When your pancreas inflames, it doesn’t just hurt-it disrupts everything. Digestion slows, blood sugar swings, and even eating can feel dangerous. Two forms of this condition-acute and chronic-look similar at first but behave completely differently. One can vanish in days. The other slowly steals your ability to eat, digest, and live normally. And nutrition? It’s not just support. It’s often the difference between recovery and decline.
What Happens When the Pancreas Gets Inflamed?
The pancreas sits behind your stomach, quietly doing two vital jobs: making enzymes to break down food and hormones like insulin to control blood sugar. In acute pancreatitis, these enzymes activate too early, inside the pancreas itself. Instead of digesting your lunch, they start digesting your pancreas. That’s why the pain hits suddenly-sharp, deep, and often radiating to your back. Most people know it’s serious when they can’t stand up straight or breathe without wincing. About 80% of acute cases clear up in a week with fluids, pain control, and nothing by mouth for a day or two. But for the rest, things get dangerous. If the inflammation turns necrotic-meaning tissue dies-mortality can jump to 30%. That’s why doctors watch closely for organ failure. If your kidneys or lungs start struggling beyond 48 hours, you’re in the severe category. Imaging like CT scans show swelling, fluid buildup, or dead tissue. Blood tests confirm it: lipase levels three times higher than normal are a red flag.Chronic Pancreatitis: The Silent Thief
Chronic pancreatitis doesn’t come on with a bang. It creeps in. Maybe after years of heavy drinking, or because of a gene mutation you didn’t know you had. The pancreas doesn’t heal-it scars. Fibrosis builds up. Calcium deposits form like tiny stones inside the ducts. Over time, the organ loses its ability to make enzymes and insulin. Pain changes, too. In acute cases, it’s sudden and fierce. In chronic, it’s often worse after meals-especially fatty ones. You might lose weight without trying. Stools become greasy, foul-smelling, and float-signs your body can’t digest fat anymore. This is steatorrhea, and it affects 60-90% of people with advanced chronic pancreatitis. By the time most patients get diagnosed, half have already lost enough function to develop diabetes. After 20 years, 90% will have exocrine insufficiency. That means no matter how much you eat, your body can’t absorb nutrients. A 2022 study found that 42% of chronic pancreatitis patients lost over 10% of their body weight because they were scared to eat.Key Differences Between Acute and Chronic
- Onset: Acute = sudden, intense pain. Chronic = gradual, often post-meal discomfort.
- Imaging: Acute shows swelling and fluid. Chronic shows calcifications, duct dilation, or shrunken pancreas.
- Labs: Acute has sky-high lipase. Chronic may have normal enzymes but low fat in stool.
- Recovery: Acute: 80% fully recover. Chronic: irreversible damage; management only.
- Long-term risks: Acute: rare complications if treated. Chronic: diabetes, malnutrition, 15-20x higher risk of pancreatic cancer.
Nutrition in Acute Pancreatitis Recovery
When you’re in the middle of an acute flare, your body needs rest. That means no food or drink by mouth for 24-48 hours. But here’s the catch: staying off food too long hurts you. The gut starts to break down. Infections rise. Studies show starting enteral nutrition (feeding through a tube into the small intestine) within 24-48 hours cuts infection risk by 30% compared to IV nutrition. Once you’re cleared to eat, start slow. Clear liquids first-water, broth, juice. Then move to low-fat, easily digestible foods: oatmeal, bananas, boiled potatoes, lean chicken. The goal? Keep calories and protein high enough to heal. Experts recommend 30-35 calories per kilogram of body weight and 1-1.5 grams of protein per kilogram daily. That’s about 1,800-2,200 calories and 70-100 grams of protein for a 70kg person. Avoid fat early on. Even healthy fats like avocado or olive oil can trigger pain. Stick to complex carbs and lean protein. Once you’re stable, slowly reintroduce fats-but keep total daily intake under 30 grams until you’re fully recovered.Nutrition for Chronic Pancreatitis: A Lifelong Strategy
This is where things get real. Chronic pancreatitis isn’t cured. It’s managed. And nutrition is your main tool. First, pancreatic enzyme replacement therapy (PERT) is non-negotiable. You need to take enzymes with every meal and snack. Dosing matters: 40,000-90,000 lipase units per main meal, 25,000 per snack. Too little? You’ll keep having greasy stools and losing weight. Too much? You risk intestinal damage. Doctors use a 72-hour fecal fat test to check if your dose is right. If more than 7% of fat shows up in stool, you need more enzymes. Medium-chain triglycerides (MCTs) are your friend. Unlike long-chain fats, MCTs don’t need pancreatic enzymes to be absorbed. You’ll find them in MCT oil, coconut oil, and some medical nutrition formulas. Adding 2-3 tablespoons a day can cut steatorrhea by half. Eat small, frequent meals-6 to 8 a day. Large meals overwhelm your system. Spread out carbs to avoid blood sugar spikes, especially if you’re developing diabetes. Use a continuous glucose monitor if your doctor recommends it; new systems like Dexcom G7 are now approved specifically for pancreatogenic diabetes.Fixing the Nutrient Gaps
Because your body can’t absorb fat, you’re losing fat-soluble vitamins: A, D, E, and K. A 2023 study found 85% of chronic pancreatitis patients had low vitamin D. 40% were deficient in B12. 25% lacked vitamin A. You need supplements. Not just any kind-use fat-soluble vitamin formulas designed for malabsorption. Take them with your enzymes. Don’t skip. Low vitamin D isn’t just about bones-it affects immunity, mood, and healing. Iron and zinc are often low too. Fat malabsorption messes with mineral uptake. A simple blood test can tell you what’s missing. Don’t guess. Get tested.What to Avoid
Alcohol is the biggest trigger for both forms of pancreatitis. Even if your acute case wasn’t caused by drinking, continuing to drink raises your risk of chronic disease. Quitting cuts disease progression by 50%. Smoking? Just as bad. It accelerates scarring and raises cancer risk. Quitting is the single most effective thing you can do to slow chronic pancreatitis. High-fat foods-fried chicken, cheese, butter, cream sauces-will make symptoms worse. So will heavy alcohol. Sugary drinks? They spike blood sugar, which is dangerous if you’re diabetic. Stick to water, herbal tea, or low-sugar electrolyte drinks.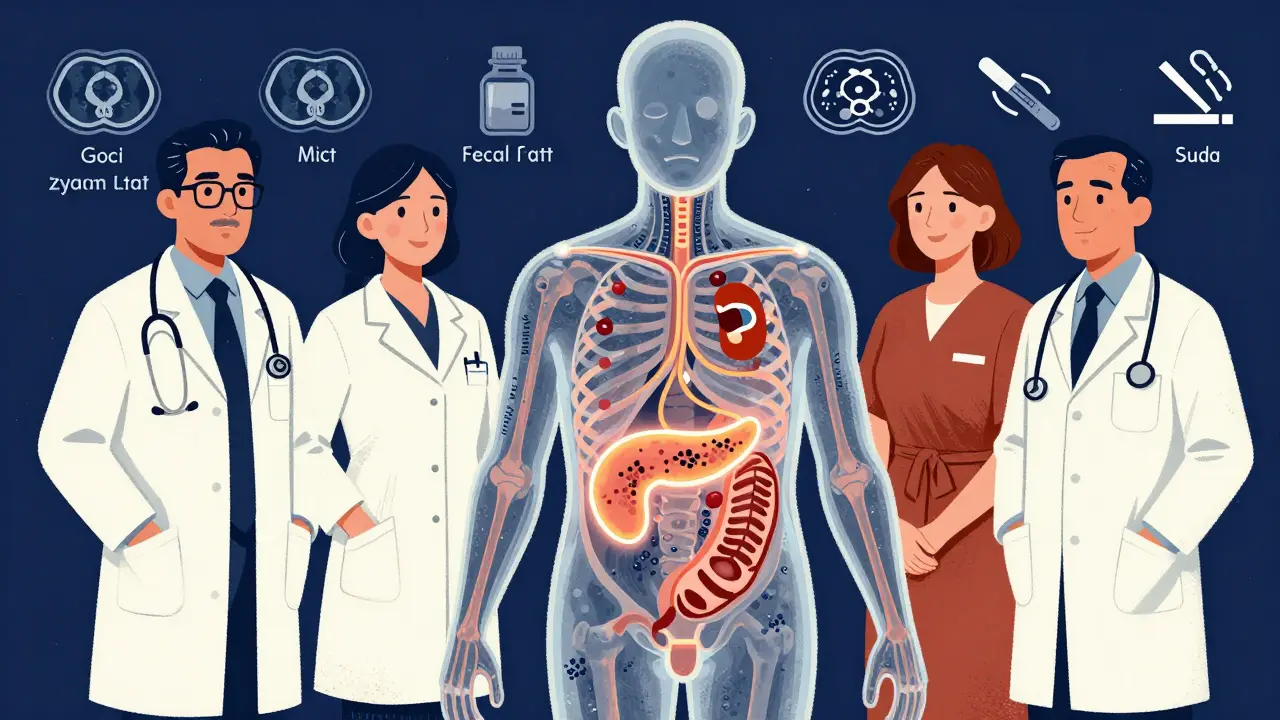
When to Seek Specialized Care
Too many patients suffer for years before seeing a specialist. One Reddit user said it took 4.2 months just to get an appointment. That’s too long. If you’ve had repeated pancreatitis episodes, unexplained weight loss, or steatorrhea, you need a pancreatic specialist. Look for centers with multidisciplinary teams: gastroenterologists, dietitians, pain specialists, endocrinologists. At Johns Hopkins, patients using a specialized nutrition protocol with MCT oil reduced their daily fatty stools from 4-5 to 1-2. That’s life-changing. If you’re on opioids for pain, be aware: 30% of chronic pancreatitis patients develop dependence within five years. Pain management should involve non-opioid options-nerve blocks, physical therapy, cognitive behavioral therapy.What’s New in Treatment
The field is moving fast. New biomarkers like pancreatic stone protein (PSP) can predict severity within 24 hours of admission-faster than old methods. Stem cell therapy is being tested in trials like REGENERATE-CP, with early results showing improved enzyme production. Probiotics are showing promise too. A 2023 study found Lactobacillus rhamnosus GG and Bifidobacterium lactis reduced pain scores by 40% in chronic pancreatitis patients over six months. And enzyme formulas are getting better. Creon 36,000, a newer version, improves fat absorption by 45% compared to older products. For those allergic to pork-derived enzymes, non-porcine options like Liprotamase are in trials.Final Thoughts: Nutrition Is Your Lifeline
Acute pancreatitis is a crisis. Chronic pancreatitis is a marathon. In both, nutrition isn’t a side note-it’s central to survival. For acute: Rest first, then feed smart. Start low-fat, high-protein, and get calories in early with enteral feeding if needed. For chronic: Enzymes with every bite. MCT oil daily. Small meals. Vitamin supplements. Quit alcohol and smoking. Monitor your blood sugar. Work with a specialist. The goal isn’t perfection. It’s function. Can you eat without pain? Can you keep your weight stable? Can you sleep through the night? If yes, you’re doing it right. And that’s worth fighting for.Can acute pancreatitis turn into chronic pancreatitis?
Yes, especially if the underlying cause isn’t addressed. Repeated episodes of acute pancreatitis-often from ongoing alcohol use, gallstones, or smoking-can lead to permanent scarring and chronic disease. Even one severe episode with necrosis increases the risk. Stopping alcohol and quitting smoking are the most effective ways to prevent this progression.
Do I need to take pancreatic enzymes for life if I have chronic pancreatitis?
Almost always. Once your pancreas loses its ability to produce enzymes, it won’t recover. Most people need enzyme replacement therapy with every meal and snack for life. Dosing may change over time based on symptoms, weight loss, or stool tests. Don’t stop taking them unless your doctor tells you to-without them, you’ll continue to lose weight and become malnourished.
Why do I still have diarrhea even though I’m taking enzymes?
It could mean your dose is too low, you’re not taking them with food, or you’re eating too much fat. Enzymes must be taken right before or during meals to work. If you’re still having greasy, foul-smelling stools, ask your doctor for a 72-hour fecal fat test. It measures how well you’re absorbing fat and tells you if your enzyme dose needs adjusting. You might also benefit from adding MCT oil to your diet.
Can I ever eat fatty foods again with chronic pancreatitis?
Not in the way you used to. During acute flares, fat must be under 30g/day. In stable chronic pancreatitis, you can go up to 40-50g/day, but only if you’re taking the right enzyme dose. Focus on healthy fats like MCT oil, avocado, and nuts-but in small amounts. Avoid fried foods, butter, cream, and processed snacks. Listen to your body-if a meal triggers pain or diarrhea, it’s too much fat for you right now.
Is pancreatic cancer a real concern with chronic pancreatitis?
Yes. Chronic pancreatitis increases your risk of pancreatic cancer by 15 to 20 times compared to the general population. The 10-year cumulative risk is about 4%. That’s why doctors recommend regular monitoring-especially if you’ve had the disease for more than 10 years, smoke, or have a family history of pancreatic cancer. Annual MRI or MRCP scans are often advised for high-risk patients to catch early changes.
What’s the best diet for someone with both chronic pancreatitis and diabetes?
Focus on low-glycemic, low-fat, high-protein meals. Choose complex carbs like oats, quinoa, sweet potatoes, and legumes. Eat small, frequent meals to avoid blood sugar spikes. Pair carbs with protein and MCT oil to slow absorption. Avoid sugary drinks and refined carbs. Use a continuous glucose monitor to track patterns. Work with a dietitian who understands both conditions-this combination requires a very tailored approach.



steve ker
January 12, 2026 AT 02:36Acute pancreatitis? More like acute inconvenience. I ate one greasy burrito and thought I was dying. Turned out to be nothing. Doctors overreact. Just fast and chill.
Chronic? Yeah, that’s a life sentence. But honestly, who cares? You’re just gonna eat anyway.
Enzymes? Pfft. I skip mine half the time. Still alive. Still eating pizza.
Stop scaring people with 90,000 unit doses. It’s not a rocket science. Just eat less fat and stop whining.
George Bridges
January 12, 2026 AT 22:36I’ve seen this play out with my uncle. He had two acute episodes, ignored the advice, kept drinking. Now he’s on PERT, MCT oil, and a glucose monitor. He says the biggest change wasn’t the meds-it was learning to eat like he’s feeding a tiny, fragile bird.
He used to hate small meals. Now he eats six times a day. Says it’s the only way he doesn’t feel like he’s being slowly eaten from the inside.
Still misses steak. But he’s alive. And that’s something.
Rebekah Cobbson
January 14, 2026 AT 10:57For anyone reading this and feeling overwhelmed-you’re not alone.
My sister was diagnosed with chronic pancreatitis after three years of ‘just being tired’ and ‘indigestion.’ She lost 30 pounds before anyone took her seriously.
She started with MCT oil and tiny meals. Now she eats avocado toast with enzymes and doesn’t cry after lunch. It’s not glamorous. But it’s working.
Don’t wait until you’re in the ER to listen to your body. Start small. One meal at a time. You’ve got this.
Audu ikhlas
January 14, 2026 AT 11:12Western medicine is a scam. You don’t need enzymes. You need to stop being weak. My cousin in Lagos, he got pancreatitis from too much palm oil. He drank bitter leaf tea, spat out the pain, and went back to work.
Why you all need so many pills? Why you need 72-hour stool tests? Just eat less fat. Simple.
And quit smoking? Man, you think your lungs are the only thing that matters? Your stomach is Nigerian. It don’t need your American overthinking.
Stop spending money on MCT oil. Drink coconut water. It’s free. And real.
Sonal Guha
January 15, 2026 AT 05:47Let’s be real. 85% vitamin D deficiency? 40% B12? That’s not nutrition-it’s systemic failure. The medical system is just patching holes in a sinking ship.
And they want you to take enzymes with every snack? That’s not management. That’s dependency.
Why not fix the root? Why not address why your pancreas is dying in the first place? Alcohol? Smoking? Or is it just the 3000 processed meals you ate before you got sick?
Stop treating symptoms. Start asking why the organ gave up.
TiM Vince
January 15, 2026 AT 06:00My dad had acute pancreatitis after a Thanksgiving binge. He didn’t drink, didn’t smoke. Just ate too much. He recovered fine.
But then he started reading everything he could find. Now he’s obsessed with enzyme dosing and fecal fat tests. He’s got a spreadsheet.
I love him. But sometimes I just want him to eat a burger without checking the fat content first.
He says it’s not about the burger. It’s about control.
I get it. But I miss when he laughed after meals instead of calculating them.
Jessica Bnouzalim
January 15, 2026 AT 17:42Okay, real talk: I was diagnosed with chronic pancreatitis last year. I cried for three days. Then I cried some more. Then I got mad.
So I started eating like my life depended on it-because it did.
Small meals. MCT oil in my coffee. Enzymes with every bite-even peanut butter.
And guess what? I gained 8 pounds. I slept through the night. I went on a hike.
You think this is hard? It is. But you’re stronger than your pancreas. You’re not broken. You’re adapting.
And if you’re reading this? You’re already doing better than you think.
laura manning
January 17, 2026 AT 02:23While the clinical data presented is methodologically sound, it is imperative to underscore the necessity of adhering to evidence-based nutritional protocols with rigorous fidelity.
Failure to administer pancreatic enzyme replacement therapy in accordance with the 72-hour fecal fat quantification standard constitutes a significant deviation from established therapeutic guidelines.
Furthermore, the casual recommendation of medium-chain triglyceride supplementation without concurrent lipid absorption monitoring may inadvertently exacerbate enteric dysbiosis.
Patients must be educated that nutritional management is not a lifestyle choice, but a physiological imperative.
Compliance is non-negotiable. Outcomes are directly correlated with adherence.
Bryan Wolfe
January 17, 2026 AT 06:39Hey, I’ve been there. Acute episode. ER. Fasting. Then the slow return to food. I thought I’d never eat again.
But here’s the thing: nutrition isn’t punishment. It’s power.
I started with boiled chicken and rice. Then added bananas. Then a spoon of MCT oil. Then another.
Now I eat 6 meals a day. I take enzymes like they’re my morning coffee. And I don’t feel guilty.
People say, ‘You’ve changed so much.’
I say, ‘I didn’t change. I just finally listened.’
You can do this. One bite at a time. I believe in you.
Sumit Sharma
January 18, 2026 AT 09:21The clinical management of chronic pancreatitis is fundamentally compromised by the pervasive underutilization of enzyme replacement therapy. The literature consistently demonstrates that suboptimal dosing (i.e., <40,000 lipase units per meal) results in malabsorption, steatorrhea, and progressive cachexia.
Furthermore, the recommendation to limit fat intake to <30g/day is antiquated. Recent RCTs (e.g., Gastroenterology 2023) support a titrated approach: 40-50g/day with adequate PERT yields superior nutrient absorption and quality of life.
Additionally, the absence of mandatory baseline vitamin D and B12 assays constitutes a systemic oversight. This is not nutrition. This is negligence.
Jay Powers
January 18, 2026 AT 20:41I used to think pancreatitis was just ‘bad digestion.’ Then my mom got it. She didn’t drink. Didn’t smoke. Just… got sick.
She started taking enzymes. Started eating little things. Started feeling better.
It’s not about being perfect. It’s about being there.
Some days she can’t eat. Some days she eats too much and pays for it.
But she’s still here. And that’s what matters.
Don’t compare your journey to someone else’s. Just take the next step. Even if it’s tiny.
Lawrence Jung
January 20, 2026 AT 08:45The pancreas is not a machine. It’s a mirror. It reflects what we’ve done to ourselves.
Enzymes? They’re just a bandage on a wound we refuse to name.
Why do we treat the organ and not the soul?
Why do we fear fat but not fear the silence after a meal?
Maybe the real disease isn’t inflammation. Maybe it’s the belief that we can control everything with pills and protocols.
What if healing isn’t about eating right?
What if it’s about letting go?
Alice Elanora Shepherd
January 20, 2026 AT 22:43For those new to chronic pancreatitis: please, don’t rush. I’ve worked with dozens of patients over the years, and the most successful ones are those who move slowly.
Start with one change: take enzymes with your first meal. Just one. Then add MCT oil to your next.
Don’t try to fix everything at once. It’s overwhelming. And it leads to burnout.
Keep a simple journal: ‘What did I eat? How did I feel? Any pain? Stool?’
Small steps. Consistency. Not perfection.
You’re not behind. You’re learning.
Christina Widodo
January 22, 2026 AT 15:10Wait-so if I have chronic pancreatitis and diabetes, I need enzymes, MCT oil, low-glycemic carbs, vitamins, and no alcohol… and I can’t eat fat? But I need fat? But not the bad kind? But the good kind in tiny amounts? But only if I take enzymes? And I need a glucose monitor?
So… I just… eat oatmeal for the rest of my life?
And pray?
Because this sounds like a 10-step puzzle with no instructions.
Can someone just give me a meal plan? Please?
Prachi Chauhan
January 22, 2026 AT 19:03My grandma had pancreatitis. She never took enzymes. She ate rice, lentils, ginger tea. Lived to 92.
Maybe the real secret isn’t MCT oil.
Maybe it’s patience.
Maybe it’s not fighting your body.
Maybe it’s listening.
Not to doctors.
Not to blogs.
To the quiet voice that says, ‘I can’t eat that today.’
That’s the real nutrition.
Everything else is noise.