Antihistamine Effectiveness Tracker
Daily Symptom Log
Allergen Exposure Log
Check all that applied today:
What Your Log Shows
Track your symptoms for 2 weeks to identify patterns. If your symptoms worsen despite consistent medication, it may indicate increasing allergy burden rather than tolerance.
Based on your entries, consider:
- Reduce exposure - Wash bedding weekly, use HEPA filters, reduce clutter
- Nasal steroids - Intranasal corticosteroids (like Flonase) work better for nasal symptoms
- Professional help - Allergy testing can identify new sensitivities
Ever taken your daily Zyrtec or Claritin for months, then noticed your sneezing and itchy eyes are back worse than ever? You’re not imagining it. But here’s the twist: it might not be your medicine losing power-it might be your allergies getting stronger.
Does Your Antihistamine Really Stop Working?
Millions of people rely on antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) to manage seasonal allergies, hives, or chronic itching. These drugs are safe, non-sedating, and available over the counter. But when you’ve been taking them for over a year, it’s common to hear someone say, “It just doesn’t work like it used to.”
So what’s really going on? Is your body building up a tolerance? Or is something else happening?
The medical world is split. Some doctors say true tolerance-where your H1 receptors stop responding to the drug-is extremely rare. Others say patients clearly report reduced effects after months of daily use. And patient surveys back this up: nearly 30% of long-term Zyrtec users on Drugs.com say it stopped working after 8 months on average. On Reddit, 78% of users reported the same.
Here’s the key: antihistamine tolerance isn’t like opioid tolerance. You don’t need higher doses just to feel normal. There’s no physical withdrawal. But that doesn’t mean the drug stops helping.
What’s Actually Changing?
Most of the time, the problem isn’t the drug. It’s your environment-or your body’s reaction to it.
Think about it: if you moved from a dry city to a humid coastal area, your pollen exposure could double. If you got a new pet, started gardening, or your home got moldy, your allergy triggers just changed. Your body’s immune system ramps up its response. Suddenly, the same dose that used to keep you calm is now fighting a bigger battle.
Dr. David Stukus from Nationwide Children’s Hospital says this is the #1 reason antihistamines seem to fail: “The allergy burden increased-not the drug lost potency.”
Another factor? You might be developing new allergies. Studies show that adults can develop new sensitivities to dust mites, mold, or even foods they never reacted to before. What worked last spring might not cut it this year because your body now has more things to react to.
What About Dose Escalation?
Some patients try taking more. Two pills instead of one. Or switching to a higher-dose version. Is that safe?
Yes-up to a point. The European Academy of Allergy and Clinical Immunology (EAACI) says it’s fine to increase second-generation antihistamines like Zyrtec or Allegra up to four times the standard dose for chronic hives. In one study, 49% of patients who didn’t respond to normal doses got relief at higher doses.
But here’s the catch: you’re not building tolerance. You’re just giving your body more of the drug to fight a stronger reaction. Think of it like using more sunscreen when you’re at the beach longer-not because your sunscreen is broken, but because the sun is stronger.
Still, don’t go beyond four times the recommended dose without seeing a doctor. While modern antihistamines like cetirizine and fexofenadine are very safe, there’s still a small risk of heart rhythm issues at very high doses-especially if you’re on other medications or have liver problems.

Why Do Some People Rotate Antihistamines?
Ever heard of “antihistamine rotation”? It’s when people switch between Zyrtec, Claritin, and Allegra every few months to “reset” their system.
It’s popular. About 35% of long-term users do it, according to market data. But here’s the truth: there’s no solid science proving it works better than sticking with one.
Why do people swear by it? Because when you switch, you get a placebo effect-you notice improvement because you expect it. Or maybe your allergies naturally dipped that week. Or you coincidentally cleaned your house.
Also, all second-generation antihistamines work the same way: they block H1 receptors. They’re chemically different, but they do the same job. Switching between them won’t “refresh” your receptors. If one stopped working, the others likely will too-unless your triggers changed.
First-Gen vs. Second-Gen: The Sleep Aid Trap
Don’t confuse the two types. First-generation antihistamines like diphenhydramine (Benadryl) were originally designed to make you sleepy. That’s why people use them for insomnia.
And yes-people do build tolerance to the sleep effect. After a few weeks, you need more to feel drowsy. That’s not true antihistamine tolerance. That’s your brain adapting to sedation, like with alcohol or sleeping pills.
But if you’re taking Benadryl for allergies, you’re using the wrong tool. It’s short-acting, causes brain fog, and isn’t meant for daily use. Stick with second-gen meds for allergies. Save Benadryl for emergencies.
When It’s Time to Try Something New
If your antihistamine isn’t cutting it anymore, don’t just up the dose or switch brands. Ask yourself: are you treating the right problem?
For nasal symptoms-congestion, runny nose, sneezing-antihistamines are only part of the solution. Intranasal corticosteroids (like Flonase or Nasacort) are far more effective. A meta-analysis of 28 studies found 73% of patients had better control with nasal sprays than antihistamines alone.
And if you’ve got chronic hives or severe allergies that don’t respond to anything? Immunotherapy might be the answer. Allergy shots (subcutaneous) work for 60-80% of people over time. Sublingual tablets (under-the-tongue) help 40-60%.
For the toughest cases-like chronic hives that don’t respond to high-dose antihistamines-Xolair (omalizumab) is a biologic injection that shuts down the allergic response at the source. In trials, 50-60% of patients became completely symptom-free.
What Should You Do?
If your antihistamine feels less effective:
- Track your symptoms for 2 weeks. Use a simple journal: note sneezing, itching, congestion, and what you were exposed to (pets, pollen, cleaning products).
- Check your environment. Wash bedding weekly in hot water. Use HEPA filters. Reduce clutter where dust collects.
- Try a nasal corticosteroid spray. Use it daily for 2-4 weeks. It takes time to work, but it’s the most effective treatment for nasal allergies.
- If you’re still struggling, talk to an allergist. Get tested for new sensitivities. Ask about immunotherapy.
- Don’t self-escalate doses beyond 4x without medical advice.
The bottom line: your antihistamine isn’t broken. Your allergies might be. And that’s fixable-with the right tools.
What’s Next for Research?
Scientists are now trying to find biomarkers-measurable signs in the blood-that can tell the difference between true drug tolerance and worsening allergy disease. A 2023 clinical trial is tracking 450 patients to see if they can predict who’s developing real tolerance versus who’s just facing new triggers.
For now, the best advice comes from real-world experience: if your meds feel weaker, look at your life, not your medicine bottle.
Can you really build up a tolerance to Zyrtec or Claritin?
True pharmacological tolerance-where your body’s receptors stop responding-is considered very rare by most allergists. What people experience is usually an increase in allergy triggers, new sensitivities, or worsening disease-not the drug losing power. Studies show most patients respond better to higher doses or switching to nasal sprays, not because of tolerance, but because their allergy burden increased.
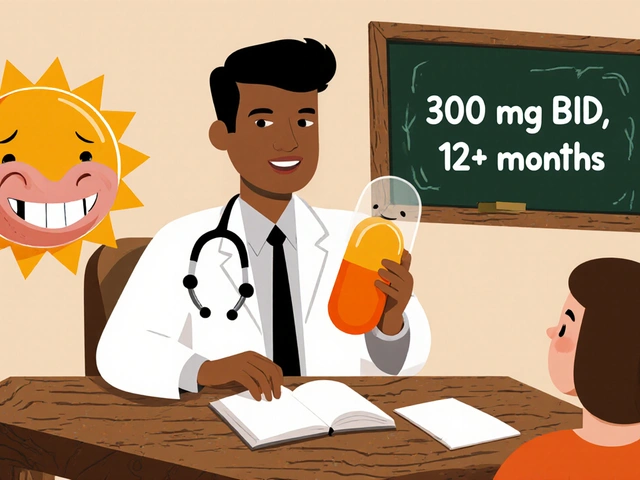
Is it safe to take two Zyrtec pills a day?
The standard dose is 10 mg once daily. Taking 20 mg (two pills) is within the recommended range for chronic hives under medical supervision. The European guidelines allow up to four times the standard dose (40 mg) for resistant cases. But don’t do this long-term without consulting a doctor. Higher doses may cause mild side effects like drowsiness or dry mouth, and there’s a small risk of heart rhythm changes in vulnerable people.
Why does my Claritin work in winter but not in spring?
Because your exposure to allergens changes. In winter, indoor allergens like dust mites are stable. In spring, pollen counts spike-sometimes tenfold. Your body reacts more intensely, so the same dose of Claritin isn’t enough. This isn’t tolerance. It’s seasonal allergy overload. A nasal spray or allergy testing can help you adjust your treatment.
Should I switch antihistamines every few months?
There’s no scientific evidence that rotating between Zyrtec, Claritin, and Allegra improves long-term results. All three work the same way-blocking H1 receptors. If one stops working, the others likely will too. Rotating may give you a placebo effect, but it won’t reset your body’s response. Focus instead on reducing triggers or adding nasal steroids.
What’s the best alternative if antihistamines don’t work?
For nasal symptoms, intranasal corticosteroids (like Flonase) are the most effective next step-better than antihistamines alone. For chronic hives, high-dose antihistamines or Xolair (omalizumab) are options. For long-term relief, allergy immunotherapy (shots or tablets) can retrain your immune system and reduce or eliminate symptoms over time. Talk to an allergist to find the right fit.

Bob Martin
October 29, 2025 AT 20:53Antihistamines don't stop working your allergies just get louder
Linda Patterson
October 31, 2025 AT 06:34Let me break this down for you people who think it's tolerance. The FDA doesn't recognize true H1 receptor tolerance because it's biologically implausible at these doses. What you're seeing is environmental escalation. Pollen counts have risen 20% in the last decade due to CO2 fertilization. Your body isn't desensitized-it's overwhelmed. And if you're still on Zyrtec alone for nasal symptoms you're basically using a Band-Aid on a hemorrhage. Intranasal corticosteroids are first-line for a reason. The data is overwhelming. Stop chasing pills and start treating the disease.
Christy Tomerlin
October 31, 2025 AT 19:42Oh please. You're all just brainwashed by Big Pharma. They don't want you to know that antihistamines are just suppressing symptoms like a drug cartel. Real healing comes from fasting, alkaline diets, and ditching all processed food. I cured my allergies in 3 weeks by eating only raw kale and chanting mantras. Your doctors are lying to you. The truth is out there.
Susan Karabin
November 1, 2025 AT 12:24It's funny how we blame the medicine when the world around us is changing faster than our bodies can adapt. We moved from quiet suburbs to the city, got a dog, started composting, and suddenly Zyrtec doesn't cut it. Not because it's broken. Because life got louder. Maybe the real question isn't what's wrong with the drug-but what's wrong with how we live.
Glenda Walsh
November 3, 2025 AT 00:25Wait wait wait-I just tried doubling my Claritin and now I’m dizzy and my heart is racing. Is this normal? Should I go to the ER? I didn’t know this could happen. I thought it was just a pill. Please someone tell me if I’m going to die. I have three kids. I can’t die. I just want to stop sneezing.
Tanuja Santhanakrishnan
November 4, 2025 AT 09:22As someone from India where seasonal allergies are wild and over-the-counter meds are the only option for most, I’ve seen this play out for years. People rotate antihistamines like they’re swapping spices in a curry-thinking it’ll magically fix things. But the real fix? Cleaning your bedding every week, using a HEPA filter, and avoiding outdoor time at dawn. Simple. Cheap. Effective. No magic pills needed. Your body just needs a quieter environment.
Raj Modi
November 5, 2025 AT 08:13From a clinical perspective, the phenomenon described herein is not indicative of pharmacological tolerance per se, but rather a dynamic upregulation of the allergic cascade secondary to increased antigenic exposure, concomitant immune sensitization, and potential dysbiosis of the mucosal microbiome. The second-generation antihistamines remain efficacious, but their pharmacodynamic ceiling is exceeded when the IgE-mediated mast cell degranulation burden surpasses the receptor blockade capacity. Therefore, augmentation with intranasal corticosteroids is not merely adjunctive-it is pathophysiologically rational and evidence-based. Furthermore, the absence of randomized controlled trials validating antihistamine rotation protocols renders such practice anecdotal at best.
Karen Werling
November 6, 2025 AT 05:24My mom used to take Benadryl every night for allergies… and then she started taking it just to sleep. Now she can’t sleep without it. I told her it’s not the same thing. She said ‘But it’s a pill, right?’ 😅 Please, please, please don’t use Benadryl for sleep. It’s like using a chainsaw to cut your toenails. Use melatonin or just… go to bed earlier. Your brain will thank you. 🌙
STEVEN SHELLEY
November 7, 2025 AT 08:20THIS IS ALL A LIE. THEY WANT YOU TO THINK IT’S YOUR ALLERGIES. IT’S THE CHEMTRAILS. THE FLUORIDE. THE 5G. THEY PUT IT IN THE WATER SO YOU’LL KEEP BUYING ZYRTEC. I’VE BEEN TRACKING THE PILL SALES AND THE PAST 10 YEARS OF POLLEN COUNTS. THEY’RE CORRELATED. BUT THE REAL CORRELATION IS THE PHARMA STOCK PRICES. THEY’RE MAKING BILLIONS. THEY DON’T WANT YOU TO KNOW THE TRUTH. I SAW IT IN A VIDEO ON A SITE NO ONE ELSE KNOWS ABOUT. YOU’RE ALL SHEEP. I’M THE ONLY ONE WHO SEES IT.
Emil Tompkins
November 8, 2025 AT 10:41Okay but what if… the antihistamine is working perfectly… and your body is just screaming at you to change your life? Like maybe you’re living in a toxic box with moldy curtains and a cat that sheds like a demon? Maybe your anxiety is making your histamine levels spike? Maybe you’re not allergic to pollen… you’re allergic to your existence? 🤔
Lorena Cabal Lopez
November 9, 2025 AT 00:59I just stopped taking it. Didn’t need it. My allergies went away. You’re all overcomplicating this. Just quit.
Stuart Palley
November 11, 2025 AT 00:04So let me get this straight. You’re telling me I can take FOUR times the dose of Zyrtec? Four?! That’s like drinking four energy drinks before a marathon. And you’re saying it’s safe? I’m not taking a single extra milligram. I’ve seen what happens to people who think they’re invincible. One day you’re doubling up. Next thing you know you’re in the ER with a heart rate of 140. And then you blame the pill. No. You blame yourself. Don’t be that guy.