Doctors prescribe generics more than ever-90% of all prescriptions in the U.S. are for generic drugs. But here’s the problem: many clinicians still don’t fully trust them.
It’s not about skepticism out of ignorance. It’s about confusion. A 2017 study found that 68% of physicians had at least some doubt about whether generics work the same as brand-name drugs. Even though the FDA requires generics to have the exact same active ingredient, strength, and route of administration, many providers still believe there’s a hidden difference. Some think the inactive ingredients matter more than they do. Others worry the manufacturing standards aren’t as strict. A 2020 survey showed 45% of prescribers incorrectly thought generics must have identical inactive ingredients. Another 27% believed generics could contain up to 25% less active ingredient. None of that is true.
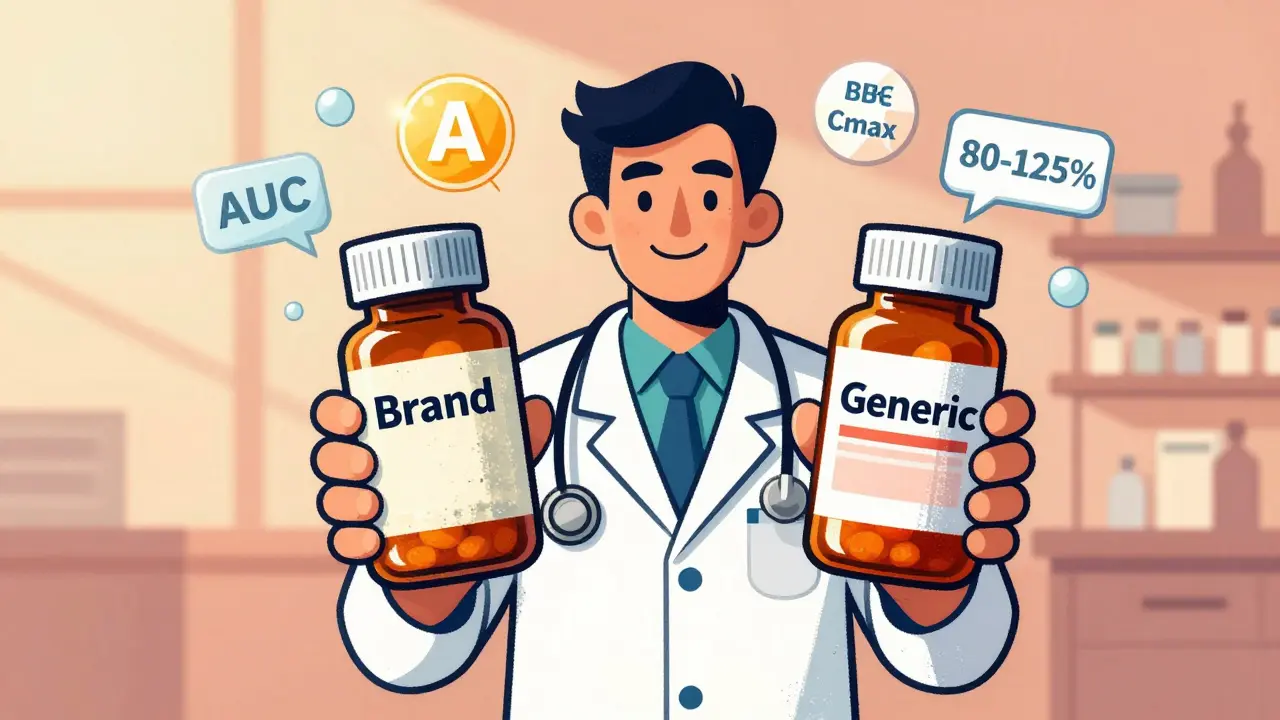
The FDA’s standards for generic approval are brutal. To get approved, a generic drug must prove it’s bioequivalent to the brand-name version. That means the amount of drug absorbed into the bloodstream-measured by AUC and Cmax-must fall within 80% to 125% of the brand’s levels. That’s not a wide margin. It’s a tight, scientifically proven window. And it’s not just one study. It’s dozens of tests across hundreds of patients. The FDA’s Orange Book lists every approved generic with a therapeutic equivalence rating: an "A" means it’s interchangeable. A "B" means it’s not. Most generics are "A."
So why do so many doctors still reach for the brand name? Partly because of habit. Many learned to prescribe by brand during training. "Lopressor," not "metoprolol." "Zoloft," not "sertraline." When a resident hears their attending say "Lopressor twice daily," they don’t always catch that it’s the same as the generic they just ordered. A Reddit thread from a third-year med student captured it perfectly: "I nearly prescribed two doses because my attending didn’t say it was generic."
Another reason? Time. A 2021 AMA survey found that 89% of physicians feel they don’t have enough time in a visit to explain generics to patients. But skipping that conversation costs more than time-it costs adherence. Patients are 35% more likely to start and stick with a medication if it’s generic. Why? Because it’s cheaper. And when patients don’t take their meds because of cost, hospitalizations go up. Studies show that for chronic conditions like hypertension or diabetes, switching from brand to generic can cut emergency visits by up to 20%.
Here’s where education makes the biggest difference: communication. When a provider says, "This generic works just like the brand," patients believe them. But when they say, "It’s the same, but cheaper," patients hear, "It’s the cheap version." The wording matters. Harvard Medical School research showed that when doctors explicitly endorsed generic equivalence, patient-reported side effects dropped by 18%. That’s not placebo. That’s nocebo-the flip side. When patients expect side effects, they often feel them, even if the drug is identical.
Some specialties struggle more than others. Cardiologists and neurologists are the most hesitant. One survey found 82% of cardiologists and 79% of neurologists hesitate to prescribe generics, even when the evidence is clear. Why? Because they treat conditions where small changes can feel risky-like seizures or heart rhythm disorders. But data doesn’t back up the fear. A 2023 analysis of over 1.2 million prescriptions for generic antiepileptics found no increase in seizure frequency compared to brand-name versions. The same goes for blood pressure meds. The FDA has reviewed thousands of studies on this. The science is solid.
But not all education works the same. Just handing out a PDF? That’s not enough. A 2021 JAMA study compared two approaches: one group got a 10-page fact sheet. The other got four 90-minute interactive sessions over six months, with real patient cases and feedback. Six months later, the interactive group had 42% higher knowledge retention. Spaced learning works. Repeating concepts over time builds confidence. One health system in California cut brand-name statin prescriptions by 37% after rolling out monthly case discussions with pharmacists and residents.
Technology is helping too. Some EHR systems now pop up a reminder when a prescriber reaches for a brand-name drug: "This generic is FDA-approved equivalent. Cost: $4 vs. $120." In a 2023 pilot, that simple nudge increased generic prescribing by 24%. AI tools are getting smarter. UnitedHealthcare’s 2024 pilot used machine learning to identify doctors who rarely prescribed generics-and then sent them personalized case studies based on their own patient data. Result? A 28% jump in generic use.
State laws add another layer of complexity. In 34 states, pharmacists can swap a brand for a generic without telling the doctor. In 16 states, the prescriber must write "dispense as written" to block substitution. That means a patient might get a different pill than expected-and if the provider didn’t explain it, they might think something went wrong. Education needs to cover not just the science, but the system.
The biggest barrier isn’t knowledge-it’s mindset. Many providers still believe that because a drug is cheaper, it must be worse. But generics save the U.S. healthcare system $2.2 trillion every decade. That’s not a rounding error. That’s lives saved, hospital stays avoided, and families protected from medical debt. And it’s not just about money. It’s about access. A patient on a fixed income won’t refill a $120 pill. They’ll refill a $4 one. That’s the difference between managing a condition and losing control of it.
There’s one exception that keeps coming up: levothyroxine. Some studies suggest brand-name Synthroid has more consistent absorption than generics, especially in patients with thyroid cancer or severe hypothyroidism. But the FDA and most endocrinology societies say the difference is minimal and not clinically meaningful for most patients. The controversy exists, yes-but it’s narrow. It doesn’t invalidate the broader rule.
And then there’s the rise of biosimilars. They’re not generics. They’re complex biological drugs, like those for rheumatoid arthritis or cancer. Only 31% of providers can correctly explain the difference. That’s a growing problem. Education must evolve to cover both small-molecule generics and biologics. The FDA’s 2023 virtual reality training module simulates patient conversations about biosimilars. Early results show a 41% boost in provider confidence.
So what can you do? Start with the FDA’s free resources. The Generic Drug Facts Handout is 148KB. The Therapeutic Equivalence guide is even shorter. Bookmark the Orange Book. Learn how to read an "A" rating. Attend a CME session-63% of physicians on Sermo say they want more. Talk to your pharmacist. Ask: "Is this generic approved? Is it rated A?" Then say it to your patient: "This is the same medicine. It’s just less expensive. You’ll get the same result."
Change doesn’t come from mandates. It comes from clarity. When providers know the science, trust the data, and communicate with confidence, patients follow. And that’s the real win.
What’s the real cost of not educating providers on generics?
It’s not just dollars. It’s missed doses. Hospital admissions. Worsening chronic disease. A 2020 ASPE study found that patients who couldn’t afford their brand-name meds were twice as likely to skip doses or stop entirely. That’s not patient noncompliance. That’s system failure. When providers don’t lead with generics, they’re not just missing a cost-saving opportunity-they’re setting patients up for failure.
Why do some doctors still prefer brand names even when generics are available?
Habit, training, and fear. Many were taught to prescribe by brand during medical school. They’ve never had a bad experience with a brand drug, so they stick with what’s familiar. Others worry about liability-"What if something goes wrong?" But data shows no increase in adverse events with generics. The fear is real, but the risk isn’t.
Can pharmacists substitute generics without a doctor’s permission?
Yes-in 34 states. Pharmacists can swap a brand for a generic if the prescription doesn’t say "dispense as written." In 19 states, they can substitute even without that note. But if the prescriber didn’t explain the switch to the patient, confusion follows. That’s why provider education must include communication about substitution.
How do you know if a generic is truly equivalent to the brand?
Check the FDA’s Orange Book. Look for an "A" rating. That means the generic is therapeutically equivalent. The FDA requires identical active ingredients, strength, dosage form, and route of administration. Bioequivalence is proven through rigorous testing. No "A" rating? Don’t assume it’s safe to substitute.
Are biosimilars the same as generics?
No. Generics are exact copies of small-molecule drugs. Biosimilars are highly similar-but not identical-to complex biological drugs like Humira or Enbrel. They’re harder to replicate. Only 31% of providers can correctly explain the difference. Education on biosimilars is now a critical part of provider training.
What’s the best way to talk to patients about generics?
Don’t say, "It’s cheaper." Say, "This is the same medicine as the brand. The FDA says it works just as well. It’s just less expensive, so you’re more likely to afford it long-term." Endorsement from the provider is the #1 factor in patient acceptance. Studies show patients are 3.2 times more likely to take a generic if their doctor says it’s equal.
Is there evidence that generic education improves patient outcomes?
Yes. A 2022 study showed that when providers received interactive, case-based education, generic prescribing increased by 29%. Patients on those prescriptions were 35% more likely to start their meds and 12-15% more likely to stay on them long-term. That’s adherence. That’s better health. That’s fewer ER visits.
What resources are available for providers to learn about generics?
The FDA offers free tools: the Generic Drug Facts Handout, the Therapeutic Equivalence Guide, and the Generic Drugs Stakeholder Toolkit. The Generic Pharmaceutical Association (GPhA) has online modules. Academic medical centers like UCSF and Brigham and Women’s have built their own curricula. CME credits are available through professional societies. Start with the FDA. It’s free, credible, and updated regularly.
Will CMS or insurance companies push providers to prescribe more generics?
Yes. Starting in 2025, Medicare’s Merit-based Incentive Payment System (MIPS) will include generic prescribing rates as a quality metric. Health systems are already tying bonuses to generic use. The financial incentive is shifting. But the real driver should be patient care-not payment.
What’s the future of provider education on generics?
Personalized, just-in-time learning. AI will identify doctors who rarely prescribe generics and serve them targeted case studies. EHRs will auto-suggest alternatives at the point of care. VR simulations will train communication skills. The goal isn’t just knowledge-it’s behavior change. And the data shows it’s working.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove bioequivalence-meaning the amount of drug absorbed into the bloodstream falls within 80-125% of the brand’s levels. Thousands of studies confirm this. For 90% of prescriptions, generics work just as well.
Why do some doctors still prescribe brand-name drugs over generics?
Many learned to prescribe by brand during training and stick with familiar names. Others worry about subtle differences in inactive ingredients or manufacturing, even though the FDA ensures safety and equivalence. Time pressures and patient expectations also play a role. But data shows these concerns are often based on myths, not evidence.
Can pharmacists switch a brand-name drug to a generic without asking the doctor?
In 34 states, yes-unless the prescription says "dispense as written." In 19 states, pharmacists can substitute even without that note. But if the prescriber hasn’t explained the switch to the patient, confusion and mistrust can follow. That’s why provider education must include how to talk about substitutions.
How can I check if a generic drug is approved and equivalent?
Use the FDA’s Orange Book, which lists all approved drugs and their therapeutic equivalence ratings. Look for an "A" rating-this means the generic is interchangeable with the brand. Avoid drugs with a "B" rating unless there’s a specific clinical reason.
Do generics have the same side effects as brand-name drugs?
Yes. Since they contain the same active ingredient, side effects are the same. But patients often report more side effects with generics-not because the drug is different, but because they expect them. When providers explicitly endorse equivalence, patient-reported side effects drop by up to 18%.
Are biosimilars the same as generics?
No. Generics are exact copies of small-molecule drugs. Biosimilars are highly similar to complex biological drugs (like those for cancer or autoimmune diseases), but not identical. They’re harder to produce and require different approval standards. Only 31% of providers can correctly explain the difference.
What’s the best way to encourage patients to accept generics?
Don’t just say it’s cheaper. Say: "This is the same medicine as the brand. The FDA says it works just as well. It’s less expensive, so you’re more likely to afford it long-term." Provider endorsement is the strongest predictor of patient acceptance-studies show patients are 3.2 times more likely to take a generic if their doctor says it’s equal.
Is there proof that educating providers improves generic use?
Yes. Interactive, case-based education improves knowledge retention by 42% compared to static handouts. Clinicians who receive this training increase generic prescribing by 29%. Patients on those prescriptions are 35% more likely to start and stay on their meds. The result: better health and lower costs.
Where can I find reliable education materials on generics?
The FDA offers free, authoritative resources: the Generic Drug Facts Handout, the Orange Book, and the Generic Drugs Stakeholder Toolkit. The Generic Pharmaceutical Association (GPhA) also provides online modules. Academic medical centers like UCSF and Brigham and Women’s have developed their own curricula. Start with the FDA-it’s free, updated regularly, and trusted by clinicians nationwide.
Will future healthcare policies require more generic prescribing?
Yes. Starting in 2025, Medicare’s MIPS program will include generic prescribing rates as a quality metric. Insurance companies and health systems are already tying bonuses to higher generic use. But the goal should be better patient outcomes-not just cost savings.


Swapneel Mehta
December 20, 2025 AT 01:45Been prescribing generics for 12 years. Never had a patient come back saying the generic didn't work. The science is rock solid. It's all about perception, not pharmacology.
Teya Derksen Friesen
December 21, 2025 AT 03:41It is imperative that healthcare professionals recognize the empirical evidence supporting the therapeutic equivalence of generic medications. The regulatory rigor applied by the FDA ensures that bioequivalence thresholds are not merely met, but consistently validated across diverse patient populations. This is not an opinion-it is a clinical imperative.
Jason Silva
December 22, 2025 AT 21:39Bro… the FDA is in bed with Big Pharma. 🤫 You think they really test every single generic? Nah. They just rubber-stamp it. I’ve seen people have seizures after switching to generic Keppra. Coincidence? I think not. 😈
Southern NH Pagan Pride
December 23, 2025 AT 19:13the fda’s ‘bioequivalence’ range is 80-125%?? that’s not equivalence, that’s a f***ing lottery. and what about the fillers? talc, dyes, lactose-some folks are allergic to those and no one tells them. this is a slow poison. 🤢
Orlando Marquez Jr
December 23, 2025 AT 19:38As a physician trained in both U.S. and international systems, I can attest that the global consensus on generic drug equivalence is remarkably consistent. The WHO’s Essential Medicines List, the European Medicines Agency’s guidelines, and the FDA’s Orange Book all converge on the same conclusion: when properly rated, generics are therapeutically interchangeable. This is not a U.S.-specific phenomenon-it is evidence-based medicine.
John Hay
December 23, 2025 AT 20:58I used to prescribe brand names out of habit. Then I started asking patients: ‘Would you rather pay $4 or $120?’ Half said they’d skip it. I switched. Now my adherence rates are up. Simple.
Jon Paramore
December 25, 2025 AT 20:18The 80–125% AUC/Cmax bioequivalence window is statistically robust, validated by over 1,200 peer-reviewed studies. The FDA’s requirement for within-subject variability control eliminates interpatient noise. The myth that generics are ‘less potent’ stems from confounding pharmacokinetic variability in uncontrolled settings-not actual pharmacologic inferiority. The Orange Book’s ‘A’ rating is the gold standard. If it’s not rated ‘A,’ don’t substitute. But if it is? You’re not compromising care-you’re optimizing access.
Cameron Hoover
December 27, 2025 AT 01:15I used to think generics were ‘good enough.’ Then I saw a 78-year-old with heart failure refill her metoprolol for $3 instead of $117. She cried. Said she was going to stop. I realized-I wasn’t just prescribing medicine. I was prescribing dignity. Now I say it out loud: ‘This is the same pill. Just cheaper. You deserve to take it.’
Stacey Smith
December 27, 2025 AT 05:29America’s healthcare system is broken, but generics are one of the few things still working right. Stop letting fear and misinformation kill patients. Prescribe the generic. Save money. Save lives.
Ben Warren
December 29, 2025 AT 03:24Let us not be naive. The entire generic drug approval paradigm is a regulatory fiction engineered to benefit corporate profit margins under the guise of cost containment. The 80–125% bioequivalence window is a mathematical loophole that permits pharmacologically divergent products to be labeled as ‘interchangeable.’ When you consider the documented variability in dissolution profiles across manufacturing batches-especially from overseas facilities with lax oversight-the notion that a generic is ‘the same’ as a brand-name drug is not merely misleading-it is ethically indefensible. The FDA’s Orange Book is not a scientific document; it is a corporate compliance checklist. And the fact that clinicians still trust it reveals a systemic failure of medical education, not a triumph of evidence.
Hannah Taylor
December 29, 2025 AT 20:39generic levothyroxine gave me heart palpitations. switched back to synthroid and i’m fine. they say it’s ‘not clinically significant’ but my body says otherwise. the fda doesn’t know what my thyroid feels like. also, i think they put fluoride in the generics to keep us docile. 🤔
Michael Ochieng
December 30, 2025 AT 17:06As a Nigerian-born physician practicing in Texas, I’ve seen this play out in both countries. In Lagos, patients beg for generics because they can’t afford anything else. Here, providers hesitate because they’ve been told generics are ‘second-rate.’ The truth? The same pill, made in the same factory (sometimes), just labeled differently. We need to stop treating patients like they’re too fragile to handle the truth. Tell them: ‘This is the same medicine. It’s just priced right.’ That’s all they need to hear.