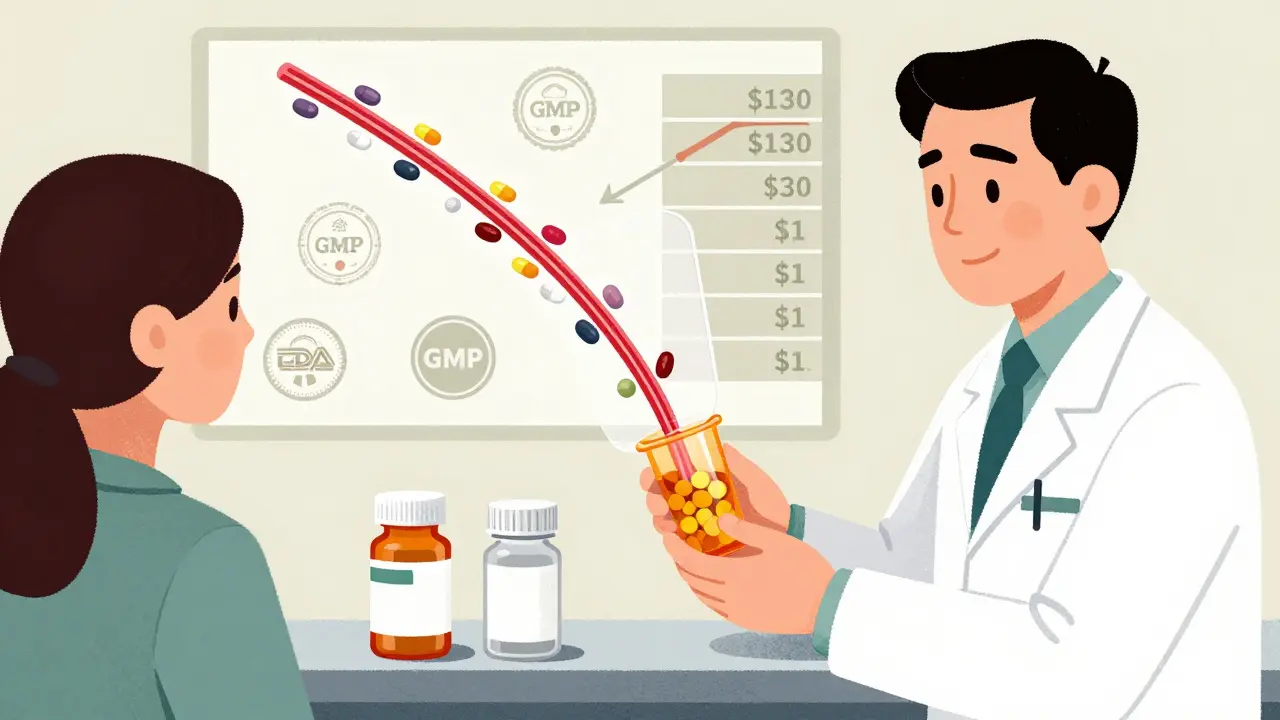
Why Are Generics So Much Cheaper?
Brand-name drugs cost a lot because their makers spend years and billions developing them. The FDA estimates the average cost to bring a new drug to market is around $2.6 billion. That includes research, testing on animals, clinical trials with humans, and years of regulatory review. Once approved, the company gets a patent-usually 20 years-that lets them be the only one selling that drug. During that time, they set high prices to recover their investment.
Generic manufacturers don’t have to repeat all that. Once the patent expires, they can copy the formula. All they need to prove is bioequivalence. That cuts their costs dramatically. As a result, generics typically cost 80% to 85% less than brand-name drugs. According to GoodRx, the average savings in 2022 was 82.5%. For some drugs, like atorvastatin (Lipitor), the price dropped from $130 a month to under $1 after generics entered the market.
What’s Different About Generics?
While the active ingredient is identical, generics can differ in the inactive ingredients. These include fillers, dyes, preservatives, and binders-things that help the pill hold its shape or make it easier to swallow. That’s why a generic version of your medication might look different: maybe it’s a different color, size, or shape. It’s not a different drug. It’s just packaged differently.
For most people, these differences don’t matter. But if you have allergies-say, to red dye or lactose-you should check the inactive ingredients. The FDA requires manufacturers to list them on the packaging, so it’s easy to compare.
There’s also a myth that generics are made in worse factories. That’s not true. Both brand-name and generic drugs must meet the same Good Manufacturing Practice (GMP) standards. The FDA inspects both types of facilities the same way. In fact, many brand-name companies also make generic versions of their own drugs.
When Generics Might Not Be the Best Choice
There’s one big exception: narrow therapeutic index (NTI) drugs. These are medications where even a small change in blood levels can cause serious problems. Examples include warfarin (a blood thinner), levothyroxine (for thyroid conditions), and some seizure medications like phenytoin or levetiracetam.
For these drugs, the FDA says generics are still approved and safe. But some doctors and patients report issues when switching between different generic brands. A 2017 study found that switching between different generic versions of levetiracetam was linked to a 32% higher risk of seizure-related hospital visits. That doesn’t mean generics are dangerous-it means consistency matters. If you’ve been stable on one generic brand, switching to another might throw off your balance.
The American Academy of Neurology and other medical groups recommend sticking with the same manufacturer for NTI drugs when possible. If you’re on one of these medications and you notice changes in how you feel after a refill-like more fatigue, mood swings, or seizures-ask your pharmacist: "Did I get the same generic as last time?" You can also ask your doctor to write "dispense as written" on your prescription to prevent automatic switches.
What Do Patients Really Experience?
Most people don’t notice any difference. A review of 250,000 patient reviews on Drugs.com found that 87% reported no change in effectiveness or side effects when switching from brand to generic for common drugs like metformin or lisinopril. On Reddit, users shared stories of saving hundreds a month after switching from Humira to its biosimilar-sometimes paying $10 instead of $460.
But the negative experiences? They’re real-and they cluster around NTI drugs. A 2023 social media analysis found that 42% of patient complaints about generics were about thyroid meds like Synthroid. People reported feeling sluggish, gaining weight, or having heart palpitations after switching to a different generic version. These aren’t placebo effects. These are measurable changes in hormone levels.
That’s why Medicare beneficiaries who use these drugs often stick with one brand-even if it costs more. Sixty-eight percent said cost was their main reason for choosing generics, but 22% said their doctor’s advice was the deciding factor.
How to Make the Right Choice
Here’s how to navigate this without confusion:
- Ask your doctor if your drug is a narrow therapeutic index (NTI) medication. If it is, talk about whether staying on one manufacturer matters for you.
- Check your pill. If it looks different, ask your pharmacist: "Is this the same generic I got last time?"
- Use tools like GoodRx to compare prices. Sometimes the brand-name version is cheaper than a particular generic-especially with coupons or pharmacy discounts.
- If you’re on a Medicare Part D plan, use the Plan Finder tool to see which generics are covered and at what cost.
- Keep a list of the generic manufacturer’s name (often printed on the bottle). If you have a bad reaction, you’ll know which one to avoid.
The FDA’s Orange Book is another useful resource. It lists every approved generic and its therapeutic equivalence rating. You can look up your drug and see which generics are rated "AB"-meaning they’re considered interchangeable.
The Bigger Picture: Why This Matters
Generic drugs aren’t just about saving money on your prescription-they’re saving the whole healthcare system billions. From 2007 to 2016, generics saved the U.S. system $1.67 trillion. Medicare saved $77 billion. Medicaid saved nearly $38 billion. In 2022, 90% of all prescriptions filled in the U.S. were for generics. But they only made up 26% of total drug spending.
That’s the power of competition. When multiple companies make the same drug, prices drop fast. And when big drugs like Humira lose their patents, biosimilars (generic versions of complex biologic drugs) enter the market and drive prices down even further.
But challenges remain. In 2022, the FDA reported 178 active shortages of generic drugs-many due to manufacturing issues or raw material shortages. And while U.S. facilities are inspected regularly, a 2023 government report found that 18% of foreign generic drug plants had at least one FDA inspection finding, compared to just 8% of domestic ones.
Still, the trend is clear: generics are here to stay. The World Health Organization predicts that by 2030, 70% of all prescriptions worldwide will be for generic drugs.
Final Takeaway: Trust the Science, Stay Aware
For most people, generic drugs are just as safe and effective as brand-name ones-and they save a ton of money. The FDA, major medical groups, and decades of research back this up. But if you’re on a drug where tiny changes in dosage matter-like thyroid, blood thinners, or seizure meds-don’t assume all generics are the same. Stick with the one that works for you. If your pharmacy switches it without telling you, speak up. Your health isn’t a cost-cutting experiment.
Generics aren’t second-rate. They’re smart medicine. And if you’re paying full price for a brand-name drug when a generic exists, you’re probably overpaying.
Are generic drugs as effective as brand-name drugs?
Yes, for the vast majority of medications, generic drugs are just as effective as brand-name versions. The FDA requires them to have the same active ingredient, strength, dosage form, and bioequivalence. Studies show no meaningful difference in outcomes for drugs like blood pressure medications, antidepressants, or antibiotics. The only exceptions are narrow therapeutic index drugs, where consistency in manufacturer matters.
Why do generic pills look different from brand-name ones?
By law, generic drugs can’t look exactly like the brand-name version, even if they contain the same active ingredient. This is to avoid trademark infringement. So, generics may differ in color, shape, size, or markings. But these differences are only cosmetic. The medicine inside is the same. If you’re unsure, check the label or ask your pharmacist.
Can I switch between different generic brands?
For most drugs, yes. But if you’re taking a narrow therapeutic index drug-like warfarin, levothyroxine, or certain seizure meds-it’s best to stick with the same manufacturer. Switching between different generic versions can cause small changes in how your body absorbs the drug, which may lead to side effects or reduced effectiveness. Always ask your pharmacist if your refill is from the same company as before.
Are generic drugs made in lower-quality facilities?
No. The FDA inspects generic and brand-name manufacturing facilities using the same standards. Both must follow Good Manufacturing Practice (GMP) rules. In fact, many brand-name companies also produce generic versions of their own drugs. While some generics are made overseas, the FDA conducts inspections worldwide and has the same authority over all facilities.
How do I know if my drug has a generic version?
Ask your pharmacist or doctor. You can also check the FDA’s Orange Book online, which lists all approved generic drugs and their therapeutic equivalence ratings. Most brand-name drugs have generics once their patent expires-usually 10 to 12 years after launch. Newer drugs may still be under patent protection, so no generic is available yet.
Should I always choose the cheapest generic?
Usually, yes-but not always. For most medications, the cheapest generic is fine. But for narrow therapeutic index drugs, it’s better to stick with the one that works for you, even if it costs a bit more. Also, sometimes the brand-name version is discounted so heavily through coupons or insurance that it’s cheaper than a particular generic. Always compare prices using tools like GoodRx before filling your prescription.
What to Do Next
If you’re taking a brand-name drug, ask your pharmacist: "Is there a generic version?" If there is, ask how much it costs compared to your current prescription. You might be surprised. If you’re on a thyroid, blood thinner, or seizure medication, check your last refill to see which manufacturer made it. Write that name down. If your next refill is different, ask why. Don’t let a switch happen without your knowledge.
Generic drugs are one of the biggest wins in modern medicine. They make life-saving treatments affordable. But like any tool, they work best when you understand how to use them.




Wren Hamley
January 2, 2026 AT 20:23Okay, but let’s be real-bioequivalence is a legal loophole dressed up as science. 80-125% absorption range? That’s a 45% swing. If I take two different generics of the same drug, one might as well be a placebo and the other a full dose. And nobody talks about how the FDA inspects maybe one factory every five years. You think your $2 lisinopril is made in the same sterile environment as the $130 version? Lol. 🤡
Angela Fisher
January 3, 2026 AT 01:54They’re lying. EVERYTHING is controlled by Big Pharma and the FDA. They let generics in so you’ll think you’re saving money, but then they switch the inactive ingredients to make you dependent on their brand. Lactose? Dyes? They’re all designed to mess with your gut microbiome and keep you docile. I stopped taking all generics after my thyroid went haywire. Now I buy mine from Canada. They don’t lie there. 🇨🇦💔
Neela Sharma
January 4, 2026 AT 02:11My grandma in Delhi takes generic insulin. She’s 78. Lives in a village. No insurance. No doctor visits. Just a local pharmacist who gives her the same vial every month. She’s alive. Stable. Happy. Meanwhile, my cousin in Chicago pays $600 for the same thing. Who’s the real science here? 🌏❤️
Lori Jackson
January 5, 2026 AT 05:33How is it that we live in a society where a person’s health is contingent on their ability to spell ‘bioequivalence’? The fact that we even have to debate whether a pill with identical active ingredients is ‘safe’ is a moral failure. You don’t need a PhD to understand that if two things contain the same molecule, they do the same thing. The real tragedy? People are being gaslit into paying more for a placebo with a logo. 🤦♀️
Philip Leth
January 5, 2026 AT 22:10Man, I used to pay $400/month for Humira. Switched to the biosimilar. Paid $12. Same injection. Same results. My rheumatoid arthritis didn’t care about the label. My wallet did. If you’re still buying brand-name for no reason, you’re just funding corporate greed. Not cool.
Kerry Howarth
January 6, 2026 AT 16:24For NTI drugs, consistency matters. If your levothyroxine brand changed and you feel off, it’s not in your head. Track the manufacturer name on the bottle. Ask for ‘dispense as written.’ Your endocrine system isn’t a cost-center.
JUNE OHM
January 7, 2026 AT 06:04They’re all made in China. You think the FDA checks every batch? LOL. My cousin’s generic Xanax made him hallucinate. He thought his cat was a government drone. That’s not a coincidence. They’re cutting corners. And you’re letting them. 🇨🇳💊
Joy F
January 8, 2026 AT 12:45Let’s deconstruct the hegemony of pharmaceutical capitalism. The FDA’s ‘bioequivalence’ standard is a neoliberal construct designed to commodify biological integrity. The pill’s molecular identity is irrelevant-what matters is the ontological rupture caused by corporate abstraction. You’re not taking medicine. You’re consuming a signifier of health, stripped of its sacred essence. The color of the pill? That’s the color of your alienation.
And yet-
And yet, I still take the generic. Because I’m trapped in the system. I’m complicit. I know this. I’m a walking contradiction. But isn’t that the human condition? We scream into the void, then pay $2 for the void’s solution.
Angela Goree
January 8, 2026 AT 16:25Wait-I just checked my last prescription. The generic I got last month was made by Teva. This month? It’s Mylan. I didn’t ask. I just took it. And now I’m having panic attacks. Is this what they mean by ‘switching’? I’m not crazy-I’m being experimented on. Someone call the FDA. I need to know who made this pill. I need to know if they’re Chinese. I need to know if they’re lying. I need to know if I’m safe.
Shanahan Crowell
January 10, 2026 AT 10:03Don’t let fear of the unknown stop you from saving money. Most people never notice a difference. But if you’re on warfarin or thyroid meds? Pay attention. Write down the maker. Ask questions. Be your own advocate. You’re worth the effort. And hey-if you’re scared, talk to your pharmacist. They’re not just cashiers. They’re your health allies.
Ian Ring
January 12, 2026 AT 08:54Interesting piece. I’ve been on generic metformin for 7 years. No issues. My GP says generics are the backbone of sustainable healthcare. But I do wonder-why does the FDA allow such a wide bioequivalence window? 80–125% feels… generous. I’d like to see more transparency on manufacturing locations. Not out of paranoia-just accountability.
Haley Parizo
January 12, 2026 AT 17:44Generics are the silent revolution. They’re the reason a single mom in Ohio can afford her antidepressants. They’re why a veteran in Texas can manage his diabetes without choosing between insulin and groceries. The real villain isn’t the generic pill-it’s the system that lets corporations profit from human suffering. If you’re still paying full price for a drug that has a generic? You’re not being smart. You’re being exploited.
Ian Detrick
January 13, 2026 AT 19:29My dad’s on levothyroxine. Switched from Synthroid to a generic. TSH went from 2.1 to 6.8. He felt like a zombie. We switched back. Now he pays $15 more a month. Worth it. Don’t gamble with your hormones.