Hyperthyroidism-Stimulant Risk Calculator
Calculate Your Risk
When your thyroid is overactive, your body is already running on high gear. Your heart races. You feel jittery. Sleep is impossible. Then you take a stimulant like Adderall or Ritalin - and everything spirals. This isn’t just a bad day. It’s a dangerous medical intersection that too many people don’t see coming.
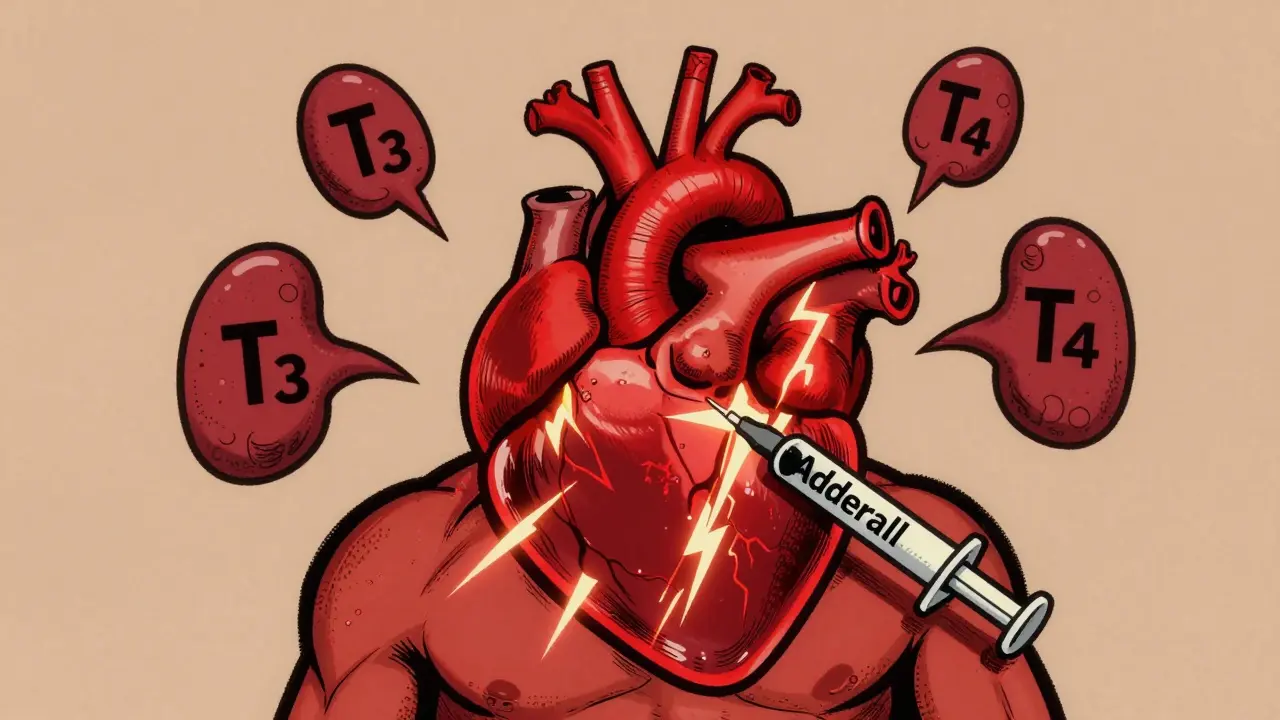
Why Hyperthyroidism and Stimulants Don’t Mix
Hyperthyroidism means your thyroid gland is pumping out too much T3 and T4. These hormones control your metabolism, heart rate, and nervous system. When they’re too high, your body is in constant overdrive. Now add a stimulant - a drug designed to boost alertness by flooding your brain with norepinephrine and dopamine - and you’re essentially stepping on the gas while someone else is already holding the brake pedal down. The result? A dangerous synergy. Studies show hyperthyroidism makes your heart’s beta-receptors 30-40% more sensitive to adrenaline-like chemicals. Adderall, which can spike norepinephrine levels by 300-500%, hits a system already primed for overload. Resting heart rates jump from normal 60-100 bpm to 120-160 bpm. Blood pressure can spike 10-15 mmHg higher than in healthy people on the same dose. That’s not just discomfort - it’s a path to atrial fibrillation, heart attack, or even sudden cardiac arrest.What the Data Says About Real-World Risks
The numbers don’t lie. Patients with untreated hyperthyroidism who take stimulants have a 3.2-fold higher risk of developing atrial fibrillation than those with hyperthyroidism alone. A 2022 meta-analysis found Adderall increases heart rate 28% more than methylphenidate at equivalent doses. That difference matters. One patient on Reddit described their heart racing at 140 bpm after taking Adderall - an ER visit followed. Another passed out from palpitations. These aren’t rare outliers. Drugs.com reports 68% of hyperthyroid patients on Adderall say their symptoms got worse. Only 24% of non-thyroid users say the same. Anxiety isn’t just a side effect - it’s a direct result. Thyroid UK found 78% of hyperthyroid patients on stimulants report severe anxiety, compared to 22% of those not taking them. That’s not “nervousness.” It’s panic attacks, trembling, feeling like you’re going to die - even when you’re sitting still.Why Misdiagnosis Is Common - and Deadly
Here’s the hidden trap: hyperthyroidism mimics ADHD. Weight loss. Trouble focusing. Restlessness. Insomnia. Irritability. These are textbook ADHD symptoms. But they’re also classic signs of an overactive thyroid. A 2022 Paloma Health survey found 41% of adults diagnosed with ADHD had undiagnosed thyroid problems. When they treated the thyroid condition instead of prescribing stimulants, 33% saw their symptoms vanish. The American Thyroid Association says ruling out thyroid dysfunction before diagnosing ADHD is crucial. Too many doctors skip thyroid tests because they assume the symptoms are “just anxiety” or “typical ADHD.” But when you treat the wrong thing, you make the patient sicker. A 2021 study in Thyroid found stimulants can even lower thyroxine (T4) levels in children, making thyroid management harder.
Which Stimulants Are Riskiest?
Not all stimulants are created equal. Adderall (amphetamine salts) carries the highest cardiac risk. Its 75% dextroamphetamine component hits fast and hard. The American College of Cardiology warns that high-dose Adderall (>30mg/day) increases the risk of ventricular tachycardia by 4.7-fold in hyperthyroid patients. Methylphenidate (Ritalin, Concerta) is less aggressive. It doesn’t release neurotransmitters - it blocks their reuptake. That means slower, steadier effects. For patients with mild subclinical hyperthyroidism (TSH 0.1-0.4 mIU/L), low-dose methylphenidate (<18mg/day) may be considered with strict monitoring. But even then, it’s not risk-free. Vyvanse (lisdexamfetamine) has a slower onset, which can reduce peak heart rate spikes by 15-20% compared to immediate-release Adderall. Still, it’s an amphetamine derivative. The Endocrine Society says Adderall is typically not recommended for anyone with hyperthyroidism - full stop.Safe Alternatives Exist
If you have hyperthyroidism and need treatment for ADHD or another condition, you’re not out of options. Non-stimulant medications like atomoxetine (Strattera) are a safer bet. They raise heart rate by only 2-3 bpm - regardless of thyroid status. That’s the difference between a gentle nudge and a sledgehammer. Behavioral therapy, structured routines, and lifestyle changes can also help manage focus and impulsivity without drugs. For many, treating the thyroid condition alone resolves ADHD-like symptoms. One patient described it this way: “I was on Adderall for three years. When I finally got my thyroid right, I didn’t need the stimulant anymore.”What You Need to Do - Step by Step
If you’re on thyroid medication or suspect you have hyperthyroidism, here’s what to do:- Get tested. Request a full thyroid panel: TSH, free T3, free T4. Don’t rely on TSH alone - some patients have normal TSH but high T3.
- Hold off on stimulants. Don’t start Adderall, Ritalin, or Vyvanse until your thyroid is stable and your doctor confirms it’s under control.
- Ask for baseline cardiac screening. If stimulants are unavoidable, get an ECG and 24-hour Holter monitor first. Know your resting heart rate before you start.
- Start low, go slow. If approved, begin with the lowest possible dose (5-10mg methylphenidate or Adderall). Monitor heart rate and anxiety daily.
- Know the red flags. Heart rate over 110 bpm at rest. Chest pain. Panic attacks lasting more than 2 hours. Dizziness or fainting. Stop the drug and call your doctor immediately.
- Re-test regularly. The Endocrine Society recommends thyroid function tests every 3 months when adjusting medications. Levels can shift with age, stress, or other drugs.

What Your Doctor Should Be Doing
Doctors are catching on - slowly. In 2018, only 12% of psychiatrists ordered thyroid tests before prescribing stimulants. By 2022, that number jumped to 27%. The American Academy of Pediatrics now requires thyroid testing in children with atypical ADHD symptoms. The FDA added thyroid monitoring recommendations to stimulant labels in 2022. But it’s not enough. Too many patients still slip through the cracks. If your doctor hasn’t checked your thyroid before prescribing a stimulant, ask why. If they say “it’s not necessary,” get a second opinion. Your heart isn’t a gamble.The Bigger Picture
More than 114 million prescriptions for levothyroxine were filled in the U.S. in 2022. Adderall XR got 25.6 million. With ADHD diagnoses up 42% since 2016, the overlap is growing. Every time a hyperthyroid patient is misdiagnosed with ADHD and given a stimulant, the risk of cardiac event rises. The Endocrine Society calls this a public health concern - and they’re right. The solution isn’t to ban stimulants. It’s to test first. Treat the thyroid. Then reassess. Too often, we treat symptoms instead of causes. In this case, fixing the thyroid can eliminate the need for stimulants altogether.Final Word: Don’t Guess. Test.
If you have symptoms of anxiety, rapid heartbeat, unexplained weight loss, or trouble focusing - don’t assume it’s ADHD. Don’t assume it’s just stress. Get your thyroid checked. It’s a simple blood test. It takes 10 minutes. It could save your life.Stimulants aren’t the enemy. But they’re not safe for everyone. When your thyroid is out of balance, they become a ticking time bomb. The science is clear. The warnings are loud. Now it’s up to you - and your doctor - to act before it’s too late.
Can I take Adderall if I have hyperthyroidism?
No, Adderall is generally contraindicated in patients with hyperthyroidism. The combination significantly increases heart rate and blood pressure, raising the risk of atrial fibrillation, ventricular tachycardia, and sudden cardiac events. The Endocrine Society and FDA both warn against its use in this population. Even low doses carry serious risks.
Can methylphenidate (Ritalin) be safer than Adderall with hyperthyroidism?
Methylphenidate is generally less risky than Adderall because it doesn’t force neurotransmitter release - it blocks reuptake. This leads to a slower, steadier effect. For patients with mild subclinical hyperthyroidism (TSH 0.1-0.4 mIU/L), low-dose methylphenidate (5-18mg/day) may be used under strict cardiac monitoring. But it’s not risk-free. Always test thyroid levels first and monitor heart rate daily.
Can hyperthyroidism be mistaken for ADHD?
Yes, very commonly. Symptoms like restlessness, poor concentration, weight loss, irritability, and insomnia are shared by both conditions. Studies show up to 41% of adults diagnosed with ADHD actually have undiagnosed thyroid dysfunction. Treating the thyroid often resolves these symptoms without stimulants. Always get a full thyroid panel before starting ADHD medication.
What are the warning signs that stimulants are harming me with hyperthyroidism?
Watch for: resting heart rate above 110 bpm, chest pain or pressure, palpitations that don’t fade, dizziness or fainting, panic attacks lasting more than 2 hours, severe tremors, or sudden shortness of breath. If you experience any of these, stop the medication immediately and seek medical help. These aren’t side effects - they’re red flags for cardiac stress.
Do I need to stop my thyroid medication if I take stimulants?
No - but you must space them out. Take thyroid medication (like levothyroxine) at least 4 hours before or after stimulants, calcium, iron, or antacids, which can interfere with absorption. Never stop thyroid medication without medical supervision. The goal is to stabilize your thyroid first, then decide if stimulants are even needed.
Are there non-stimulant options for ADHD with hyperthyroidism?
Yes. Atomoxetine (Strattera) is a non-stimulant that raises heart rate by only 2-3 bpm, regardless of thyroid status. It’s FDA-approved for ADHD and carries far less cardiac risk. Behavioral therapy, exercise, sleep hygiene, and mindfulness techniques can also help manage symptoms without drugs. Many patients find they no longer need stimulants once their thyroid is properly treated.




John O'Brien
January 28, 2026 AT 02:39Bro, I was on Adderall for 3 years with undiagnosed Graves'. One day I collapsed at work. ER said my heart was firing like a machine gun. They didn't even check my thyroid till I begged them. Now I'm off stimulants, on methimazole, and actually sleeping. Don't be me.
astrid cook
January 29, 2026 AT 15:15Wow. Just... wow. So now we're blaming ADD meds for people who can't even get their thyroid under control? I mean, if you're that unstable, maybe you shouldn't be on anything. I've seen people self-diagnose thyroid stuff on TikTok and then refuse real treatment. This is just another cry for sympathy.
April Williams
January 31, 2026 AT 02:43THIS. I was prescribed Adderall at 19 because I was 'too distracted.' Turns out my TSH was 0.02. I had panic attacks so bad I thought I was dying. My doctor didn't even order a thyroid panel until I showed up with a printout of this exact article. They called me 'overly dramatic.' I was 19. I didn't know what a TSH was. Now I'm 28, off all stimulants, and finally stable. Don't let them gaslight you into a cardiac event.
Desaundrea Morton-Pusey
February 1, 2026 AT 13:04So let me get this straight - you’re saying America’s ADHD epidemic is just people with thyroid issues? That’s just lazy. If you can’t focus, take the pill. Stop blaming your body for not being perfect. Also, Adderall isn’t a death sentence. My uncle’s been on it since ‘98 and he’s still running marathons.
Murphy Game
February 3, 2026 AT 01:29Did you know the FDA quietly changed the Adderall label in 2020 to include a 'thyroid caution' but buried it in section 8.3? And the pharmaceutical reps still tell docs it's 'safe if monitored.' I’ve got screenshots of emails from reps telling med reps to 'downplay thyroid risks.' This isn’t negligence. It’s profit-driven murder.
Kegan Powell
February 3, 2026 AT 03:03man i just want to say thank you for writing this
it took me 7 years to figure out my 'anxiety' was my thyroid
and every time i took a stimulant i felt like my chest was going to explode
now i'm off everything, on levothyroxine, and i actually like my own skin again
you're not broken
you're just misdiagnosed
and that's not your fault 💙
Harry Henderson
February 4, 2026 AT 10:51STOP GIVING IN. You think you need Adderall to function? You don't. You think you're lazy? You're not. You're hypothyroid or hyperthyroid. Get tested. Get treated. Sleep. Eat real food. Move your body. No pill fixes what your body is screaming at you to fix. I was on 60mg Adderall daily. Now I'm off it. I run 5Ks. I sleep 8 hours. I'm 32. I'm not dying for a prescription.
suhail ahmed
February 6, 2026 AT 05:31in India we call this 'jugaad' - patching a broken system with bandaids. Doctors here slap on Adderall like it's chai. Thyroid tests? 'Too expensive.' I had a student come to me with heart palpitations - turned out his TSH was 0.05. We got him tested through a nonprofit. Now he's calm. No pills. Just iodine, sleep, and a damn good doctor. We need to stop treating symptoms and start treating people.
Andrew Clausen
February 7, 2026 AT 04:26The data cited is statistically significant but not causally proven. Correlation does not equal causation. Furthermore, the claim that '68% of hyperthyroid patients on Adderall report worsening symptoms' is misleading - no control group for symptom severity pre-medication is provided. Additionally, the study from Thyroid mentioning lowered T4 levels in children was conducted on a cohort of 17 patients over 6 weeks - insufficient for generalization. Please cite peer-reviewed meta-analyses with adjusted confounders before making sweeping clinical assertions.
Kirstin Santiago
February 8, 2026 AT 18:21I had the same experience. Thought I had ADHD. Took Ritalin. Felt like my heart was trying to escape my chest. Went to a new endocrinologist - TSH 0.07, free T4 sky-high. Stopped the med. Started treatment. Within two weeks, my anxiety dropped 80%. I didn't need stimulants. I needed a thyroid specialist. If you're reading this and feel like your body's on fire - get tested. It's not your fault.
Conor Flannelly
February 9, 2026 AT 11:26My cousin in Dublin was diagnosed with ADHD at 16. Took Concerta for 4 years. Went to the ER with atrial fibrillation. Turned out she had silent Graves'. She’s now off everything, on carbimazole, and actually has a social life. The system failed her. Not her. We need mandatory thyroid screening before prescribing stimulants - especially in teens. It’s not complicated. It’s just ignored.
Conor Murphy
February 10, 2026 AT 14:05Thank you for this. I'm a nurse and I've seen too many young people come in scared, shaking, heart racing - and the doc just says 'take less Adderall.' No one checks the thyroid. I started pushing for TSH tests on every new ADHD patient. 1 in 5 had thyroid issues. Changed their lives. You're not alone. Keep speaking up 🙏