
Statin Myopathy Risk Assessment Tool
This tool uses the Statin-Associated Muscle Symptom Clinical Index (SAMS-CI) to determine your likelihood of tolerating statins again. Based on clinical evidence from major guidelines, this 5-question assessment helps you and your doctor decide if rechallenge is appropriate.
Answer the following 5 questions about your symptoms and medical history. The SAMS-CI scores range from 0-12, with lower scores indicating better tolerance for statin rechallenge.
- Score below 5: 91% chance of tolerating rechallenge
- Score 5-7: Moderate risk
- Score above 7: Likely true statin intolerance
Your SAMS-CI Score
Stopping statins because of muscle pain sounds like a smart move-until you realize how much risk you’re taking. Statins cut heart attacks and strokes by up to 30% in high-risk patients. But if your muscles ache, cramp, or feel weak after starting one, it’s easy to quit. The problem? Most of the time, the pain isn’t even from the statin. And if you never try again, you’re leaving your heart unprotected.
What Exactly Is Statin-Induced Myopathy?
Statin-induced myopathy isn’t one thing. It’s a range of muscle issues, from mild soreness to rare but dangerous rhabdomyolysis-where muscle breaks down so badly it can wreck your kidneys. The most common sign is muscle pain without obvious cause, especially in the thighs or shoulders. But here’s the twist: in clinical trials, about 5% of people on statins report muscle pain. So do 5% of people on sugar pills. That means for most, the pain isn’t caused by the drug. It’s the nocebo effect-the mind expecting harm, and then feeling it.
True statin myopathy shows up with high creatine kinase (CK) levels-usually more than 10 times the normal range. Rhabdomyolysis, the extreme version, hits when CK is over 40 times normal. That’s rare-less than 1 in 1,000 users. But when it happens, you stop statins forever. No exceptions.
Why Rechallenge Isn’t Just an Option-It’s a Necessity
Most people who quit statins because of muscle pain never get them back. A 2021 survey found 73% of patients weren’t even offered a rechallenge plan. That’s a problem. Stopping statins for even four weeks can destabilize artery plaques. That’s not theoretical-it’s backed by data from the 2022 PMC review. For someone who had a heart attack or has diabetes and high cholesterol, going off statins is like turning off a fire alarm and then wondering why the house burned down.
Rechallenge isn’t about pushing through pain. It’s about finding the right version of the drug that works for your body. And it works-most of the time. Studies show 60-80% of people who try again can get back on statins safely, using smart strategies.
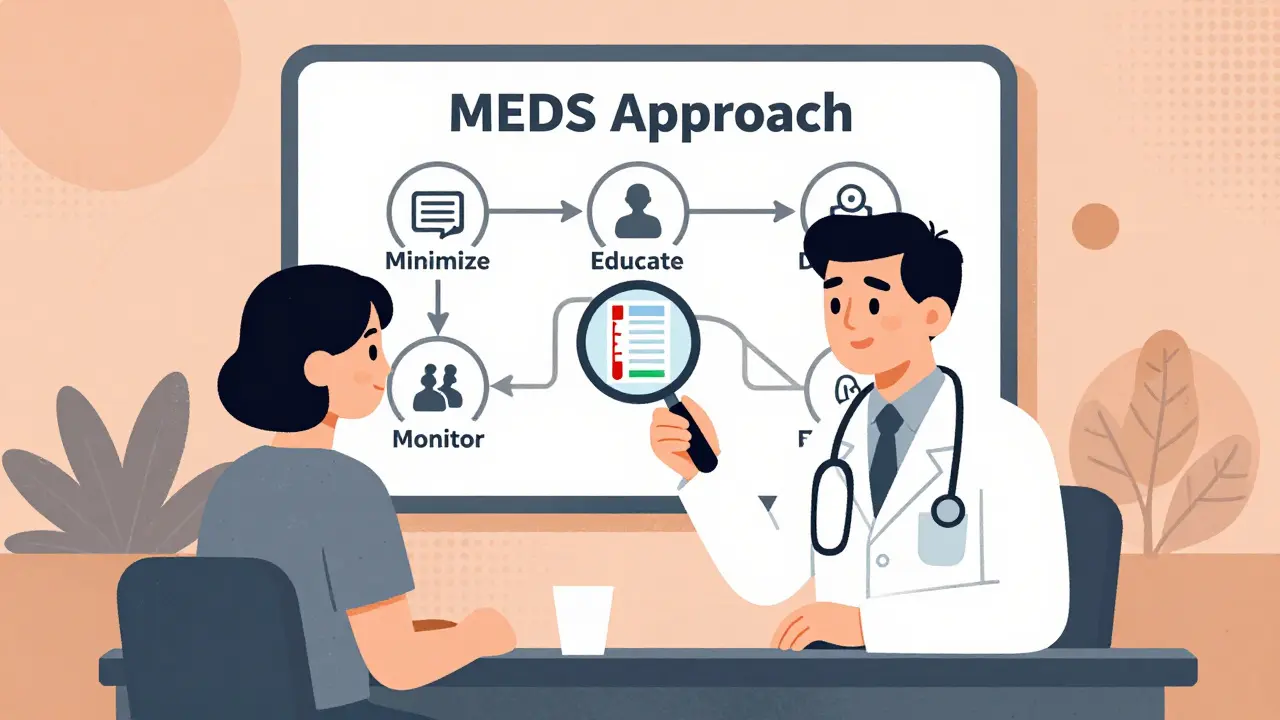
The MEDS Approach: A Proven Roadmap
The International Lipid Expert Panel built a simple, evidence-backed system called MEDS:
- Minimize time off statins-don’t wait months. Aim for 2-4 weeks after symptoms fade.
- Educate the patient-explain the nocebo effect. Many think their pain is the statin, but it’s often their fear.
- Diet and nutraceuticals-coenzyme Q10, vitamin D, and omega-3s may help reduce muscle symptoms. They won’t fix everything, but they can lower the statin dose you need.
- Systematic monitoring-track symptoms and check CK levels 2-4 weeks after restarting.
This isn’t guesswork. It’s a protocol used in lipid clinics where 85% of providers follow it. Primary care doctors? Only 43% do. That gap is costing lives.
Which Statin Should You Try Next?
Not all statins are created equal. Some are more likely to cause muscle problems. If you had trouble with simvastatin or atorvastatin, switching can make all the difference.
Lowest risk for muscle issues:
- Pravastatin
- Fluvastatin
- Pitavastatin
Higher risk:
- Simvastatin (especially 80mg-now mostly avoided)
- Atorvastatin (high dose)
Real-world data from the American Heart Association Support Network shows 41% of people who switched from simvastatin to pravastatin stayed on it long-term with no issues. That’s not luck. It’s pharmacology. Pravastatin doesn’t rely as much on liver enzymes that can build up in some people.
Dosing Tricks That Work
You don’t have to take a statin every day to get results. For many, every-other-day dosing works just as well.
For example:
- Switch from 40mg atorvastatin daily → 20mg every other day
- Switch from 20mg rosuvastatin daily → 10mg every other day
Why? Statins like atorvastatin and rosuvastatin have long half-lives-they stick around in your blood for days. So skipping a day doesn’t mean your LDL spikes. In fact, 29% of successful rechallenges in patient forums used this method. It cuts the dose in half, which dramatically lowers muscle risk.
When NOT to Rechallenge
There are two red flags that mean: Don’t try again.
1. Immune-mediated necrotizing myopathy (IMNM)-This is rare, but deadly if missed. It’s confirmed by a blood test for anti-HMGCR antibodies. If positive, your immune system is attacking your own muscle tissue because of the statin. You need immunosuppressants, not another statin. Restarting will make it worse.
2. Rhabdomyolysis-If your CK was over 40x normal, you had a medical emergency. The American Heart Association is clear: never restart statins. The risk isn’t worth it. Switch to alternatives.
What If You Can’t Tolerate Any Statin?
For 20-30% of people, even the lowest dose or every-other-day schedule brings back pain. That’s when you need plan B.
Best alternatives:
- PCSK9 inhibitors (evolocumab, alirocumab): Injected every 2-4 weeks. Lower LDL by 50-60%. Proven to reduce heart attacks and strokes. Cost? Around $5,850 a month. But many insurers cover it if you’ve tried and failed statins.
- Ezetimibe: A pill that blocks cholesterol absorption. Lowers LDL by 15-20%. Safe, cheap, and works well with low-dose statins if you can tolerate even a little.
- Bempedoic acid: A newer oral drug that works like a statin but in the liver differently. Fewer muscle side effects. Approved for patients with statin intolerance.
Here’s the hard truth: PCSK9 inhibitors work better than any statin rechallenge for people who truly can’t tolerate them. But cost and access are barriers. That’s why rechallenge is still the first step-it’s cheaper, safer, and just as effective for most.
The SAMS-CI Tool: Know Your Risk Before You Restart
The Statin-Associated Muscle Symptom Clinical Index (SAMS-CI) is a 5-question tool doctors use to predict if your muscle pain is really from statins. It looks at:
- Timing of symptoms (did they start within 6 months of starting the statin?)
- Resolution after stopping
- Family history of muscle disease
- Use of interacting drugs (like fibrates or cyclosporine)
- CK levels
A score below 5 means you have a 91% chance of tolerating a rechallenge. A score above 7? You’re likely a true case of statin intolerance. This isn’t fluff-it’s validated in multiple studies. Yet, most doctors don’t use it.

Genetic Testing: The New Frontier
Some people have a gene variant called SLCO1B1 *5. This slows how your liver clears certain statins, like simvastatin. If you have two copies (*5/*5), your statin levels can be 222% higher than normal. That’s why you get muscle pain.
The European Atherosclerosis Society now recommends genetic testing for people with recurrent myopathy. It’s not routine yet, but if you’ve tried three statins and failed, it’s worth asking your doctor. The FDA already lists this gene in simvastatin’s label. It’s not science fiction-it’s in the manual.
Real Stories, Real Outcomes
One man in Ohio stopped simvastatin after muscle pain. His doctor said, “You’re intolerant.” He stayed off statins for two years. His LDL hit 190. He had a minor heart event. Then he found a lipid specialist. They switched him to pravastatin 20mg every other day. His LDL dropped to 75. No pain. He’s been on it for 18 months.
A woman in Texas tried every statin at lowest doses. Still had pain. She got tested for anti-HMGCR antibodies. Negative. Her doctor used the SAMS-CI-score was 3. They restarted her on fluvastatin 20mg daily with CoQ10. She’s been fine for a year.
But others? They tried everything. Three statins. Every-other-day. Low dose. Nothing worked. They went on evolocumab. Their LDL dropped. Their risk dropped. And they finally slept at night.
What You Should Do Next
If you stopped a statin because of muscle pain:
- Wait 2-4 weeks after symptoms disappear.
- Ask for a CK blood test and thyroid check (low thyroid can mimic statin myopathy).
- Ask your doctor: “Can we use the SAMS-CI to see if I’m a good candidate for rechallenge?”
- Request a switch to pravastatin, fluvastatin, or pitavastatin.
- Ask about every-other-day dosing.
- If it fails, ask about ezetimibe or bempedoic acid. If you’re high-risk, ask about PCSK9 inhibitors.
Don’t accept “you’re intolerant” as a final answer. That’s outdated thinking. With the right strategy, most people can get back on statins-and protect their heart.
Can statin muscle pain go away on its own?
Yes. In most cases, muscle symptoms from statins fade within 2-4 weeks after stopping the drug. That’s why guidelines recommend waiting this long before rechallenge-your body needs time to reset. If pain persists beyond 6 weeks, other causes like thyroid issues, vitamin D deficiency, or nerve compression should be checked.
Is it safe to take CoQ10 with statins?
Yes. CoQ10 is safe and often recommended for people with statin-related muscle pain. While studies show mixed results on whether it prevents pain, many patients report improvement. It doesn’t interfere with statin effectiveness. A typical dose is 100-200 mg daily.
Why do some doctors say not to restart statins after muscle pain?
Some doctors avoid rechallenge because they fear liability or don’t know the evidence. But major guidelines from the AHA, ACC, and NLA all support structured rechallenge. The real issue is lack of training-not risk. Patients are often mislabeled as “intolerant” when they just need a different statin or dose.
Can I take a statin if I have kidney disease?
Yes-but you need to be careful. Some statins, like pravastatin and fluvastatin, are safer in kidney disease because they’re not cleared through the kidneys. Avoid high-dose simvastatin and atorvastatin if your kidney function is low. Always check your eGFR and adjust the statin type and dose with your doctor.
Are PCSK9 inhibitors better than statins?
For lowering LDL, yes-they’re stronger. For preventing heart attacks, they’re proven in high-risk patients. But they’re not better for everyone. Statins are still first-line because they’re cheap, safe, and reduce risk across all risk levels. PCSK9 inhibitors are for those who can’t take statins or need extra LDL lowering. They’re not replacements-they’re upgrades when statins fail.
How long should I wait before trying a statin again after stopping?
Wait 2-4 weeks after all muscle symptoms have fully resolved. This gives your muscles time to recover and helps distinguish true statin intolerance from temporary side effects. Restarting too soon can lead to false conclusions and unnecessary avoidance of statins.
Final Thought: Your Heart Can’t Wait
Statin myopathy is real for some. But it’s overdiagnosed for many. You don’t have to live without statins. With the right approach-switching drugs, lowering doses, using every-other-day schedules, and checking for true causes-you can protect your heart without sacrificing your muscles. The data is clear. The tools exist. The question is: are you ready to ask for them?



Jasmine Yule
December 29, 2025 AT 12:43I was told I was statin-intolerant after one week of simvastatin and just accepted it. Turns out, I had a vitamin D deficiency and was just stressed. Restarted on pravastatin 10mg every other day with CoQ10-no pain, LDL down to 80. Why do doctors skip the basics?
Also, CoQ10 isn’t magic, but it helped me sleep better too. 🙌
Greg Quinn
December 30, 2025 AT 10:38It’s wild how much of medicine is still based on fear instead of data. The nocebo effect is real, but so is the fact that most docs don’t have time to explain it. I get why people quit-muscle pain sucks. But labeling someone ‘intolerant’ without a plan is just lazy.
Meanwhile, my uncle’s LDL hit 210 after quitting statins. He had a mini-stroke at 58. Now he’s on ezetimibe. Still alive. Still scared.
Lisa Dore
January 1, 2026 AT 03:46To anyone reading this and thinking ‘I can’t handle statins’-please don’t give up. I was in your shoes. Tried four statins, quit each time. Then I found a lipid specialist who used the SAMS-CI tool. Score was 4. We switched to pitavastatin 4mg every other day. No pain. No panic.
You’re not broken. The system is just outdated. Ask for the tool. Ask for the switch. You deserve to protect your heart without suffering.
Sharleen Luciano
January 1, 2026 AT 13:54How quaint. You’re all acting like this is some revolutionary insight. The MEDS protocol? Published in 2018. The SLCO1B1 gene? FDA-labeled since 2012. PCSK9 inhibitors? Available since 2015.
Yet here we are, in 2025, with primary care docs still treating statin myopathy like it’s witchcraft. The real tragedy isn’t the muscle pain-it’s the systemic ignorance. You’re not victims of biology. You’re victims of a broken healthcare pipeline.
And yes, I’ve seen three patients die because their GP said ‘just avoid statins’ and never followed up. This isn’t advice. It’s negligence dressed up as compassion.
Jim Rice
January 2, 2026 AT 02:25Wait-so you’re telling me the pain isn’t real? That’s what this whole thing boils down to? My legs felt like they were full of cement. I didn’t ‘imagine’ it. You think I wanted to be on a pill that made me limp around like a 90-year-old?
And now you want me to try again? With a different statin? Maybe a lower dose? Maybe on alternate days? Sounds like you’re just rearranging deck chairs on the Titanic.
My heart’s fine. My legs aren’t. Let me live with my LDL at 140 instead of being a walking zombie.
Henriette Barrows
January 3, 2026 AT 02:14I had the same thing. Thought I was done with statins forever. Then I found a doc who actually listened. She checked my thyroid, my vitamin D, even my magnesium. Turned out I was low on all three. Took supplements for 3 weeks, then tried fluvastatin 20mg daily. No pain. No drama.
Don’t give up. But also don’t rush. Give your body time. And ask for the SAMS-CI. Most docs haven’t heard of it, but it’s free and easy. Just say ‘I want to be properly assessed before giving up.’ You’ve got this 💪
Alex Ronald
January 3, 2026 AT 03:39For those considering rechallenge: the key isn’t just switching statins-it’s tracking your symptoms with a journal. Write down when the pain started, where it is, how bad (1-10), and what you were doing that day. I did this for 3 months before restarting. Turned out my pain was worse after long walks, not after taking the pill.
Turns out I had early hip osteoarthritis. The statin wasn’t the villain. I just blamed it because it was new.
Document everything. It changes everything.
Marie-Pierre Gonzalez
January 3, 2026 AT 04:28Thank you for this comprehensive and meticulously researched post. As a registered nurse in Ontario, I have witnessed firsthand the devastating consequences of premature statin discontinuation. The MEDS protocol is not merely a guideline-it is a lifeline. I consistently educate my patients on the nocebo effect and the pharmacokinetic differences between statins. Pravastatin, in particular, is underutilized due to misconceptions regarding potency. I am heartened to see this information being disseminated beyond specialist clinics. Please continue advocating for evidence-based practice. 🙏
Nicole K.
January 3, 2026 AT 08:32So you’re telling me people who feel pain from statins are just weak-minded? That’s rich. I’ve seen people die from heart attacks because they didn’t take statins. But I’ve also seen people who got worse on them. Who says you have to take them at all? Maybe your body’s telling you something.
And what about all the people who get diabetes from statins? You ignore that? You’re just pushing pills because Big Pharma pays your doctor.
I’m not restarting. I’m taking my chances. At least I’m not a lab rat.
Fabian Riewe
January 4, 2026 AT 00:44My mom tried every statin, got rhabdo once (CK over 10,000). She was terrified. But after 2 years off, her doctor used the SAMS-CI-score was 2. They restarted her on pitavastatin 2mg every third day. She’s been fine for 3 years now. LDL 72.
Don’t write yourself off. There’s almost always a way. Just don’t rush. And find a doc who actually knows what they’re doing. Not every GP is a lipid expert.
Amy Cannon
January 4, 2026 AT 08:01As someone who studied pharmacology in the UK and now works in public health here in the States, I find it deeply concerning that the gap between clinical evidence and frontline practice remains so vast. The MEDS framework is not merely a recommendation-it is a standard of care in lipid clinics across Europe and Canada. Yet in rural primary care settings, patients are routinely dismissed with the phrase ‘you’re intolerant’ without even a CK test. This is not just a knowledge gap-it is a systemic failure of clinical governance. We must prioritize continuing education for primary care providers and implement mandatory lipid literacy modules in residency programs. The cost of inaction is measured in preventable myocardial infarctions and strokes.
And yes, I did spell ‘myocardial’ correctly. No typos here.
Himanshu Singh
January 5, 2026 AT 02:54i read this whole thing and i was like wow. i had simvastatin and my legs hurt so bad i couldnt walk. i went off it. then i tried pravastatin 10mg every 2 day and it was fine. no pain. my ldl is 88 now. thank you for this. i was so scared to try again. you saved my life 😊
Teresa Rodriguez leon
January 6, 2026 AT 23:50You all are so naive. Statins cause muscle wasting, cognitive decline, and mitochondrial damage. You think a 10% reduction in heart attacks is worth losing your ability to climb stairs or remember your kid’s name? I’ve seen patients on PCSK9 inhibitors still get heart attacks. The whole system is built on fear and profit.
And now you want me to trust a blood test and a gene? You’re the ones being manipulated.
My heart is fine. My body knows better than your algorithms.
Louis Paré
January 8, 2026 AT 15:59Let’s be real: this entire post reads like a pharmaceutical white paper disguised as patient advocacy. The ‘60-80% success rate’? That’s from industry-funded trials. The ‘MEDS protocol’? A marketing rebrand of ‘try another pill.’
And let’s not forget-statins don’t prevent heart disease. They mask it. The real fix? Diet. Movement. Stress reduction. But those don’t come in a bottle with a patent.
So yes, go ahead and rechallenge. Keep swallowing your chemical crutches. Meanwhile, your gut microbiome is screaming.