When someone survives a car crash, combat, assault, or any deeply frightening event, their brain doesn’t always reset. For about 1 in 10 people, the fear doesn’t fade. It lingers - in nightmares, in jumpiness, in the way a loud noise can send them back to the moment everything changed. This isn’t weakness. It’s Post-Traumatic Stress Disorder, a real, measurable condition that rewires how the brain responds to danger.
What PTSD Actually Feels Like
PTSD isn’t just being stressed after something bad happens. It’s when your brain gets stuck in survival mode. You might relive the trauma through flashbacks or nightmares. You avoid places, people, or thoughts that remind you of it. You feel numb, detached, or constantly on edge. Simple things - a car backfiring, a smell, a certain time of day - can trigger a panic response that feels like you’re back in the event. The DSM-5-TR, the official diagnostic manual used by clinicians, defines PTSD by four key clusters: intrusion symptoms (like flashbacks), avoidance, negative changes in thinking and mood, and hyperarousal (like being easily startled or having trouble sleeping). These symptoms have to last more than a month and mess up your daily life - work, relationships, even eating or showering.Medication: The Tools We Have Right Now
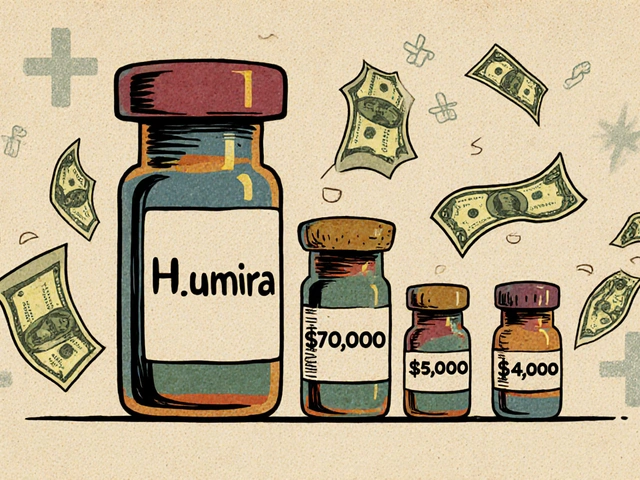
In the U.S., only two medications are FDA-approved specifically for PTSD: sertraline (Zoloft) and paroxetine (Paxil). Both are SSRIs - selective serotonin reuptake inhibitors - originally developed for depression. They work by increasing serotonin, a brain chemical tied to mood and fear regulation. The data shows they help. In large studies, about 53% of people on sertraline saw meaningful symptom reduction. For paroxetine, that number was around 60%. But here’s the catch: only 20-30% of people fully recover on medication alone. Most see improvement, not elimination. Other drugs are used off-label because they work for some people. Venlafaxine (Effexor XR), an SNRI, has similar results to SSRIs. Mirtazapine and amitriptyline show modest benefits, especially for sleep and anxiety. Atypical antipsychotics like risperidone or quetiapine are sometimes added when someone’s stuck with severe nightmares or agitation. But they come with side effects - weight gain, drowsiness, tremors - and aren’t first-line for a reason. Then there’s prazosin. It’s not an antidepressant. It’s a blood pressure drug. But for veterans and others plagued by trauma-related nightmares, it’s a game-changer. Studies show half of users cut their nightmare frequency in half within four weeks. It’s cheap, low-risk, and targeted. If nightmares are your biggest struggle, prazosin might be the most useful tool you’ve been given.Why Medication Alone Isn’t Enough
Medication can quiet the noise. But it doesn’t help you process what happened. That’s where trauma-focused therapy comes in. Cognitive Processing Therapy (CPT) and Prolonged Exposure (PE) are the gold standards. CPT helps you challenge distorted thoughts like “It was my fault” or “The world is completely dangerous.” PE gently guides you to face avoided memories and situations - not to relive the trauma, but to rewire your brain’s fear response. Both have been proven to produce remission rates of 60-70% after 8-12 sessions. Compare that to medication: even the best SSRIs only get you to 50-60% symptom reduction. And if you stop taking them, relapse rates hit 55% within a year. Therapy? The gains stick. Your brain learns new ways to respond. It’s not a crutch - it’s a rebuild. Dr. Matthew Friedman, former head of the VA’s National Center for PTSD, put it bluntly: “Medications treat symptoms but don’t process trauma.” That’s why guidelines from the VA, NICE, and APA all say: start with therapy. Use medication only if therapy isn’t possible, isn’t working, or if symptoms are so severe you can’t even show up for a session.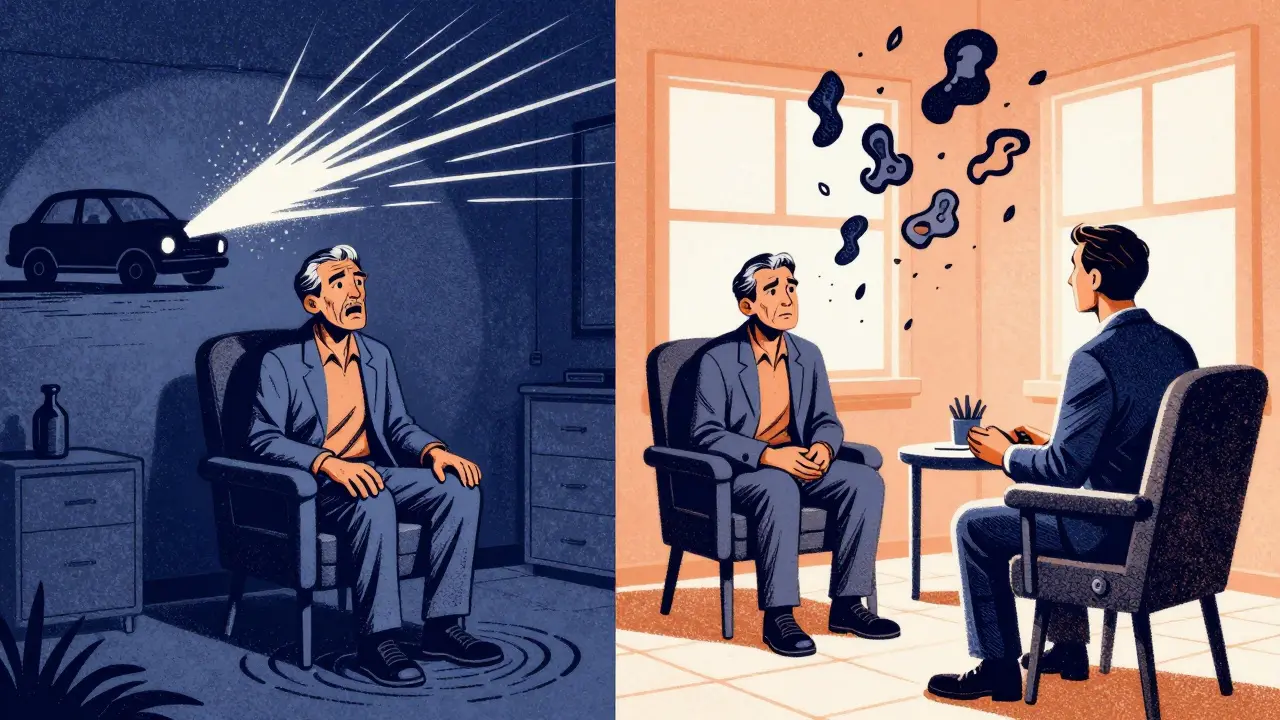
The Real Trade-Offs: Side Effects, Cost, and Time
SSRIs aren’t harmless. About 35% of users report reduced libido. 28% struggle with anorgasmia. Nausea, insomnia, and emotional blunting - feeling flat, disconnected, like you’re watching your life through glass - are common in the first few weeks. One Reddit study of over 1,200 people with PTSD found 42% stopped SSRIs because of side effects. Cost is another factor. A month of generic sertraline costs $4-$10. A single therapy session? $100-$200. But therapy ends. Medication often doesn’t. You might be on it for years. And if you’re not seeing progress after 8-12 weeks at the right dose (sertraline at least 150 mg, paroxetine at least 40 mg), continuing it is unlikely to help. The VA’s own data shows 31% of patients quit SSRIs early because of side effects. That’s not failure. It’s a signal - maybe this isn’t the right path for you. Or maybe you need therapy alongside it.Combining Therapy and Medication: The Best of Both Worlds?
Here’s where things get interesting. A 2021 JAMA Psychiatry study found that combining sertraline with Prolonged Exposure led to a 72% response rate - higher than either alone. Why? Because medication can take the edge off. If you’re too hypervigilant to sit through a therapy session, SSRIs or prazosin might make it possible. Think of it like this: therapy is the construction crew. Medication is the scaffolding. You need the scaffolding to get the crew in, but the house is built by the crew. Some people start with medication to stabilize enough to begin therapy. Others start with therapy and add medication later if symptoms are too overwhelming. There’s no single right order. But the evidence is clear: using both gives you the best shot at real, lasting recovery.
What’s Coming Next?
The field is changing fast. MDMA-assisted psychotherapy - yes, the party drug - is on the verge of FDA approval for PTSD. Phase III trials showed 67% of participants no longer met PTSD criteria 18 weeks after treatment. That’s not a small improvement. That’s remission. Brexpiprazole, an antipsychotic, is being reviewed by the FDA as an add-on to SSRIs. Early results show a 35% symptom reduction when added to existing meds - better than placebo, but not a standalone fix. Researchers are also looking at genetics. The Psychiatric Genomics Consortium has found 95 gene variants linked to how people respond to SSRIs. In the next five years, we may be able to test someone’s DNA and predict if sertraline will work for them - or if they’re better off trying something else.What Should You Do?
If you’re struggling with PTSD, here’s what the evidence says to try:- Start with trauma-focused therapy - CPT or PE. Find a provider trained in it.
- If you can’t access therapy, or symptoms are too severe to begin, consider sertraline or paroxetine. Start low: 25-50 mg. Increase slowly over weeks.
- If nightmares are your main issue, ask about prazosin. It’s simple, cheap, and often life-changing.
- If medication alone isn’t enough after 8-12 weeks, add therapy. Don’t wait.
- If therapy isn’t helping after 12 sessions, talk to your provider about alternatives - including emerging treatments like MDMA-assisted therapy.
Don’t Give Up
PTSD isn’t a life sentence. It’s a wound that needs the right kind of care. Some people heal with therapy alone. Others need medication to get to the point where therapy can work. A few need both - and even then, it takes time. The most important thing? Don’t try to do it alone. Talk to a clinician who understands PTSD isn’t just about taking a pill. It’s about rewiring a brain that learned to fear the world - and helping it learn, again, that it’s safe to feel.Can SSRIs make PTSD worse?
SSRIs don’t make PTSD worse, but they can cause side effects that make people feel worse - like emotional blunting, sexual dysfunction, or nausea. These often fade after a few weeks, but for some, they’re unbearable. If you feel more numb, disconnected, or hopeless after starting an SSRI, talk to your doctor. It might mean the medication isn’t right for you - not that you’re failing. Many people switch to another SSRI, try venlafaxine, or combine it with therapy.
How long does it take for PTSD medication to work?
Most people start to notice small improvements in sleep or anxiety within 2-4 weeks. But full benefit usually takes 8-12 weeks. That’s why doctors don’t switch medications too soon. If you’ve been on sertraline at 150 mg for 10 weeks and still feel overwhelmed, it’s time to talk about other options - not just another pill, but therapy, prazosin, or a different approach.
Is it safe to stop PTSD medication suddenly?
No. Stopping SSRIs or SNRIs abruptly can cause dizziness, nausea, brain zaps, anxiety, or even rebound PTSD symptoms. Always taper off slowly under medical supervision - usually over 2-4 weeks. Even if you feel fine, your brain needs time to readjust. This is especially true if you’ve been on medication for more than 6 months.
Why do some people not respond to any medication?
About 1 in 3 people with PTSD don’t respond to SSRIs, SNRIs, or even antipsychotics. That doesn’t mean they’re broken. It means their brain’s trauma response may rely more on other systems - like norepinephrine or the stress hormone cortisol. For these people, therapy is even more critical. Emerging treatments like MDMA-assisted therapy or ketamine are showing promise for treatment-resistant PTSD. Don’t give up - the right combination might still be out there.
Can I use marijuana or CBD for PTSD?
Some people report short-term relief from anxiety or sleep with CBD or marijuana. But research is mixed. High-THC products can worsen paranoia or flashbacks in PTSD. There’s no strong evidence that cannabis improves core PTSD symptoms long-term. The VA and APA don’t recommend it due to lack of controlled data and potential for dependence. If you’re using it, talk to your provider - don’t hide it. It might be interfering with your treatment.
What if I can’t afford therapy?
Many VA medical centers offer free trauma-focused therapy for veterans. Community mental health centers often have sliding-scale fees. Online platforms like BetterHelp or Talkspace may offer lower-cost options. Some universities with psychology programs run low-cost clinics staffed by supervised trainees. Don’t assume therapy is out of reach. Ask around. The VA’s PTSD Consultation Program (1-800-827-1000) can connect you to resources - even if you’re not a veteran.



Jennifer Littler
January 10, 2026 AT 19:41Just wanted to say prazosin changed my life. Nightmares were crippling - I’d wake up drenched in sweat, heart pounding, convinced I was back in the Humvee. Started at 1mg, bumped to 2mg after a week. Within 10 days, I slept through the night. No euphoria. No high. Just peace. I wish I’d known about this 5 years ago. Therapy helped, but prazosin made therapy possible.
Sam Davies
January 12, 2026 AT 15:35Oh wow. SSRIs are the ‘just take this and you’ll be fine’ band-aid for a broken spine. Of course the FDA only approved two - because Big Pharma doesn’t fund research on ‘cheap blood pressure drugs’ that actually work. Prazosin? That’s like finding a Ferrari in the junkyard. Meanwhile, my therapist charges $180/hour and still thinks ‘cognitive restructuring’ is a magic spell.
Alfred Schmidt
January 13, 2026 AT 07:38STOP TELLING PEOPLE TO JUST ‘DO THERAPY’ LIKE IT’S A CHOICE. You think I don’t want to sit in a room and talk about the ambush? I can’t even get out of bed before noon. SSRIs made me feel like a zombie. Prazosin made me feel human again. Now I can drive to the VA without hyperventilating. So yeah - medication isn’t a crutch. It’s the damn wheelchair.
Priscilla Kraft
January 13, 2026 AT 07:53Thank you for writing this 💙 I’ve been on sertraline for 14 months. Emotional blunting was brutal at first - felt like watching my life on mute. But after 6 months, I started noticing little things: I laughed at a dog chasing its tail. I remembered my mom’s voice. Therapy + meds = slow rebuild. Not magic. But real. And I’m still here. That’s enough for today. 🌱
Michael Patterson
January 14, 2026 AT 16:44So let me get this straight - you're saying that after decades of research, the best we've got is a couple of antidepressants that make people numb, a blood pressure pill that accidentally helps nightmares, and some fancy talk therapy that only works if you're not too depressed to leave the house? And we're calling this progress? The system is broken. We're treating symptoms like they're the disease. PTSD isn't a chemical imbalance - it's a soul wound. And we're handing out aspirin to someone who lost a leg.
Matthew Miller
January 15, 2026 AT 12:58Anyone who says MDMA-assisted therapy is the future is either a cult member or a pharma shill. You’re gonna give trauma survivors hallucinogens? That’s not treatment - that’s a rave with a therapist. And you think people won’t abuse it? Of course they will. This is America. We turn everything into a drug. Next up: PTSD IV drips with ketamine and a Spotify playlist.
Adewumi Gbotemi
January 17, 2026 AT 08:56Here in Nigeria, we don’t have SSRIs or therapists. We have family. We have prayers. We have silence that says, ‘I see you, you’re not alone.’ Maybe your science is good. But healing isn’t always in a pill or a clinic. Sometimes it’s just someone sitting with you while you cry. No diagnosis needed.
Sean Feng
January 18, 2026 AT 15:23Therapy works. Medication works. But most people don't do either. They just scroll Reddit and call it healing. Congrats. You read an article. Now go do the work.
Christian Basel
January 18, 2026 AT 18:15Let’s be real - the whole PTSD pharmacopeia is just a series of educated guesses. We don’t know why SSRIs help. We don’t know why prazosin works for nightmares. We just know that in some people, it does. Medicine is still archaeology - we dig up patterns, but we don’t understand the civilization that made them. The brain is a black box with a scream inside.
Alex Smith
January 20, 2026 AT 14:34Oh so now we’re gonna make PTSD a ‘treatment protocol’ instead of a human experience? Cool. Next they’ll give you a checklist: ‘☐ 8 therapy sessions ☐ 150mg sertraline ☐ 2mg prazosin ☐ 3x weekly yoga ☐ 1 existential crisis per month.’ Real progress. Meanwhile, I’m over here trying to remember what ‘calm’ feels like.
Roshan Joy
January 20, 2026 AT 18:05I’ve been through all of this - meds, therapy, even tried CBD (it made me paranoid). What finally helped? A veteran’s group in Delhi. No jargon. No scripts. Just people who knew what silence felt like. We didn’t talk about PTSD. We talked about chai, about missing our dogs, about how the rain sounds different now. Healing isn’t always clinical. Sometimes it’s just… being together.
Madhav Malhotra
January 22, 2026 AT 04:20Love how you mentioned prazosin - my cousin in Mumbai used it after a bus accident. He was scared to drive again. After 2 weeks on prazosin, he drove himself to the market. Just a small thing. But for him? It was freedom. No fancy therapy. Just a cheap pill and a lot of patience. Sometimes the simplest things are the most powerful.
Priya Patel
January 23, 2026 AT 00:59Okay but imagine if we treated broken bones like we treat PTSD: ‘Just walk it off, it’s in your head.’ We’d be in a nightmare. PTSD isn’t weakness. It’s a biological hostage situation. And we’re giving people bandaids while the kidnapper’s still in the room. Thank you for saying this out loud.
Jason Shriner
January 25, 2026 AT 00:14So the VA says ‘start with therapy’... but the waitlist is 18 months. Meanwhile, my PTSD is screaming every day. So I take the pill. And then I feel guilty because I’m not ‘doing the real work.’ But who’s to say the pill isn’t the real work? Maybe the work is just surviving long enough to get to therapy. Maybe the pill is the bridge. Maybe I’m not broken - maybe the system is.
Vincent Clarizio
January 26, 2026 AT 21:38You think this is the end of the story? Nah. This is just the first chapter of a 12-book series. We’re gonna have AI therapists that analyze your voice patterns and adjust your meds in real time. We’re gonna have neural implants that zap the fear center like a Nintendo controller. We’re gonna have PTSD gene therapy where you edit your DNA to stop remembering the trauma. And then we’ll all be like - ‘wait, why did we ever think a pill and a 45-minute chat were enough?’