
For women with PCOS, excessive facial or body hair isn’t just a cosmetic concern-it’s a daily reminder of a hormonal imbalance that’s hard to control. About 70 to 80% of women with PCOS experience hirsutism, where thick, dark hair grows in places like the chin, upper lip, chest, or back. It’s not just about appearance. It affects confidence, mental health, and quality of life. Many try shaving, waxing, or threading for years before realizing they need something that targets the root cause: high androgens.
Why Antiandrogens Are Used for PCOS Hirsutism
Antiandrogens don’t remove hair. They stop new hair from becoming thick and dark by blocking the effects of male hormones like testosterone and DHT. These hormones trigger hair follicles to grow coarse, pigmented hair in areas where women typically only have fine, light hair. In PCOS, the ovaries and adrenal glands make too much of these hormones, and the body’s tissues respond more strongly to them.
The goal isn’t to eliminate all hair-it’s to reduce the density and coarseness. That means fewer threading sessions, less bleaching, and less shame. Antiandrogens work by either blocking androgen receptors (like spironolactone) or stopping the conversion of testosterone into its stronger form, DHT (like finasteride). They’re not quick fixes. You won’t see results in a few weeks. It takes 6 to 12 months of daily use to notice a difference, and the best results often come after 18 to 24 months.
Which Antiandrogens Are Actually Used Today
Not all antiandrogens are created equal. Some are outdated, dangerous, or no longer recommended. Here’s what’s actually prescribed today:
- Spironolactone (50-200 mg/day): The most common oral antiandrogen for PCOS. It blocks androgen receptors and also reduces DHT production. It’s affordable-generic versions cost around $15-$45 per month in the U.S. But it can cause dizziness, fatigue, and irregular periods. It’s also a diuretic, so you might need to urinate more often.
- Finasteride (2.5-5 mg/day): Blocks the enzyme that turns testosterone into DHT. It’s effective for scalp and facial hair. But it’s expensive-up to $245 a month without insurance. It’s also FDA-approved for men with hair loss, not women, so it’s used off-label. Some women report improved hair texture but also mood changes or libido drops.
- Eflornithine cream (Vaniqa, 13.9%): A topical treatment applied twice daily to the face. It doesn’t kill hair follicles-it slows hair growth by blocking an enzyme called ornithine decarboxylase. It works best when paired with laser or electrolysis. Studies show 60% of users see noticeable improvement after 6 months. It’s not a cure, but it’s safe for women who can’t take oral meds.
- Bicalutamide (25-50 mg/day): Sometimes used in severe cases, but not first-line. It’s stronger and carries higher liver risk.
- Flutamide and cyproterone acetate: No longer recommended. Flutamide can cause liver failure. Cyproterone acetate has been linked to brain tumors (meningiomas) and is banned or restricted in many countries.
Antiandrogens Are Not First-Line Treatment
Despite how often they’re talked about, antiandrogens are not the starting point for PCOS hirsutism. That’s reserved for combined oral contraceptive pills (COCPs). COCPs lower androgen production from the ovaries and increase sex hormone-binding globulin (SHBG), which binds free testosterone. Studies show COCPs reduce hirsutism scores by about 30-40% over 6-12 months.
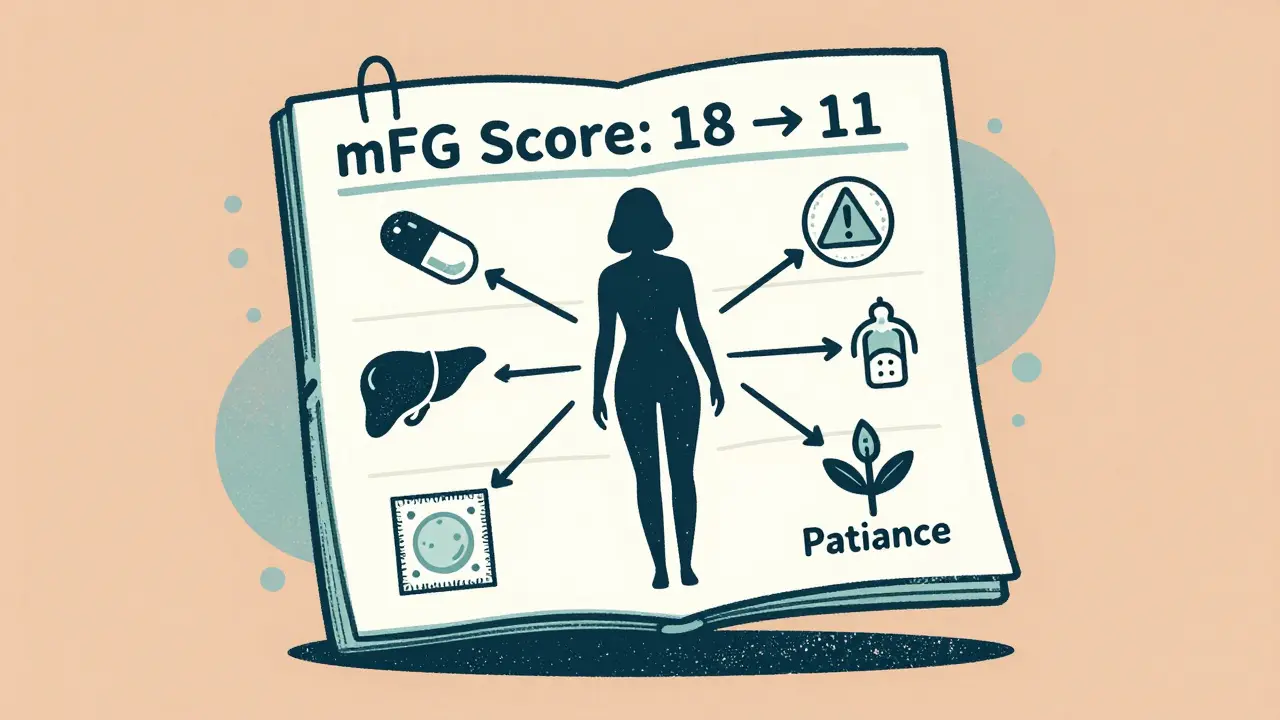
Antiandrogens are reserved for when COCPs don’t work well enough-or can’t be used. Maybe you have migraines with aura, a history of blood clots, high blood pressure, or you’re breastfeeding. Maybe you’ve been on a pill for 6 months and your mFG score (a clinical scale measuring hair growth) hasn’t dropped more than 2 points. That’s when your doctor might add spironolactone or finasteride.
Research from Monash University in 2023 shows that combining antiandrogens with COCPs works better than COCPs alone-but it’s not without risk. Some studies found worse lipid profiles (cholesterol changes) when both are used together. That’s why doctors don’t automatically combine them. They weigh the benefit of faster hair reduction against potential heart health risks.

Topical Options: Eflornithine and Laser
If you’re wary of pills, eflornithine cream is a solid alternative. It’s applied directly to the skin-usually the upper lip and chin-and doesn’t affect your hormones. It won’t make hair disappear, but it slows growth enough that you can go longer between laser sessions or waxing. In clinical trials, adding eflornithine to laser treatment improved hair reduction by 35% compared to laser alone.
Laser hair removal and electrolysis are the only methods that can permanently damage hair follicles. But they’re expensive and require multiple sessions. For PCOS patients, the hair often grows back because the hormonal trigger is still there. That’s why combining laser with antiandrogens or eflornithine is the most effective long-term strategy. One woman on Reddit wrote: “After 4 laser sessions, I still had chin hair. Added Vaniqa. Six months later, I only need one touch-up every 3 months.”
Side Effects and Safety Concerns
Every antiandrogen has risks. Spironolactone can cause low blood pressure, dizziness, and increased potassium levels-especially if you have kidney problems. Finasteride may cause mood changes, depression, or sexual side effects that persist even after stopping the drug. The FDA has issued a black box warning for this.
But the biggest risk? Pregnancy. All oral antiandrogens can cause serious birth defects in male fetuses. That’s why doctors require two forms of contraception if you’re sexually active. One pill isn’t enough. You need a barrier method (condom, diaphragm) plus a hormonal method (pill, IUD, implant). Even if your periods are irregular, you can still ovulate. Many women don’t realize this until it’s too late.
Side effects are why some women quit. On RealSelf, 42% of users said side effects were worse than the hirsutism. One wrote: “Spironolactone made me so tired I couldn’t work. I stopped. The hair came back faster than ever.”
What to Expect: Real Results, Real Time
Patience is non-negotiable. Hair grows slowly. Even after starting treatment, you’ll still see hair. You might even think it’s getting worse at first-this is called shedding, and it’s normal. The follicles are being reset.
Here’s what real patients report:
- At 3 months: Little to no change. Some notice finer hair.
- At 6 months: Hair feels softer, less dark. Fewer ingrown hairs. Threading intervals increase from weekly to biweekly.
- At 12 months: Noticeable reduction in density. Some areas (like upper lip) look almost normal.
- At 18-24 months: Maximum benefit. Most women report feeling more confident, fewer self-conscious moments.
One patient tracked her mFG score: started at 18 (severe), dropped to 11 after 8 months on spironolactone + Yaz. That’s a 39% improvement. Not perfect. But life-changing.
Cost, Access, and Insurance
Spironolactone is cheap-$15-$45/month with insurance. Finasteride? $85-$245/month without coverage. Eflornithine cream (Vaniqa) costs about $245 for one tube, which lasts 1-2 months. Most insurance plans cover spironolactone but not Vaniqa or finasteride for hirsutism because they’re used off-label.
Some pharmacies offer discount cards. GoodRx can cut finasteride costs by 70%. Generic eflornithine isn’t available in the U.S. yet. In Australia, where spironolactone is subsidized under the PBS, it’s under $10 per script. Access varies wildly by country and income.
When to Consider Alternatives
If you’ve tried COCPs and an antiandrogen for 12-18 months with little progress, it’s time to reassess. Maybe your PCOS is more complex. Maybe insulin resistance is driving your androgen levels. In that case, metformin might help-but studies show it’s less effective for hair than antiandrogens.
Other options:
- Weight loss: Even 5-10% body weight reduction can lower androgens and improve hirsutism.
- Insulin-sensitizing diets: Low-glycemic, high-protein, low-refined-carb diets show modest benefit in small trials.
- Acupuncture: Some studies suggest it may lower testosterone, but evidence is weak.
- Professional laser or electrolysis: Best for stubborn areas. Requires commitment and cash.
The Future: What’s Coming Next
Researchers are working on safer, more targeted drugs. One promising candidate is enobosarm (GTx-024), a selective androgen receptor modulator (SARM). In early trials, it reduced hirsutism by 28% more than placebo over 24 weeks-with fewer side effects than spironolactone. It’s not approved yet, but Phase III trials are underway.
Future treatment may be personalized. Genetic tests could identify who’s most sensitive to androgens, helping doctors pick the right drug faster. Combination therapy-COCP + antiandrogen + eflornithine + laser-is becoming the gold standard for moderate to severe cases.
But for now, the most effective approach remains simple: start with COCPs. Wait 6 months. If it’s not enough, add spironolactone or finasteride. Use eflornithine on the face. Pair it with laser. Be patient. And don’t give up.
Can antiandrogens cure hirsutism in PCOS?
No, antiandrogens don’t cure hirsutism. They manage it by reducing the effects of high androgens. Hair growth may slow significantly, but it won’t disappear completely. Stopping the medication usually leads to regrowth. Long-term management is needed, often combining medication with hair removal methods like laser or electrolysis.
How long does it take for spironolactone to work for hirsutism?
Most women start noticing softer, finer hair after 3-6 months. Visible reduction in density usually takes 6-12 months. Maximum improvement often occurs between 18 and 24 months. Consistency is key-missing doses slows results.
Is finasteride safe for women with PCOS?
Finasteride is used off-label for PCOS hirsutism and is generally safe when taken under medical supervision. However, it carries a black box warning from the FDA for potential persistent sexual side effects, including low libido and erectile dysfunction in men-though data in women is limited. It’s not recommended for women who are pregnant or planning pregnancy due to fetal risks.
Can I use eflornithine cream without taking oral medication?
Yes. Eflornithine cream works independently of hormones. It slows hair growth by targeting an enzyme in the follicle. It’s ideal for women who can’t take oral antiandrogens due to side effects, contraindications, or pregnancy plans. Results are slower than with oral meds, but it’s a safe, non-systemic option.
Do I need two forms of birth control if I’m on spironolactone?
Yes. Spironolactone is classified as FDA Pregnancy Category B, meaning it can harm a developing male fetus. Even if your periods are irregular, you can still ovulate. The 2023 International PCOS Guideline requires two forms of contraception-such as a hormonal method (pill, IUD) plus a barrier method (condom)-to prevent pregnancy while taking antiandrogens.
Why do some doctors avoid prescribing antiandrogens for PCOS?
Many doctors avoid them because the strongest evidence supports COCPs as first-line treatment. Antiandrogens have side effects, require long-term use, and carry pregnancy risks. Until 2023, major guidelines said evidence was lacking for their use in PCOS specifically. Even now, they’re considered second-line. Some providers prefer to exhaust lifestyle changes and COCPs first.




Benjamin Glover
December 15, 2025 AT 13:33Spironolactone? Please. If you’re not on the pill first, you’re doing it wrong. This isn’t a beauty pageant-it’s endocrinology. Stop chasing quick fixes and start treating the root. Also, why are we still talking about finasteride for women? It’s not even approved for this. Amateur hour.
Raj Kumar
December 17, 2025 AT 07:07bro i was on spiro for 14 months and it was life changing but my doc said i need to use condom + pill even if my periods are irregular 😅 i thought i was safe bc i skip periods sometimes but nope. also vaniqa + laser = best combo. i go every 3 months now instead of weekly threading. worth every penny.
Melissa Taylor
December 17, 2025 AT 16:33Thank you for writing this with such clarity. So many women feel alone in this, like it’s just their problem. The timeline you laid out-3 months, 6 months, 18 months-is exactly what I needed to hear. It’s not about perfection. It’s about progress. You’re not failing if it takes time. You’re healing.
Jake Sinatra
December 18, 2025 AT 02:49The data on combined therapy is compelling, yet the risk-benefit analysis remains underemphasized in clinical practice. The 2023 Monash study demonstrated a statistically significant reduction in mFG scores with dual pharmacotherapy, yet lipid profile alterations warrant caution, particularly in patients with preexisting metabolic syndrome. Further longitudinal studies are required to assess cardiovascular endpoints.
Lisa Davies
December 18, 2025 AT 09:07Just wanted to say you’re not alone 💪 I was at my worst at 22-chin hair, no confidence, cried in the bathroom before work. Started COCPs, added spiro after 8 months, used Vaniqa on my lip. Now? I wear tank tops. I smile in photos. It took 2 years. But it was worth it. You got this. 🌱
Nupur Vimal
December 18, 2025 AT 14:31Cassie Henriques
December 19, 2025 AT 01:02Actually, the 2023 PCOS guideline update clarified that antiandrogens are now considered second-line *only* if COCPs are contraindicated OR fail to reduce mFG by ≥2 points after 6 months. Also, the term "off-label" is misleading-finasteride’s use in PCOS hirsutism is well-documented in endo journals since 2018. The real barrier is insurance, not evidence. And yes, the black box warning is real-but so is the data showing libido drops are rare (<5%) and reversible. Context matters.
John Samuel
December 21, 2025 AT 00:26As a physician who has managed over 200 PCOS patients with hirsutism, I can confirm: the gold standard remains sequential, multimodal therapy. First, optimize insulin sensitivity through diet and metformin if indicated. Second, initiate combined oral contraceptives for 6–12 months. Third, if mFG score remains ≥12, introduce spironolactone at 50–100 mg/day-never above 200 mg without renal monitoring. Fourth, layer topical eflornithine for facial hair. Fifth, initiate laser after 6 months of medical therapy to maximize follicular damage. Sixth, maintain contraception with dual methods-always. Seventh, monitor liver enzymes and potassium monthly for the first 3 months. Eighth, document progress with serial photographs and mFG scoring. This is not cosmetic. This is endocrine medicine. And it works-if you have the patience, the resources, and the provider who knows how to navigate the system.