Lithium Toxicity Risk Calculator
Your Current Lithium Level
Medications You're Taking
Risk Assessment
Why Lithium Can Turn Dangerous With Common Medications
Lithium has been used for over 50 years to treat bipolar disorder, and it still works better than most alternatives at preventing suicide. But it’s not a safe drug if you don’t know how to use it. The difference between healing and hospitalization is tiny-just 0.3 mmol/L. A normal level is between 0.6 and 1.2 mmol/L. Go above 1.5, and you’re in danger. Hit 2.5 or higher, and you could need dialysis.
Here’s the problem: two of the most common medications people take-diuretics and NSAIDs-can push lithium levels into the toxic range without warning. And many patients don’t even realize they’re at risk.
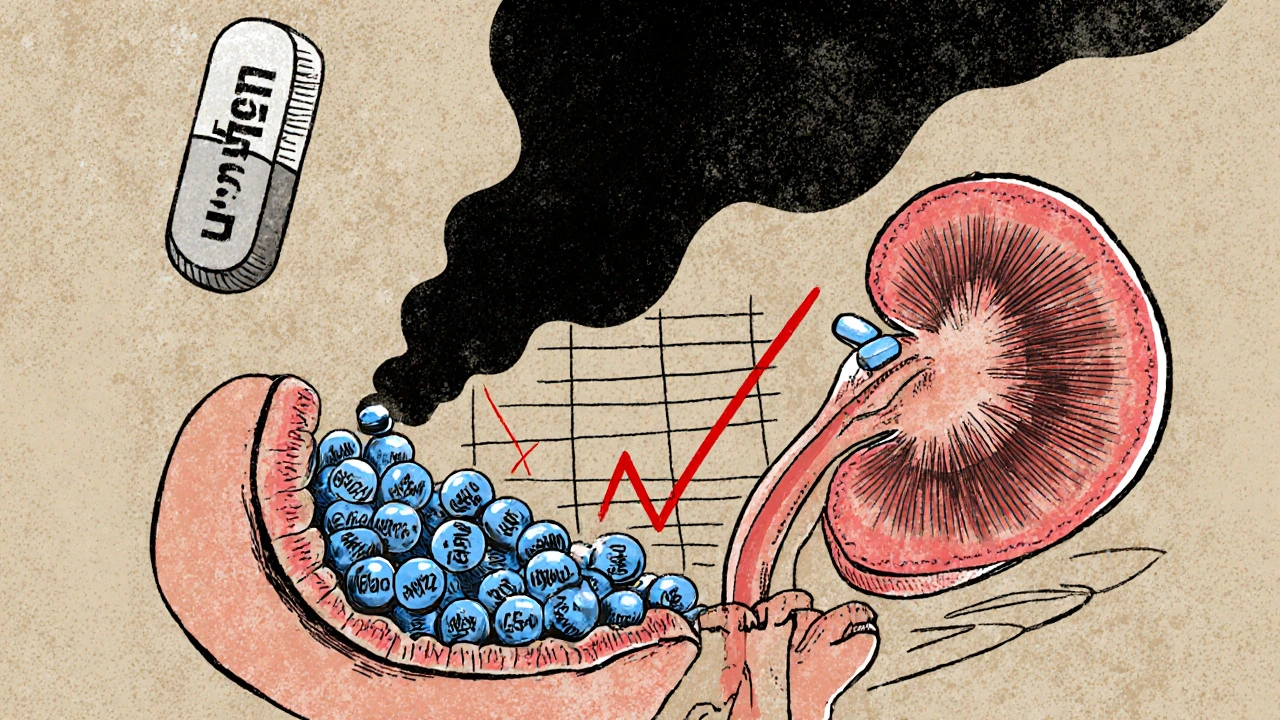
How Lithium Works (And Why Your Kidneys Are the Weak Spot)
Lithium doesn’t get broken down by your liver. It doesn’t bind to proteins. It just floats in your blood and gets filtered by your kidneys. What makes it dangerous is that your kidneys reabsorb about 80% of it, meaning most of what you take stays in your body. That’s fine when everything’s working normally.
But if your kidneys start holding onto more lithium-because of another drug, dehydration, or kidney decline-levels climb fast. And because lithium has such a narrow window between helpful and harmful, even a small change can cause serious symptoms: tremors, confusion, nausea, muscle weakness, or seizures. In extreme cases, it can be fatal.
Diuretics: The Silent Lithium Boosters
Diuretics are water pills. They help with high blood pressure and swelling. But they also interfere with how your kidneys handle lithium. Not all diuretics are equal, though.
Thiazide diuretics like hydrochlorothiazide and bendroflumethiazide are the worst offenders. They cause lithium levels to jump by 25% to 40%, sometimes even four times higher. That’s not rare-it happens in 75% to 85% of patients taking them with lithium. Why? Because thiazides act on the part of the kidney where lithium gets reabsorbed. Less sodium excretion means more lithium stays behind.
Loop diuretics like furosemide are less risky. They raise lithium levels by only 10% to 25%, and mostly in people who already have kidney problems. That’s why doctors sometimes choose furosemide over thiazides if a patient on lithium needs a diuretic. But even furosemide isn’t safe without monitoring.
Here’s what happens in real life: a 72-year-old woman on lithium for bipolar disorder started taking hydrochlorothiazide for high blood pressure. Her lithium level went from 0.8 mmol/L (safe) to 1.9 mmol/L (toxic) in just seven days. She ended up in the hospital with confusion and vomiting. This isn’t an outlier. It’s textbook.
NSAIDs: The Over-the-Counter Threat
NSAIDs-like ibuprofen, naproxen, and indomethacin-are everywhere. You can buy them at the grocery store. People take them for headaches, back pain, arthritis. But they’re one of the most common causes of lithium toxicity.
NSAIDs block prostaglandins, chemicals your kidneys use to keep blood flow steady. Less blood flow means less lithium gets filtered out. The result? Lithium builds up. The effect is dose-dependent:
- Indomethacin: 20-40% increase
- Piroxicam: 20-30% increase
- Naproxen: 15-25% increase
- Ibuprofen: 15-20% increase
- Celecoxib: only 5-10% increase
That last one matters. If someone on lithium absolutely needs an NSAID, celecoxib is the safest choice. But even then, you still need to check lithium levels.
One case in 2013 involved a patient who took 600 mg of ibuprofen three times a day for back pain. His lithium level shot up to 2.8 mmol/L. He needed hemodialysis. Even after his blood levels dropped, he stayed at risk because lithium lingers inside cells longer than it shows up in blood tests. That’s why symptoms can keep getting worse even after the level looks normal.
And here’s the scary part: many people don’t tell their doctor they’re taking ibuprofen or naproxen. They think it’s just an OTC painkiller. But for someone on lithium, it’s a hidden danger.
Other Medications That Can Interfere
It’s not just diuretics and NSAIDs. Other common drugs also raise lithium levels:
- ACE inhibitors (like lisinopril): 15-25% increase
- ARBs (like valsartan): 10-20% increase
- Calcium channel blockers (like verapamil): don’t raise lithium levels much, but can make tremors and tinnitus worse
These drugs affect kidney blood flow or sodium balance, which indirectly impacts lithium clearance. The risk isn’t as high as with thiazides or indomethacin, but it’s still real. And if you’re taking more than one of these together, the risk multiplies.
What You Need to Do: Monitoring and Safety Steps
If you’re on lithium and your doctor prescribes a new medication, ask: “Will this affect my lithium level?” Don’t assume it’s safe just because it’s common.
Here’s what works in practice:
- Check lithium levels before starting any new drug-especially diuretics, NSAIDs, or blood pressure meds.
- Test again 4-5 days after starting the new medication. That’s when levels peak.
- Keep checking weekly for the first month, then every 3-6 months if stable.
- Reduce lithium dose by 15-25% if you must stay on a thiazide or strong NSAID. Your doctor should adjust this.
- Never start an OTC painkiller without telling your psychiatrist or pharmacist.
- Stay hydrated. Dehydration makes lithium toxicity worse. Drink water, especially in hot weather or when exercising.
Some patients now use home testing devices like LithoLink™, which lets them check their levels at home and send results to their doctor. It’s not perfect, but it helps people stay on track.

What to Do If You Think You’re Toxic
Don’t wait for a blood test. If you start feeling off-shaky, confused, nauseous, dizzy, or having trouble speaking-get help immediately. These aren’t side effects. They’re warning signs.
Severe toxicity (level above 2.5 mmol/L) with mental changes or seizures requires emergency dialysis. Lithium doesn’t leave the body quickly. It takes multiple dialysis sessions to clear it fully.
Even if your level drops, symptoms can continue. That’s because lithium stays inside your brain and nerve cells longer than in your blood. So treatment isn’t just about numbers-it’s about how you feel.
Why Lithium Is Still Worth It-If You Manage the Risk
Lithium reduces suicide risk by 44% compared to no treatment. No other mood stabilizer does that. For many people, it’s the only thing that keeps them alive.
The problem isn’t lithium. It’s the lack of awareness. A 2021 study found that only 45% of doctors follow the recommended monitoring schedule after starting a new drug. That’s not enough.
The future is better monitoring, smarter dosing, and new lithium formulations that don’t rely so heavily on kidney function. But right now, the safest way to use lithium is to know the risks-and act on them before it’s too late.
What to Ask Your Doctor
If you’re on lithium, make sure you ask these questions:
- Is this new medication safe with lithium?
- When should I get my next lithium level checked?
- Should I reduce my lithium dose if I start this drug?
- What symptoms should I watch for?
- Is there a safer alternative to this drug?
Can I take ibuprofen if I’m on lithium?
You can, but it’s risky. Ibuprofen can raise lithium levels by 15-20%. If you need it, take the lowest dose for the shortest time. Get your lithium level checked 4-5 days after starting. Avoid daily use. Celecoxib is a safer NSAID option if you need long-term pain relief.
Why are thiazide diuretics more dangerous than furosemide with lithium?
Thiazides act on the part of the kidney where lithium is reabsorbed. They reduce sodium excretion, which causes your kidneys to hold onto more lithium. Furosemide works higher up in the kidney and doesn’t affect lithium reabsorption as much. That’s why furosemide is often preferred if a patient on lithium needs a diuretic.
How often should lithium levels be checked when starting a new drug?
Check lithium levels 4-5 days after starting any new medication that affects the kidneys-like diuretics, NSAIDs, or ACE inhibitors. Then check again weekly for the first month. After that, go back to every 3-6 months if stable. Never skip a check just because you feel fine.
Can herbal supplements interact with lithium?
Yes. There’s not enough data to say any herbal supplement is safe with lithium. Some, like St. John’s Wort, can affect kidney function or alter drug metabolism. Others, like ginger or ginkgo, may increase bleeding risk when combined with lithium’s side effects. Always tell your doctor about every supplement you take.
What happens if lithium levels are too high?
Mild toxicity (1.5-2.0 mmol/L) causes nausea, tremors, and dizziness. Moderate (2.0-2.5 mmol/L) can lead to confusion, slurred speech, and muscle weakness. Severe toxicity (above 2.5 mmol/L) causes seizures, coma, or cardiac issues. At this point, you need emergency treatment, often including dialysis. Symptoms matter more than the number-don’t wait for a test if you feel wrong.



Dion Hetemi
November 20, 2025 AT 01:23And don't get me started on how half the patients don't even know their own lithium levels. You wouldn't drive a car without checking the fuel gauge-why are we treating brain chemistry like it's a magic trick?
river weiss
November 21, 2025 AT 23:41Furthermore, the notion that 'it's just an OTC painkiller' reflects a dangerous cultural normalization of pharmacological risk. Celecoxib is not a 'safer alternative'-it is a risk-mitigation strategy. And hydration? It's not advice-it's a physiological imperative.
Brian Rono
November 22, 2025 AT 23:39And don’t even get me started on home testing devices. LithoLink? That’s not innovation-that’s a Band-Aid on a hemorrhage. If your system requires patients to self-test just to stay alive, you’ve already lost.
Zac Gray
November 24, 2025 AT 09:22Maybe the real problem isn’t lithium. Maybe it’s that we keep prescribing drugs that require patients to become pharmacologists just to stay alive. Shouldn’t the system protect us? Not the other way around?
Ellen Calnan
November 26, 2025 AT 08:01I keep a little card in my wallet now: ‘LITHIUM PATIENT. DO NOT GIVE NSAIDS OR DIURETICS WITHOUT CHECKING LEVELS.’ I’ve handed it out to EMTs. I’ve given it to pharmacists. I’ve left copies with my family. Because if no one else is going to protect me, I will.
This isn’t just medical advice. It’s survival.
Andrew Montandon
November 27, 2025 AT 16:26Here’s what actually works: if you’re on lithium, become your own pharmacist. Bookmark this post. Print it. Tape it to your fridge. Memorize the names of the dangerous drugs. And if your doctor says ‘it’s fine,’ ask them to show you the data. If they can’t, find a new doctor. Your brain is worth more than their convenience.
Michael Petesch
November 28, 2025 AT 16:58Moreover, the cultural invisibility of OTC drug risks speaks to a broader societal failure: we treat pharmaceuticals as binary-prescription = dangerous, OTC = harmless. This is dangerously simplistic.
seamus moginie
November 30, 2025 AT 11:02Doctors don’t warn us. They assume we know. We assume they’ve got it covered. Result? Chaos. This needs to be on every pharmacy shelf. In every GP waiting room. On the back of every lithium prescription bottle. Not a blog post. Not a PDF. A sign. A warning. Like cigarette packs. Because people are dying because we’re too polite to say ‘DON’T.’
Richard Risemberg
November 30, 2025 AT 22:34Here’s the truth: lithium toxicity doesn’t care if you’re smart, rich, or educated. It doesn’t care if you ‘feel fine.’ It only cares about sodium balance, kidney function, and whether someone remembered to check your levels after you started that new blood pressure med.
So if you’re on lithium: make a list. Write down every pill, every supplement, every tea you drink. Bring it to every appointment. Don’t say ‘I think I’m fine.’ Say ‘I need a lithium level today.’ And if your provider rolls their eyes? Find someone who doesn’t.
Christopher K
December 2, 2025 AT 06:45I stopped lithium. I started walking. I started eating real food. My moods are better. My kidneys are fine. And I didn’t need a single blood test.
Sam Reicks
December 2, 2025 AT 13:04river weiss
December 3, 2025 AT 17:15