
When Tuberculosis a bacterial infection caused by Mycobacterium tuberculosis that primarily attacks the lungs meets the habit of smoking inhalation of tobacco smoke containing nicotine and thousands of chemicals, the result is more than just a bad cough. The two act together to cripple the immune system, damage lung tissue faster, and raise the odds of severe disease or death. If you’re reading this because you or a loved one have TB, or you’re a smoker wondering about the risks, you’ve come to the right place.
TL;DR
- Smoking doubles the chance of developing active TB after infection.
- It weakens the immune response and worsens lung damage, making treatment harder.
- Quitting smoking improves TB treatment success by up to 30%.
- Standard TB therapy (e.g., isoniazid) works best when the lungs are smoke‑free.
- Seek support: doctors, quit lines, and community programs can help you break the habit.
How Smoking Increases TB Risk
Scientists have measured the link for years. A 2023 meta‑analysis of 18 cohort studies found that current smokers are about 2.1 times more likely to progress from latent TB infection to active disease than non‑smokers. The reason isn’t just “bad lungs.” Tobacco smoke contains carbon monoxide, reactive oxygen species, and nicotine, all of which interfere with immune system the body’s defense network of macrophages, T‑cells, and cytokines functions.
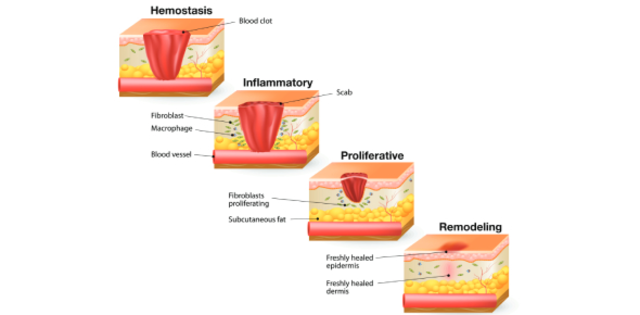
When you breathe in smoke, the tiny particles settle in the airways and trigger chronic inflammation. Lung tissue the delicate alveoli and bronchi that exchange oxygen and carbon dioxide becomes scarred, reducing its ability to clear bacteria. Mycobacterium tuberculosis, which normally gets trapped and killed by activated macrophages, finds a weakened battlefield and can multiply unchecked.
Impact on TB Treatment Outcomes
Even after diagnosis, smoking continues to sabotage therapy. The standard regimen-six months of isoniazid, rifampicin, ethambutol, and pyrazinamide-relies on patients adhering to daily doses and on lungs being able to absorb the drugs effectively. Studies from Australia, India, and South Africa show that smokers have a 15‑30% higher rate of treatment failure or relapse.
Two mechanisms drive this:
- Pharmacokinetic interference: Nicotine induces liver enzymes that can speed up drug metabolism, lowering the concentration of antibiotics in the bloodstream.
- Behavioral non‑adherence: Smokers are statistically more likely to miss doses, often because the side‑effects of medication (nausea, fatigue) feel worse when combined with nicotine withdrawal.
In short, the smoke‑filled lungs become a hostile environment for both the bacteria and the medicines trying to kill it.
Why Quitting Makes a Difference
Good news: the moment a smoker stops, the body begins to repair. Within weeks, cilia-the tiny hair‑like structures that sweep mucus out of the airways-start to regrow. After three months, lung capacity improves by about 10%, and immune markers such as interferon‑γ increase, making it easier for the body to control TB bacteria.
Clinical trials in 2022 demonstrated that TB patients who quit smoking during treatment had a 28% higher cure rate compared to those who kept smoking. Moreover, quitting reduces the risk of developing drug‑resistant TB, a growing global concern.

Practical Steps to Quit Smoking While on TB Therapy
Quitting is tough, especially when you’re already dealing with a heavy medication schedule. Here’s a realistic roadmap:
- Talk to your doctor: Ask for a full assessment of nicotine dependence. Many TB clinics can prescribe nicotine replacement therapy (NRT) or short‑term bupropion that won’t clash with anti‑TB drugs.
- Set a quit date: Choose a day within the first two weeks of starting TB treatment. The overlap of two health goals creates momentum.
- Use NRT wisely: Patches provide steady nicotine, while gums help manage cravings. Replace each cigarette with a patch dose that equals your usual intake.
- Lean on support networks: Australian Quitline (137848) offers free counseling, text reminders, and peer groups. If you live in Perth, the local community health centre runs weekly “Smoke‑Free TB” workshops.
- Track progress: Keep a simple log of daily medication intake and smoke‑free days. Seeing the numbers rise is a powerful motivator.
Remember, slipping is normal. If you have a lapse, restart right away-don’t wait for a “perfect” moment.
Comparison: TB Outcomes in Smokers vs. Non‑Smokers
| Metric | Smokers | Non‑Smokers |
|---|---|---|
| Progression from latent to active TB | 2.1× higher risk | Baseline |
| Treatment success rate | 73% | 88% |
| Relapse within 12months | 15% | 5% |
| Development of drug‑resistant TB | 9% | 3% |
| Average time to sputum conversion | 9weeks | 6weeks |
The numbers paint a clear picture: smoking not only raises the odds of getting sick, it also makes recovery slower and more complicated.
Public Health Perspective
From a community angle, the combination of TB and smoking fuels a vicious cycle. In crowded urban settings-like parts of Perth’s northern suburbs-smokers often share indoor spaces, spreading infectious droplets. The World Health Organization estimates that tobacco use accounts for about 15% of all TB deaths worldwide.
Policies that integrate smoking cessation into TB programs have shown success. For example, a 2021 pilot in Queensland linked every newly diagnosed TB patient with a cessation counselor. After two years, the region saw a 22% drop in TB‑related mortality.
Bottom Line: Take Action Today
If you’re battling TB, the smartest move you can make is to quit smoking now. It boosts your body’s natural defenses, improves drug effectiveness, and cuts future health risks. Talk to your healthcare provider, grab a nicotine patch, and lean on community resources. The path isn’t easy, but the payoff-healthier lungs, a higher chance of cure, and a brighter future-is worth every effort.

Frequently Asked Questions
Does secondhand smoke increase TB risk?
Yes. Even if you don’t smoke, prolonged exposure to tobacco smoke can impair lung immunity and raise the chance of latent TB turning active.
Can nicotine replacement therapy interact with TB meds?
Most NRT products (patches, gum, lozenges) are safe and don’t affect the metabolism of isoniazid or rifampicin. Always confirm with your doctor before starting any new medication.
How long does it take for lung function to improve after quitting?
Significant gains appear within 2‑3months, with cilia regrowth and reduced inflammation. Full recovery can take up to a year, depending on previous smoking intensity.
Is there a higher risk of drug‑resistant TB for smokers?
Studies show smokers are about three times more likely to develop multidrug‑resistant TB, mainly due to poor treatment adherence and altered drug metabolism.
What community resources are available in Perth?
Perth’s Western Australian Health Department runs free TB clinics that include smoking‑cessation counseling. The Statewide Quitline (137848) offers 24/7 phone support, and several local NGOs host weekly support groups.


shivam mishra
September 30, 2025 AT 06:04Just had a patient in Delhi quit smoking during TB treatment last month. His sputum cleared in 5 weeks-normally takes 8-9 for smokers. The nicotine patch helped him sleep better too. Docs here are starting to push this hard now. If you’re smoking and have TB, just stop. Your lungs don’t need the extra drama.
Scott Dill
October 1, 2025 AT 23:51Bro. I smoked for 12 years. Got TB last year. Quit on day 3 of meds. Didn’t use patches. Just told myself ‘I’m not dying for a habit.’ Now I’m 8 months clean, no relapse. My cough’s gone. I can climb stairs without wheezing. This isn’t just advice-it’s survival.
Arrieta Larsen
October 3, 2025 AT 00:29My mom had TB in ’19. She smoked 2 packs a day. Took her 11 months to clear it. Relapsed once. After she quit, she got a lung scan last year-still some scarring, but no active infection. I wish someone had told us how much quitting mattered. Not just for her, but for everyone around her.
Mike Gordon
October 3, 2025 AT 15:05So like, the science is solid right? Smoking messes with macrophages and drug metabolism and cilia and blah blah. But honestly? Most people don’t care about macrophages. They care about ‘does this make me feel better now?’ And quitting? Feels like losing a friend. That’s the real barrier. Not the science. The emotion.
Kathy Pilkinton
October 4, 2025 AT 04:12Wow. So smokers are basically volunteering to be TB’s personal buffet. And then they wonder why treatment fails? No one’s forcing you to smoke. No one’s forcing you to ignore your own lungs. You think the WHO cares? They’re just documenting how dumb humans can be. Congrats on being statistically predictable.
Holly Dorger
October 5, 2025 AT 17:01Just wanted to say if you’re reading this and you’re scared to quit because you think you’ll fail… you won’t. Not because it’s easy. But because you’re worth the effort. I’m not a doctor. I’m just someone who watched my cousin go through this. He quit. He’s alive. That’s all that matters.
Amanda Nicolson
October 6, 2025 AT 13:57Okay imagine your lungs are a garden. Smoking is like dumping acid on the soil, setting fire to the plants, and then yelling at the flowers for not blooming. TB is the fungus that shows up because the garden’s already dying. Now imagine someone says, ‘Hey, stop pouring acid.’ And you say, ‘But I’ve been pouring acid for 20 years!’ Yeah, but the acid isn’t the problem? The acid is the whole damn problem. You don’t need to be a scientist to get that. Just stop. Please.
Jackson Olsen
October 8, 2025 AT 01:22My uncle smoked. Got TB. Quit. Cured. Now he bikes 10 miles every morning. No joke. I used to think quitting was for weak people. Now I know it’s for smart ones. Just stop. It’s not magic. It’s just not poison anymore.
Penny Clark
October 9, 2025 AT 23:40i had tb last year and i was smoking 15 cigs a day. i quit on day 5. i used gum. it was hell. but i did it. now my lungs dont hurt when i laugh. i know its hard. but you can. i believe in you. 💪❤️
Niki Tiki
October 11, 2025 AT 17:55Why are we even talking about this? People smoke because they want to. TB is just nature’s way of filtering out the weak. If you can’t quit smoking, you probably shouldn’t be breathing anyway. Stop whining and let evolution do its job.
Jim Allen
October 12, 2025 AT 02:46What if smoking is just a symptom? Like… what if people smoke because they’re lonely? Or traumatized? Or just tired of being told what to do? TB is the consequence. But the real disease is the system that makes people feel like they need smoke to feel human. We’re treating the cough, not the despair.
Nate Girard
October 13, 2025 AT 17:59My sister’s a nurse in Chicago. She says the biggest change she’s seen in the last 3 years? Smokers who quit during TB treatment are way more likely to show up for follow-ups. They’re more hopeful. It’s not just the medicine. It’s the mindset. Quitting gives you back control. And that’s half the battle.
Carolyn Kiger
October 15, 2025 AT 10:00My grandma smoked for 50 years. Never got TB. But she died of COPD at 78. I used to think, ‘See? Smoking doesn’t always kill you.’ But now I know-TB was just waiting. And if she’d quit even at 60, she might’ve had 15 more years. Don’t wait for the diagnosis to start caring.
krishna raut
October 17, 2025 AT 00:24Smoking doubles TB risk. Quitting improves cure rate by 30%. Simple math. Do the right thing.
Prakash pawar
October 17, 2025 AT 16:03They say smoking causes TB but what about the government? They sell cigarettes and then charge you for treatment. They make money off your sickness. So who’s really guilty? The smoker? Or the system that feeds the addiction and then sells you the cure?
MOLLY SURNO
October 18, 2025 AT 21:48Thank you for this well-researched and compassionate post. The inclusion of clinical data alongside practical steps is invaluable. I will be sharing this with my patients at the community clinic. The public health implications are profound and deserve wider dissemination.
Alex Hundert
October 19, 2025 AT 07:47That table with the stats? That’s the wake-up call. 73% success rate for smokers vs 88% for non-smokers? That’s not a small difference. That’s a death sentence for 1 in 4 people. If you’re still smoking and have TB, you’re not just hurting yourself-you’re gambling with your life. And that’s not brave. It’s reckless.
Emily Kidd
October 20, 2025 AT 21:00just read this and my heart broke. my bro got tb last year. he smoked. he missed doses. he relapsed. he’s doing better now but i wish i’d known this sooner. please if you’re reading this and you smoke… please stop. for them. for you. for the people who love you.
Justin Cheah
October 21, 2025 AT 22:54Let’s be real. This whole thing is a distraction. Big Pharma and the WHO want you to think quitting smoking will fix everything. But what about the air pollution? The mold in your apartment? The fact that TB is spread by overcrowded housing and poverty? They don’t want you to talk about that. They want you to blame yourself. Quit smoking? Sure. But don’t forget who profits from your guilt.