
When a batch of medicine is released, it’s not just a number on a log. It’s someone’s life. That’s why quality assurance units can’t report to the production manager. They can’t be part of the team trying to hit monthly output targets. They can’t be budgeted under the same department that’s rushing to ship product. If they are, the system breaks - and people get hurt.
What Exactly Is a Quality Assurance Unit?
A quality assurance unit (QU) is not just another department that checks boxes. It’s a legally mandated, independent watchdog with one job: protect product quality at all costs. In pharmaceuticals, nuclear plants, and other high-risk manufacturing environments, this isn’t optional. It’s written into law. The U.S. FDA requires it. The European Medicines Agency demands it. The International Atomic Energy Agency enforces it. The QU doesn’t make the product. It doesn’t run the machines. It doesn’t schedule shifts. Its only authority is to say no. To reject a batch. To halt production. To demand an investigation - even if it delays shipping. That’s the whole point. Independence isn’t a nice-to-have. It’s the only thing that keeps quality from being sacrificed for speed.Why Independence Isn’t Just a Best Practice - It’s the Law
In 2006, the FDA made it crystal clear: quality and production must be separated. That guidance didn’t come out of nowhere. It was built on decades of failures. The 1979 Three Mile Island nuclear incident showed what happens when safety checks are buried under operational pressure. In pharmaceuticals, the same pattern repeated: batches released without proper testing, data altered to meet targets, investigations buried. Today, 21 CFR 211.22 is the rule: the quality control unit must have the authority to approve or reject every component, container, label, and finished product. No exceptions. No compromises. The FDA’s own data shows that when quality units report to production leaders, critical failures jump by 37%. That’s not a coincidence. It’s cause and effect. In 2024, 68% of FDA warning letters cited failures in QU independence. That’s up from 29% in 2020. Companies are still trying to cut corners. Some try to make the production manager also the QA manager. Others let warehouse staff call quality directly to rush approvals. These aren’t minor slips. They’re violations that trigger regulatory action - and sometimes recalls.How Independence Actually Works in Practice
A truly independent QU doesn’t just sit in a separate office. It has:- Direct reporting lines to the CEO or Board of Directors
- A separate budget - not controlled by production
- The legal right to stop production without approval from anyone in manufacturing
- Access to all records, systems, and personnel without permission
- Staff trained in GMP, statistical process control, and conflict resolution

What Happens When Independence Is Compromised
It doesn’t take long for things to go wrong. On Reddit, a quality professional shared how their company merged QA and production roles during restructuring. Within three months, two critical deviations slipped through - both were released without full investigation. One batch contained a contaminant. The company had to recall 12,000 units. The FDA issued a warning letter. The CEO resigned. Another case: a small pharma facility with only 40 employees. The QU had three people. One was also managing inventory. Another was helping schedule production. The third was overwhelmed. In 2023, the FDA found 14 batch records with missing data. All were approved by the same person who also oversaw production. The facility lost its license. The numbers don’t lie. Facilities with fewer than 50 employees are 2.3 times more likely to fail QU independence audits. Why? Because they try to do too much with too little. But cutting corners on quality doesn’t save money - it costs more in recalls, fines, and lost trust.How Large Companies Get It Right
Big companies don’t just have bigger budgets - they have better systems. Eli Lilly implemented a “quality ambassador” program. Manufacturing staff took training from the QU, attended meetings, and learned how to spot risks early. But the QU still reported directly to the Chief Quality Officer. No overlap. No dual roles. Result? A 40% improvement in quality culture and zero critical deviations linked to communication gaps. Merck spent nine months restructuring its QU after years of resistance from production teams. They created formal conflict resolution protocols. They gave QU leaders direct access to the CEO. They published the QU’s authority in every employee handbook. Today, Merck has one of the highest first-time inspection success rates in the industry. The common thread? They didn’t just change the org chart. They changed the culture.The Real Cost of Ignoring QU Independence
Some argue that separating quality from production slows things down. MIT’s Dr. Alan Chen points to a 2023 case where integrated teams resolved deviations 22% faster. But here’s the catch: those same teams had 17% more borderline compliance decisions - meaning they let things slide that should have been rejected. The FDA’s data shows that when QU independence fails, 63% of warning letters involve data integrity violations. That’s not about slow processes. That’s about lying to regulators. That’s about fraud. And it’s expensive. A single recall can cost $10 million to $50 million. A warning letter can tank stock prices. A revoked license can kill a business. The cost of independence? A few extra staff. A separate budget. A clear reporting line. That’s nothing compared to the cost of failure.
What Small Businesses Can Do
Not every company can hire a 10-person QU. But every company can ensure independence. Many small manufacturers now use third-party quality oversight services. These are independent firms that audit your processes, review batch records, and provide an objective second opinion. It’s not perfect - but it’s better than having your production manager approve his own work. The key is documentation. If you don’t have a formal QU, you still need a written policy that says: “Quality decisions are made independently of production pressure.” And you need to follow it. FDA data shows 95% of warning letters cite inadequate documentation of QU authority. That’s not about the size of your team. It’s about clarity. If your policy says “quality has final say,” then make sure it’s true.The Future: Digital Manufacturing and AI
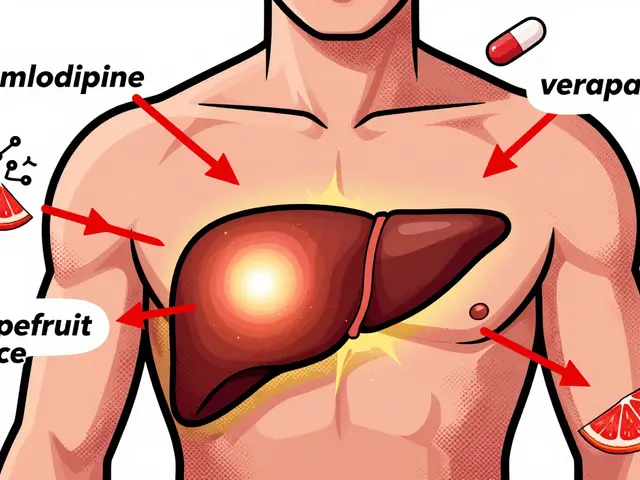
Now, new challenges are emerging. AI-driven production systems make real-time quality decisions. Algorithms decide whether a batch passes or fails. Who oversees the algorithm? The FDA’s 2025 draft guidance says: even in digital manufacturing, independence must be maintained. The algorithm can’t be owned by the production team. Someone outside production must validate its logic, monitor its performance, and have the authority to shut it down. The future isn’t about human vs. machine. It’s about who controls the control system. If the machine is programmed by production, it will optimize for speed. If it’s governed by an independent QU, it will optimize for safety.Final Thought: Quality Isn’t a Department - It’s a Culture
A quality assurance unit isn’t a team that checks paperwork. It’s the last line of defense. It’s the voice that says, “This isn’t safe.” And if that voice is silenced - even quietly, even unintentionally - the whole system becomes a lie. The data is clear. The regulations are clear. The consequences are clear. If you’re in manufacturing - especially in pharma or high-risk industries - independence isn’t a policy. It’s a promise. To patients. To customers. To the law. Don’t just have a quality unit. Make sure it’s truly independent. Because if it’s not, you’re not just risking compliance. You’re risking lives.Can a quality assurance unit report to the production manager?
No. Regulatory agencies like the FDA and EMA require that quality assurance units operate independently of production. If a QU reports to production leadership, it creates a conflict of interest where efficiency goals can override safety standards. This is a direct violation of 21 CFR 211.22 and triggers FDA warning letters.
What authority does a quality assurance unit have?
A compliant QU has the legal authority to approve or reject all components, packaging, in-process materials, and finished products. It can halt production, require investigations, and refuse to release batches - even if doing so delays shipments or impacts revenue. This authority must be documented and enforced without interference from manufacturing.
How many people should be in a quality assurance unit?
Industry benchmarks suggest 8-12% of total manufacturing staff should be in the QU. For example, a facility with 200 employees should have 16-24 quality staff. Smaller companies may use third-party oversight, but they must still maintain independence and documented authority.
What happens if a quality unit fails an audit?
Failure to meet independence standards leads to FDA warning letters, import alerts, or even suspension of manufacturing licenses. In severe cases, companies face mandatory recalls, fines, or criminal charges for data integrity violations. Over 68% of 2024 FDA warning letters cited QU independence failures.
Is QU independence required in all industries?
It’s legally required in pharmaceuticals, medical devices, and nuclear energy. ISO 9001-certified manufacturers may not require it by law, but industry experts agree that independence reduces risk and improves product safety - even in non-regulated sectors.
Can AI replace the need for an independent quality unit?
No. AI can automate quality checks, but it cannot replace independent oversight. Algorithms must be validated and monitored by personnel outside production. The FDA’s 2025 draft guidance explicitly states that AI-driven decisions must still be governed by an independent quality authority to prevent bias toward speed over safety.


Michelle Edwards
December 9, 2025 AT 01:48Just wanted to say this post nailed it. I work in a small pharma lab, and we don’t have a big team-but we made sure QA reports straight to the COO. No compromises. Last year, we caught a contamination in a batch before it left the facility. No one thanked us. But we sleep fine at night.
Quality isn’t sexy. But it’s sacred.
Sarah Clifford
December 10, 2025 AT 06:46lol so you’re saying if my cousin’s vape shop has a guy who checks if the juice isn’t just food coloring and battery acid, he can’t also be the guy who stocks the shelves? 😂
Rebecca Dong
December 11, 2025 AT 21:22Oh here we go again. The ‘independent QA’ cult. You know what actually keeps people safe? Accountability. Not some bureaucrat with a badge who says ‘no’ because they’re scared of getting fired. Real companies don’t need 10 layers of red tape-they need people who care enough to fix things, not just block them.
And let’s be real-most of these ‘violations’ are just regulators flexing because they don’t understand modern manufacturing. AI doesn’t need a human to say ‘stop.’ It just needs good code.
Also, who’s paying for all these extra QA staff? You? Me? The patient? We’re all paying for this nonsense.
Regan Mears
December 12, 2025 AT 15:45I get where Rebecca’s coming from-but you’re missing the point. It’s not about fear. It’s about structure. When QA reports to production, you’re asking someone to choose between their job and their ethics. That’s not leadership-that’s coercion.
I’ve seen it. A guy I worked with got pressured to sign off on a batch with a 12% variance. He said no. They moved him to nights. Six months later, he quit. The batch went out. Two patients had reactions. It wasn’t his fault. But he carried it.
Independence isn’t about power. It’s about protecting the people who do the right thing.
And yes, AI can help. But AI doesn’t have a conscience. Someone has to teach it what ‘right’ looks like-and that someone can’t be the same person getting bonuses for output.
Neelam Kumari
December 12, 2025 AT 19:06Wow. So you’re telling me that in a $200 million pharma company, they can’t afford to have one person who’s not also doing production? How about you hire one less manager and one more QA? Oh wait-you’d rather pay $40 million in recalls than $100k in salaries. Classic.
Ben Greening
December 13, 2025 AT 23:35The data is overwhelming. The FDA’s own figures show that facilities with independent QA units have 58% fewer critical deviations. This isn’t theory. It’s statistical fact. The only people arguing against it are either benefiting from the current system-or haven’t seen what happens when it fails.
Read the warning letters. Look at the recalls. The pattern is identical: someone in production overruled QA. Someone got scared. Someone signed off.
It’s not about bureaucracy. It’s about not killing people.
Nikki Smellie
December 15, 2025 AT 20:41EVERYTHING IS A LIE. 🤫 The FDA doesn’t care about patients. They’re owned by Big Pharma. The whole “independent QA” thing? A distraction. They want you to think you’re safe while they quietly approve 80% of the same labs every year. The real danger? The algorithms that control the QA systems are written by the same people who design the production lines. They’re all connected. You think you’re protected? You’re being monitored.
And yes-I’ve seen the internal emails. The ones they don’t publish.
They’re watching. They’re always watching. 😈
Stephanie Maillet
December 16, 2025 AT 17:11There’s a deeper layer here, isn’t there? We talk about independence like it’s a structural fix-but what we’re really talking about is trust. Can we trust the people who make the product to also judge its safety? Can we trust the system to value life over profit? The QA unit isn’t a department-it’s a moral compass. And when we try to bend it to fit corporate goals, we’re not just risking compliance-we’re eroding the very idea that human life matters more than quarterly earnings.
Maybe the real question isn’t ‘how do we organize QA?’
It’s: ‘what kind of society do we want to be?’
David Palmer
December 17, 2025 AT 10:44Yeah but what if the QA guy is just a jerk? What if he’s the one holding things up because he’s mad his coffee machine broke? You can’t just hand someone the power to shut down a whole plant because they’re having a bad day.
Maybe we need a QA guy who’s also part of the team. Like, you know… human?
Queenie Chan
December 17, 2025 AT 15:30Let’s get real for a sec. The whole ‘independent QA’ thing? It’s beautiful in theory. But in practice? It’s a power play dressed up as ethics. The QA team becomes its own silo-full of people who’ve never touched a machine, never seen a production line, never understood why a batch was rushed.
And then they say ‘no’… for no good reason.
I’ve seen QA reject a batch because the label font was 0.2mm too small. The medicine was fine. The patient was fine. But the ‘process’ was violated.
So now we’re punishing people for perfectionism? That’s not safety. That’s bureaucracy with a halo.
What we need isn’t independence. It’s collaboration. QA and production working together-not in separate castles.
And yeah-I’ve worked on both sides. I know what I’m talking about.
Doris Lee
December 19, 2025 AT 04:29My dad worked in a small insulin plant in the 80s. They didn’t have a fancy QA team. Just one woman who showed up every morning with coffee and a clipboard. She didn’t report to anyone. She just asked, ‘Is this safe?’
And if the answer wasn’t yes-she didn’t sign it.
She didn’t need a title. She just needed courage.
Maybe that’s what we’re really missing.