When someone suddenly loses strength on one side of their body, slurs their words, or sees double - even if it lasts only a few minutes - most people think, ‘It’s nothing. It went away.’ But that’s exactly when you should call 911. What many call a ‘mini-stroke’ is actually a TIA - a Transient Ischemic Attack - and it’s not a warning. It’s a full-blown neurological emergency that’s already happened.
What Exactly Is a TIA?
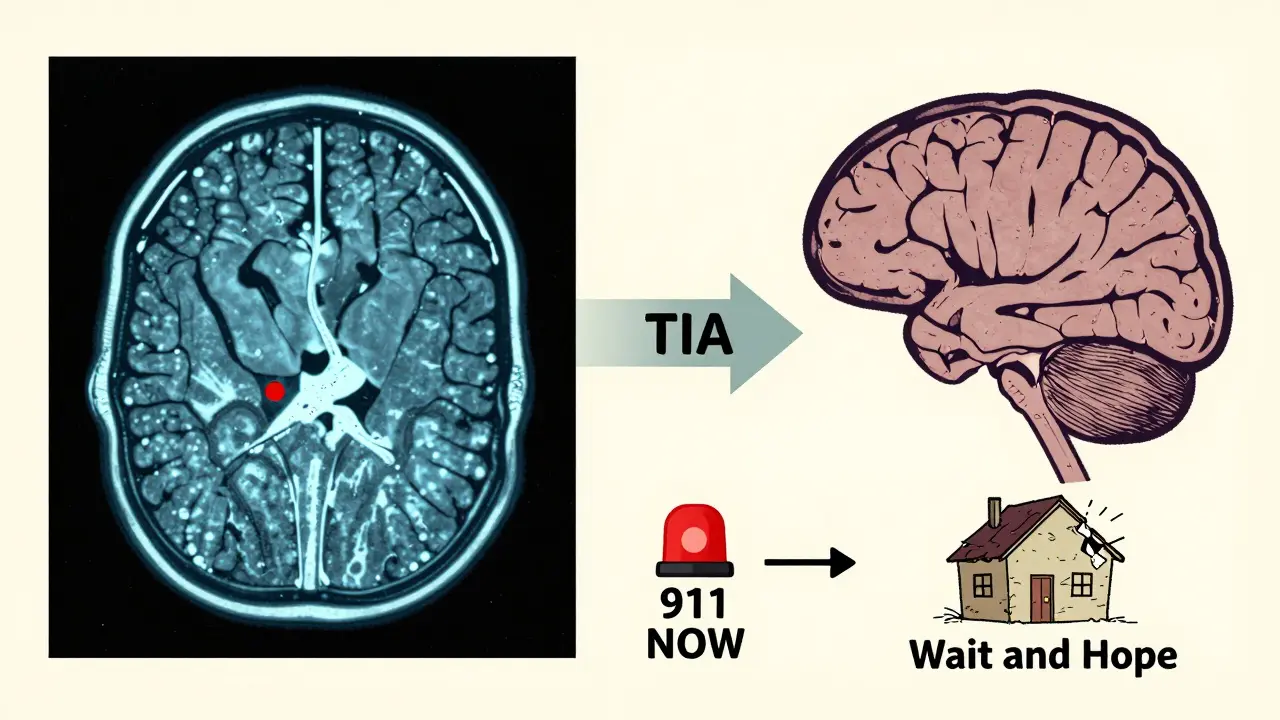
A TIA happens when blood flow to part of the brain is blocked, just like in a stroke. But unlike a stroke, the blockage clears quickly - usually within minutes - and no permanent brain damage shows up on an MRI. That’s why, for years, doctors defined a TIA by how long symptoms lasted: under 24 hours. But that definition is outdated. Since 2009, the American Heart Association and American Stroke Association have changed the rules. Now, a TIA is defined by what’s not there: no brain tissue death. If an MRI shows even a tiny spot of damaged brain cells, it’s not a TIA - it’s a minor stroke. And here’s the shocking part: about 35% of people who think they’ve had a TIA actually have that damage. That means nearly one in three ‘TIA’ cases are already strokes. The term ‘mini-stroke’ is dangerous. It makes people think it’s not serious. But a TIA is your brain screaming for help. One in five people who have a TIA will have a full stroke within 90 days. And the biggest risk? The first 48 hours. Up to 5% of people will have another stroke in just two days.How to Spot a TIA or Stroke - The BE FAST Rule
The symptoms of a TIA and an ischemic stroke are identical. The only difference? One fades. The other doesn’t. That’s why you don’t wait to see if it gets better. Use BE FAST:- Balance: Sudden dizziness, loss of coordination, or trouble walking
- Eyes: Blurred, double, or lost vision in one or both eyes
- Face: One side of the face droops when smiling
- Arm: One arm drifts down when raised
- Speech: Slurred, strange, or hard to understand speech
- Time: Call 911 now - even if symptoms disappear
Why Timing Is Everything
If you have a stroke, you might be eligible for clot-busting drugs like alteplase - but only if you get to the hospital within 4.5 hours. For a TIA, there’s no magic drug that reverses it. Instead, the goal is to stop the next stroke from happening. The key is speed. If you’re evaluated within 24 hours - ideally within 60 minutes - your risk of a stroke in the next 90 days drops by more than 80%. That’s not a guess. It’s from the EXPRESS study, published in The Lancet. Patients treated within 24 hours had a stroke risk of just 2.1%. Those who waited? 10.3%. Doctors use a tool called ABCD2 to quickly measure your risk:- Age: 60 or older = 1 point
- Blood pressure: 140/90 or higher = 1 point
- Clinical features: Weakness on one side = 2 points; speech trouble without weakness = 1 point
- Duration: Symptoms over 60 minutes = 2 points; 10-59 minutes = 1 point
- Diabetes: Present = 1 point
What Happens in the ER?
When you arrive at the emergency department with suspected TIA or stroke, they don’t waste time. First, they do a non-contrast CT scan to rule out bleeding in the brain. Then, within 24 hours, you’ll get an MRI with diffusion-weighted imaging. This is the gold standard. It can spot tiny areas of brain damage that a CT scan misses - and it’s why so many ‘TIA’ cases turn out to be strokes. If your MRI shows no damage, you’re diagnosed with a TIA. But even then, you’re not safe. You still need aggressive prevention. That means:- Aspirin and clopidogrel together for 21-30 days (dual antiplatelet therapy)
- High-intensity statin daily
- Blood pressure under 140/90
- Checking for atrial fibrillation (a heart rhythm problem that causes clots)
- Managing diabetes and cholesterol
The Big Misconception: ‘It Went Away, So I’m Fine’
The biggest problem isn’t medical. It’s cultural. People don’t take TIAs seriously because the symptoms vanish. The CDC found that 31% of TIA patients delay seeking care for more than 24 hours. Many think, ‘It was just a spell.’ Or, ‘I didn’t want to bother the doctor.’ That’s deadly. A TIA is not a warning sign. As Dr. Steven Levine from Northwell Health says, ‘TIA is not a warning - it’s an actual stroke event that resolved spontaneously.’ The brain was injured. The body just healed the blockage before permanent damage showed up on a scan. But the system that caused it - the clogged artery, the irregular heartbeat, the high blood pressure - is still there. And here’s something even more unsettling: new research from UC San Francisco in 2022 found that nearly half of patients diagnosed with TIA had subtle brain injuries visible only on advanced MRI scans. That means their ‘temporary’ attack actually caused permanent, undetected damage. They’re walking around with silent brain injury - and they’re at high risk for another, bigger stroke.Who’s at Risk?
TIA doesn’t pick favorites, but some groups are more vulnerable:- People over 60 - median age is 69
- Those with high blood pressure, diabetes, or high cholesterol
- Smokers and people with obesity
- People with atrial fibrillation
- Those with a family history of stroke

What Happens After the ER?
Leaving the hospital doesn’t mean you’re safe. You need a follow-up plan:- See a neurologist within 1 week
- Get a carotid ultrasound to check for artery narrowing
- Have a 24-hour heart monitor to catch silent AFib
- Start a daily aspirin or other antiplatelet drug
- Take a statin - even if your cholesterol is normal
- Control blood pressure - aim for under 130/80
What You Can Do Today
You don’t need to wait for symptoms to act. Here’s how to lower your risk right now:- Know your numbers: Blood pressure, cholesterol, blood sugar
- Walk 30 minutes a day - even if it’s just around the block
- Stop smoking - your stroke risk drops by half after one year
- Limit salt and processed foods - they raise blood pressure fast
- Don’t ignore ‘spells’ - dizziness, vision blur, or numbness that fades
Final Thought: A TIA Is a Second Chance
A TIA isn’t a punishment. It’s a gift - a brutal, scary, life-saving gift. It’s your body’s last chance to tell you something’s wrong before a stroke steals your speech, your movement, your independence. The good news? If you act fast, you can prevent almost all of them. The bad news? Most people don’t. They wait. They hope. They dismiss it. Don’t be one of them. If you’ve had a TIA - treat it like the emergency it is. And if you haven’t - start living like you might be one heartbeat away from one.Is a TIA the same as a stroke?
No. A TIA is a temporary blockage of blood flow to the brain that causes stroke-like symptoms but leaves no permanent brain damage on imaging. A stroke causes lasting brain injury due to prolonged lack of blood flow. But the symptoms are identical, and a TIA is often a hidden stroke - up to 35% of people diagnosed with TIA actually have brain damage seen on MRI.
Can a TIA go away on its own?
Yes, symptoms usually disappear within minutes to an hour. But that doesn’t mean the danger is gone. The same problem that caused the TIA is still in your body. Without treatment, you’re at high risk for a full stroke - especially in the next 48 hours. Never assume it’s over just because you feel fine.
Do I need to go to the hospital if my symptoms disappeared?
Absolutely. Even if symptoms are gone, you need emergency evaluation. Hospitals use imaging and risk scores like ABCD2 to find hidden damage and predict your next stroke risk. Delaying care increases your stroke risk by 5 times. Call 911 - don’t drive yourself.
What’s the best treatment after a TIA?
Immediate treatment includes aspirin (325 mg) and clopidogrel together for 21-30 days, a high-dose statin like atorvastatin 80 mg daily, and strict blood pressure control under 140/90. You’ll also need tests for heart rhythm problems and artery blockages. Following this protocol reduces your 90-day stroke risk from over 10% to under 2%.
Can I prevent another stroke after a TIA?
Yes - if you act fast and stick to your plan. Studies show that getting treatment within 24 hours cuts your stroke risk by 80%. Long-term, controlling blood pressure, quitting smoking, taking your meds, and exercising regularly can reduce your risk by more than 90%. A TIA isn’t the end - it’s your chance to change your future.




rachel bellet
January 17, 2026 AT 01:19The term 'mini-stroke' is not just misleading-it’s a catastrophic misnomer that undermines public health literacy. A TIA is a neurovascular event with the same pathophysiology as a stroke; the only distinction is the absence of infarction on DWI-MRI. But even 'silent' microinfarcts-detectable only with high-field MRI-can accumulate and lead to vascular cognitive impairment. The CDC’s 31% delay statistic isn’t just alarming-it’s a systemic failure of medical communication. We need mandatory public education campaigns, not just pamphlets in ER waiting rooms.
And let’s not pretend aspirin is a panacea. Dual antiplatelet therapy is only indicated for 21-30 days post-TIA per AHA/ASA guidelines. Long-term monotherapy? That’s where adherence drops off a cliff. Patients think they’re 'fixed' after the ER. They’re not. They’re walking time bombs with uncontrolled hypertension, undiagnosed AFib, and a 20% one-year stroke risk if they stop statins.
Also, why are we still using ABCD2? It has a C-statistic of 0.68. We’ve had AI models with 92% predictive accuracy for 7-day stroke risk since 2021. If your hospital isn’t deploying AI triage tools, you’re practicing 2015 medicine in 2024.
And yes-'mini-stroke' should be banned from all clinical and public discourse. It’s medical malpractice by euphemism.
Jay Clarke
January 18, 2026 AT 14:09Bro. I had a TIA and I didn’t even go to the hospital. Just sat there for 20 minutes thinking, 'Man, my coffee must’ve been bad.' Then I felt fine. Guess what? I’m still here. And I’m 47. So yeah, maybe you’re right, maybe I’m dumb, but I’m alive. You wanna live in fear of every little dizzy spell? Go ahead. I’ll be over here, eating tacos and not letting Big Medicine scare me into a lifetime of pills.
Also, why is everyone so obsessed with MRIs? My grandma had a stroke and they didn’t even do a scan for three days. She’s fine now. Maybe the system’s broken, not me.
Selina Warren
January 19, 2026 AT 23:54Listen. I used to be the person who thought 'it’ll pass.' I ignored the numbness in my arm for three hours because I was 'too busy.' Then I had a full stroke at 52. Lost half my speech. Can’t hold a coffee cup without shaking. I’m 58 now. I walk with a cane. I cry when I can’t say my daughter’s name right.
A TIA is not a glitch. It’s your brain screaming, 'I’m dying, and you’re ignoring me.'
You don’t get a second chance to fix this. Not like a broken phone. Not like a missed deadline. Your brain doesn’t have a 'restore point.'
If you’re reading this and you’ve ever had a 'spell'-call 911. Now. Not tomorrow. Not after lunch. NOW. I’m not asking. I’m begging. Because I wish someone had begged me.
Nishant Sonuley
January 21, 2026 AT 09:22Interesting perspective, but let’s not forget the global context here. In the U.S., you have access to MRI machines, neurologists, and AI triage tools. In rural India, where I’m from, a person with TIA symptoms might wait 48 hours just to see a general practitioner who’s never heard of ABCD2. The real tragedy isn’t just patient denial-it’s systemic inequity. We need to stop treating this as an individual failure and recognize it as a public health infrastructure crisis.
Also, the statin recommendation-atorvastatin 80 mg-is not universally applicable. In South Asia, we see higher rates of statin-induced myopathy. Guidelines from the Indian Stroke Association recommend lower doses and closer monitoring. One-size-fits-all medicine is dangerous, even when it’s well-intentioned.
And yes, 'mini-stroke' is a terrible term. But changing terminology won’t fix what’s broken: lack of access, lack of awareness, lack of resources. Let’s fix those first.
Still, props to the original post. It’s one of the clearest explanations I’ve seen in English. Even if I’m from a different world, I learned something.
Emma #########
January 21, 2026 AT 14:28I just lost my dad to a stroke last year. He had a TIA two months before but didn’t go in because he said he 'felt fine.' He didn’t want to be a burden. I wish I’d known then what I know now. I would’ve driven him myself. I would’ve screamed if I had to.
This post saved me from making the same mistake with my mom. I printed it out and taped it to the fridge. She doesn’t read much, but she sees it every day.
Thank you for writing this. Not everyone gets a second chance. But we can still make sure others do.
Andrew McLarren
January 22, 2026 AT 18:41While the clinical content presented is largely accurate and aligned with current AHA/ASA guidelines, one must exercise caution regarding the assertion that 'a TIA is not a warning-it is an actual stroke event.' This terminology, while neuroanatomically defensible, risks conflating clinical syndromes with radiological outcomes, potentially undermining the utility of the TIA construct as a distinct prognostic category. The absence of infarction on diffusion-weighted imaging remains a clinically meaningful distinction, even if the underlying pathophysiology is identical. Furthermore, the implication that all patients with TIA require dual antiplatelet therapy may not be generalizable to those with non-atherosclerotic etiologies, such as cardiac embolism or vasculitis. A nuanced, etiology-driven approach remains paramount.
That said, the emphasis on early neuroimaging and risk stratification is unequivocally supported by the literature, particularly the EXPRESS trial. The integration of AI-driven risk prediction tools into emergency workflows represents a paradigm shift worthy of broader adoption.
Andrew Short
January 23, 2026 AT 12:05Let’s be real. The whole 'TIA is a stroke' narrative is just Big Pharma’s way of selling more statins and aspirin. You think they care about your brain? They care about your prescription refill rate. They invented 'mini-stroke' to scare people into buying drugs. And now they’re redefining TIA to make it sound scarier so you’ll get an MRI, which costs $2,000, and then they’ll find 'tiny lesions' you didn’t even know about and scare you into lifelong medication.
My uncle had a 'TIA' and they put him on five drugs. He’s 70. He’s now got kidney issues, muscle pain, and can’t sleep. He’s worse off than before.
Maybe the real problem isn’t the TIA-it’s the medical industrial complex that turns every little blip into a crisis.
christian Espinola
January 24, 2026 AT 10:08Correction: The original post incorrectly states that '56% of TIAs resolve within 10 to 60 minutes.' According to the 2018 AHA/ASA scientific statement, the median duration is 10 minutes, with 80% resolving within 30 minutes. The 56% figure appears to be a misinterpretation of data from the Oxford Vascular Study, which reported that 56% of TIAs resolved within 1 hour-but that’s not the same as 'within 10 to 60 minutes.'
Also, the claim that 'nearly half of patients diagnosed with TIA had subtle brain injuries' is misleading. The 2022 UCSF study found that 48% of patients with clinically diagnosed TIA had DWI-positive lesions-but this cohort was selected from a tertiary care center with high-resolution MRI protocols. The true prevalence in community settings is closer to 25-30%.
And while the ABCD2 score is imperfect, it remains widely used because it’s validated in diverse populations. Dismissing it as 'outdated' without offering a superior, accessible alternative is irresponsible.
Grammar note: 'MRI with diffusion-weighted imaging' is redundant. DWI is a sequence on MRI. You don’t say 'CT with non-contrast.' You say 'non-contrast CT.'
Point is: precision matters. Misinformation-even well-intentioned-costs lives.
Chuck Dickson
January 25, 2026 AT 18:02Hey everyone-I’m not a doctor. I’m just a guy who used to ignore his blood pressure. I had a TIA last year. Thought it was stress. Turns out my BP was 190/110. I didn’t even know what that meant.
After I got out of the hospital, I started walking every day. Cut out soda. Got my cholesterol checked. Took my meds. I’m not ‘fixed.’ But I’m alive. And I’m not scared anymore.
If you’re reading this and you’re thinking, 'I’m too young for this'-you’re wrong. If you’re thinking, 'I don’t have time'-you’re wrong. If you’re thinking, 'It’ll go away'-you’re playing Russian roulette with your brain.
I’m not here to scare you. I’m here to say: you’ve got time. Right now. Use it. Don’t wait for the next spell. Don’t wait for the next hospital visit. Start today. Walk. Check your numbers. Call your doctor. Your future self will thank you.
And if you see someone with BE FAST symptoms? Call 911. Even if they laugh. Even if they say no. Do it anyway. You might just save someone’s life.