Key Takeaways
- Boosted protease inhibitors pose the greatest interaction risk, especially with statins, inhaled steroids and certain erectile‑dysfunction drugs.
- Integrase strand transfer inhibitors (INSTIs) have the lowest overall burden but still need attention with rifampin, metformin and some herbal supplements.
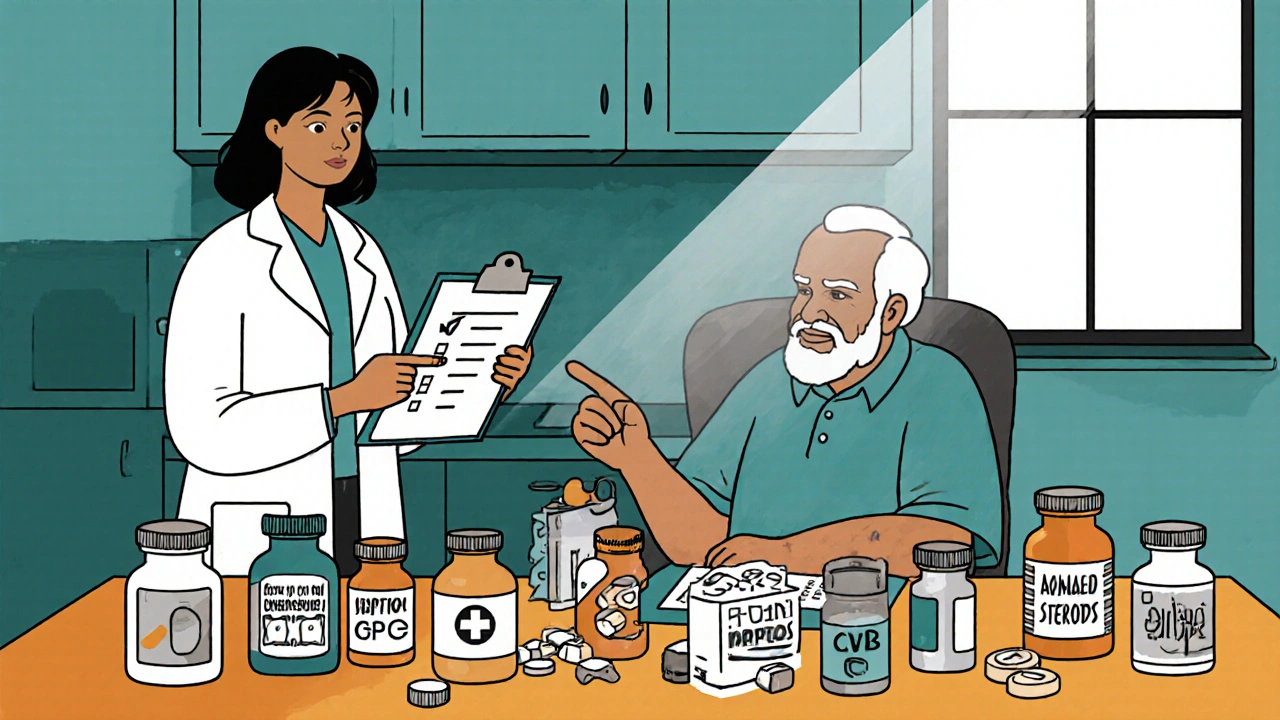
- Older patients on polypharmacy are the most vulnerable; a systematic medication review at each visit cuts adverse events by ~40%.
- The University of Liverpool HIV Drug Interactions Checker remains the gold‑standard tool for clinicians.
- Future regimens aim to be "interaction‑proof," with next‑generation capsid inhibitors leading the way.
When treating HIV, Antiretroviral therapy (ART) is a lifelong regimen of medicines that keeps the virus suppressed and the immune system functional. While ART has turned HIV into a manageable chronic condition, it also brings a hidden threat: drug‑drug interactions that can wreck treatment success or cause serious toxicity. In today’s aging HIV population, where half of patients are over 50 and many take five or more additional drugs, recognizing high‑risk blends is essential.
Why Interactions Matter: The Pharmacokinetic Landscape
Most interactions stem from three mechanisms: enzyme inhibition, enzyme induction, and transporter modulation. Protease inhibitors (PIs) are potent inhibitors of cytochrome P450 3A4 (CYP3A4) and P‑gp transporters. When combined with drugs that rely on these pathways, plasma concentrations can sky‑rocket-sometimes 20‑ to 30‑fold, as seen with simvastatin a CYP3A4‑metabolized statin. Conversely, non‑nucleoside reverse transcriptase inhibitors (NNRTIs) like efavirenz act as CYP3A4 inducers, slashing co‑drug levels by up to 75%. Integrase strand transfer inhibitors (INSTIs) such as dolutegravir and bictegravir have minimal CYP inhibition, making them the safest class for co‑medication-but they’re not completely interaction‑free.
Class‑by‑Class Interaction Profiles
| ART Class | Typical Boosters | Number of Major Interactions* | Representative High‑Risk Co‑meds |
|---|---|---|---|
| Boosted Protease Inhibitors | Ritonavir 100 mg, Cobicistat 150 mg | 217 | Simvastatin, Fluticasone, Avanafil, Tacrolimus |
| NNRTI‑based (efavirenz) | None (inducer) | 68 | St. John’s Wort, Methadone, Oral contraceptives |
| INSTI‑based (dolutegravir, bictegravir) | None | 7-12 | Rifampin, Metformin, Carbamazepine |
*Based on the University of Liverpool HIV Drug Interactions Checker (2023).
High‑Risk Pairings You Must Watch
The following combos have enough evidence to be labeled “contraindicated” or “requires immediate dose adjustment.”
- Statins + boosted PIs: Simvastatin should never be used with ritonavir or cobicistat because concentrations can rise 20‑ to 30‑fold, leading to rhabdomyolysis. Safer options include pitavastatin 4 mg daily or fluvastatin 80 mg daily.
- Inhaled corticosteroids + ritonavir: Fluticasone 250 µg BID or budesonide nasal spray can cause adrenal insufficiency or Cushing‑like features. About 17 % of patients on boosted PIs with these inhalers required hospitalization (University of Washington, 2023).
- SSRIs + ritonavir: Fluoxetine combined with ritonavir can precipitate serotonin syndrome; dose‑reduce fluoxetine by 50 % or discontinue ritonavir.
- Erectile‑dysfunction drugs: Avanafil is absolutely contraindicated; sildenafil must be limited to 25 mg every 48 h when taken with a booster.
- Rifampin + INSTIs: Rifampin cuts dolutegravir levels by ~71 %, requiring a dose increase to 100 mg BID or switching to a PI‑based regimen.
- Metformin + dolutegravir: Dolutegravir lowers metformin exposure by 33 %; monitor glucose and consider a modest dose increase.
- St. John’s Wort + NNRTIs: This herbal inducer drops efavirenz concentrations by 50‑60 %, risking virologic failure.
Practical Workflow for Clinicians
1. Medication reconciliation at every visit. Capture prescriptions, OTCs, supplements, and recreational drugs-38 % of serious interactions involve non‑prescription agents.
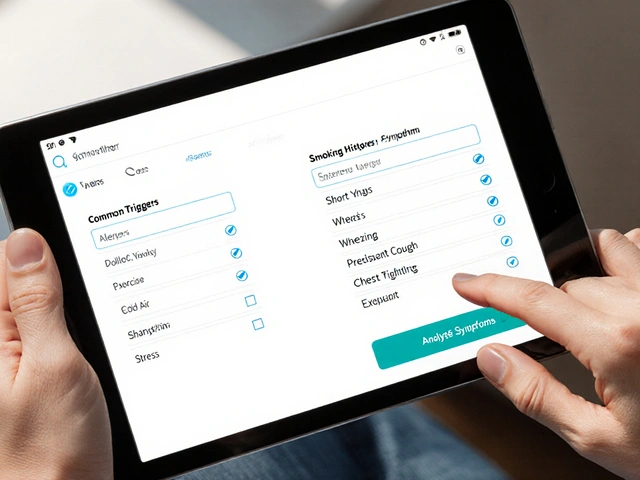
2. Run the regimen through an interaction checker. The Liverpool tool covers >1,200 non‑ART drugs and updates continuously.
3. Apply class‑specific rules:
- For boosted PIs, flag any CYP3A4 substrate with a narrow therapeutic index (statins, calcium‑channel blockers, certain anti‑arrhythmics).
- For NNRTI inducers, check oral contraceptives, anticoagulants, and antidepressants.
- For INSTIs, verify rifampin, carbamazepine, and high‑dose metformin.
4. Adjust doses or switch agents before the patient leaves. Example: when moving from ritonavir‑boosted darunavir to dolutegravir, reduce tacrolimus by 75 % and monitor levels.
5. Document the plan and educate the patient. Explain why a statin was changed and what symptoms to watch for (muscle pain, dark urine).

Special Populations: Older Adults and Polypharmacy
Data from the VA (2023) show veterans with HIV over 65 take an average of 9.2 meds, and 68 % have at least one potential interaction. Each added medication raises interaction odds by 18 %, and each year since diagnosis adds 7 % risk. Strategies:
- Prioritize INSTI‑based first‑line therapy whenever resistance allows.
- Choose statins with minimal CYP3A4 metabolism (pitavastatin, fluvastatin).
- Avoid inhaled steroids; if needed, use budesonide at the lowest dose and monitor cortisol.
- Screen for renal function when prescribing metformin and adjust dolutegravir dose accordingly.
Emerging Solutions and the Future of Interaction Management
Lenacapavir, a subcutaneous capsid inhibitor given every six months, entered the 2023 HHS Guidelines. It inhibits CYP3A, so colchicine and certain anti‑arrhythmics must be avoided, but its long‑acting nature reduces daily pill burden and the chance of missed doses that trigger rescue therapy interactions.
Next‑generation ART aims for “interaction‑proof” profiles. Early trials of a novel protease inhibitor with negligible CYP impact show a 90 % drop in major drug‑drug alerts versus ritonavir. By 2030, the International Antiviral Society‑USA predicts an 80 % reduction in clinically significant interactions as INSTI‑centric regimens dominate.
Meanwhile, digital solutions are rising. AI‑driven EMR plugins now auto‑populate the Liverpool checker in real‑time, flagging high‑priority alerts before the prescription is signed.
Quick Checklist for Busy Clinicians
- Gather a full medication list at each encounter.
- Enter the ART regimen into the Liverpool interaction checker.
- Identify any “contraindicated” or “high‑priority” matches.
- Statins → switch to pitavastatin or fluvastatin.
- Inhaled steroids → consider oral alternatives or taper.
- SSRIs → evaluate serotonin‑syndrome risk.
- Adjust doses or change agents before patient leaves.
- Document changes and provide clear patient counseling.
What makes ritonavir a high‑risk booster?
Ritonavir strongly inhibits CYP3A4, CYP2D6, and P‑gp. This raises levels of any co‑administered drug that depends on those pathways, sometimes by 20‑ to 30‑fold, leading to toxicity.
Are INSTIs completely free of interactions?
No. While they have the fewest interactions, INSTIs still require adjustments with strong CYP inducers like rifampin and with metformin, which has reduced exposure when used with dolutegravir.
How should I manage a patient on a boosted PI who needs a statin?
Avoid simvastatin and lovastatin entirely. Choose pitavastatin 4 mg daily or fluvastatin 80 mg daily, and monitor lipid levels and muscle symptoms.
What is the best tool for checking ART interactions?
The University of Liverpool HIV Drug Interactions Checker is widely endorsed, covering >1,200 non‑ART drugs and providing evidence‑based management advice.
Do herbal supplements matter?
Absolutely. St. John’s Wort can halve efavirenz levels, and even modest supplements like ginseng may affect CYP activity. Always ask patients about herbs.


Cheyanne Moxley
October 25, 2025 AT 20:01Honestly, it's infuriating how some clinicians treat patients like they're just a list of pills. You can't just slap a boosted PI on someone without checking their statin or inhaler first. It's basic duty to run the Liverpool checker every visit, not an optional extra. If we keep ignoring these high‑risk combos, we're basically signing death warrants for our patients. Wake up and own your responsibility!
Kevin Stratton
October 30, 2025 AT 19:01When we think of medication safety, we're really confronting the delicate balance between life‑preserving science and the hubris of shortcuts. The checklist is a mirror reflecting our ethical commitment; ignoring it says we value convenience over human dignity 😊. It's not just about labs; it's about trust.
Manish Verma
November 4, 2025 AT 19:01Mate, I get the moral preaching, but let's be real-our healthcare systems are built on evidence, not on your sanctimonious rant. In Australia we follow the guidelines to the letter, and we still see patients fall through the cracks because of cheap shortcuts. A friendly reminder: the science doesn't care about your feelings.
Lionel du Plessis
November 9, 2025 AT 19:01PK/PD interaction profiling shows Cmax spikes that translate to toxicity risk especially with CYP3A4 substrates like statins and inhaled steroids. Minimalist approach to monitoring often misses these high‑impact events.
Andrae Powel
November 14, 2025 AT 19:01I've seen a lot of patients get flustered when their meds clash, so here’s a quick practical tip: always pull up the Liverpool interaction checker before you sign a prescription. If you see a “contraindicated” flag, either switch the ART backbone or pick an alternative co‑medication-often a different statin works just fine. Also, document the change in the chart and walk the patient through why the switch matters; it reduces confusion and improves adherence.
Leanne Henderson
November 19, 2025 AT 19:01Great point! 😊
Just to add, when you’re counseling someone on a new regimen, it helps to give them a printable list of “do NOT combine” meds-people love a handy cheat sheet!
And always remind them to bring every OTC or herb they’re taking to the next visit; those “natural” supplements can be sneaky culprits.
Megan Dicochea
November 24, 2025 AT 19:01Thanks for the rundown. The key is to keep the medication list up‑to‑date and run the checker regularly. It’s a simple habit that saves a lot of trouble.
Greg Galivan
November 29, 2025 AT 19:01Look, the data is clear-if you ignore the interaction alerts you are just asking for trouble. People keep saying "it's just a small risk" but that little risk becomes a big problem when you have dozens of patients on the same regimens. Stop making excuses.
James Doyle
December 4, 2025 AT 19:01It is beyond alarming that, in this day and age, we continue to witness repeated negligence surrounding antiretroviral drug interactions, especially given the plethora of robust tools at our disposal. The moral imperative for clinicians is unequivocal: they must internalize the principle that every prescription is a covenant with a human life, not a mere transaction.
First, the University of Liverpool HIV Drug Interactions Checker provides a comprehensive, evidence‑based platform that should be integrated into every encounter; neglecting to consult it is tantamount to willful ignorance. Second, the data on boosted protease inhibitors demonstrate a staggering 217 major interactions, with statins and inhaled corticosteroids topping the list. Ignoring these interactions can precipitate rhabdomyolysis, adrenal insufficiency, or even fatal outcomes.
Third, the aging HIV population-now half over the age of 50-exhibits polypharmacy at a rate that rivals any chronic disease cohort. Each additional medication compounds the interaction risk exponentially, a fact underscored by the VA study citing a 68 % prevalence of at least one high‑risk pairing in patients over 65. Consequently, medication reconciliation is not a bureaucratic checkbox; it is a lifesaving ritual that must be performed with meticulous rigor at every visit.
Moreover, the pharmacokinetic mechanisms-enzyme inhibition, induction, and transporter modulation-are not abstract concepts but concrete pathways that dictate plasma concentrations. For instance, ritonavir’s potent inhibition of CYP3A4 can amplify simvastatin levels twenty‑fold, directly leading to catastrophic muscle breakdown. Conversely, efavirenz’s induction of the same enzyme can degrade concomitant drug concentrations, risking therapeutic failure.
In practice, the clinician must adopt a systematic workflow: capture the full medication list (including OTCs and herbal supplements), run the regimen through the interaction checker, apply class‑specific rules, adjust doses proactively, and document every decision with patient education. The cost of omission is far greater than the time invested in this process.
Finally, the future promises interaction‑proof regimens, such as the capsid inhibitor lenacapavir, yet even these novel agents carry their own interaction caveats. Until we reach an era where pharmacokinetic independence is the norm, the onus remains on prescribers to wield the existing tools with diligence and ethical responsibility. The stakes are simply too high to accept anything less.
Edward Brown
December 9, 2025 AT 19:01Sure, the big pharma labs say the new capsid inhibitors are safe but have you ever wondered why they keep hiding the full interaction data? They want us to trust their "interaction‑proof" hype while quietly monitoring us with hidden pharma back‑doors. The whole system is a staged play and the checker is just a curtain.
ALBERT HENDERSHOT JR.
December 14, 2025 AT 19:01I appreciate all the insights shared here. 🌟 A practical takeaway for anyone prescribing ART: set a reminder to run the Liverpool tool before each new prescription, and keep a simple cheat‑sheet of high‑risk pairings handy for patients. This proactive step not only safeguards health but also builds confidence in our therapeutic decisions.
Suzanne Carawan
December 19, 2025 AT 19:01Oh sure, because ignoring drug interactions has never caused any harm before.