
Most women don’t realize that the critical window for fetal development starts before they know they’re pregnant. By the time a pregnancy test turns positive, the baby’s heart, brain, spine, and limbs have already begun forming - and any medication you’re taking could affect that process. That’s why creating a medication plan before conception isn’t just smart - it’s essential for a safe pregnancy.
Why Timing Matters More Than You Think
The first eight weeks of pregnancy are when the baby’s major organs form. This is called the embryogenic period. But here’s the catch: most women don’t even know they’re pregnant until week 5 or 6. By then, it’s too late to avoid certain risks. If you’re on a medication that’s known to cause birth defects - like valproic acid for seizures or isotretinoin for acne - waiting until you’re pregnant to stop it puts your baby at serious risk. According to the American College of Obstetricians and Gynecologists (ACOG), nearly half of all pregnancies in the U.S. are unintended. That means a lot of women are unknowingly exposed to medications during those first crucial weeks. The good news? You can prevent most of these risks by planning ahead.Start With a Full Medication Review
Don’t just think about your prescription drugs. Include everything: over-the-counter painkillers, herbal supplements, vitamins, and even acne treatments. Many people assume natural means safe, but that’s not true. St. John’s Wort, for example, can interfere with fertility and increase the risk of miscarriage. High-dose vitamin A (over 10,000 IU daily) can cause skull and heart defects. Make a list of every substance you take - even if you think it’s harmless. Bring this list to your doctor or pharmacist at least 3 to 6 months before you start trying to conceive. They’ll check each item against current teratogenicity databases. Some medications need to be stopped months in advance. Others can be swapped for safer alternatives.Key Medications to Watch Out For
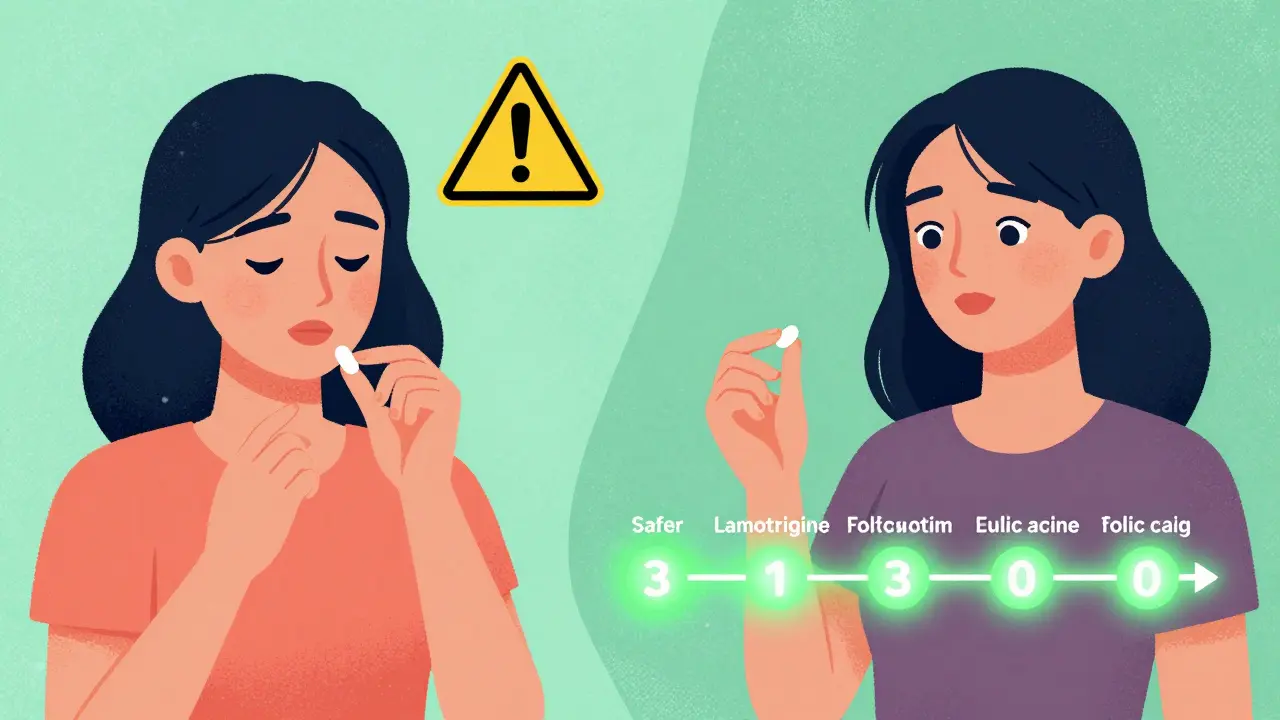
Here are some common drugs that require special attention before pregnancy:- Valproic acid (for epilepsy or bipolar disorder): Linked to a 10.7% risk of major birth defects, including neural tube defects and facial malformations. Switch to lamotrigine or levetiracetam if possible.
- Lithium (for bipolar disorder): Increases the risk of Ebstein’s anomaly, a rare heart defect. Requires careful monitoring and dose adjustment.
- Topiramate (for seizures or migraines): Doubles the risk of cleft lip or palate. Consider alternatives like gabapentin.
- Methotrexate (for rheumatoid arthritis or psoriasis): Highly teratogenic. Must be stopped at least 3 months before conception - and you need to use reliable contraception during that time.
- Warfarin (blood thinner): Crosses the placenta and can cause fetal warfarin syndrome. Switch to low-molecular-weight heparin before conception.
- Isotretinoin (Accutane for acne): Causes severe birth defects. Must be discontinued at least 1 month before trying to conceive, and you must use two forms of birth control during treatment and for one month after.
Folic Acid: The One Supplement You Can’t Skip
Folic acid is the single most important thing you can take before pregnancy. It reduces the risk of neural tube defects - like spina bifida - by up to 70%. But not all doses are the same.- If you’re healthy and have no chronic conditions: Take 400 to 800 micrograms (mcg) daily.
- If you have epilepsy, diabetes, obesity, or a family history of neural tube defects: Take 4 to 5 milligrams (mg) daily. That’s 5 to 10 times the standard dose.
- If you’re on anticonvulsants like valproic acid or carbamazepine: You’re at higher risk, and your body may break down folic acid faster. Stick with the 4-5 mg dose.
Managing Chronic Conditions Before Conception
If you have a long-term health condition, your medication plan needs to be more detailed.Thyroid disease: Your TSH level should be under 2.5 mIU/L before conception. If you’re on levothyroxine, your dose will likely need to increase by about 30% as soon as you get pregnant. Waiting until you’re pregnant to adjust it raises your risk of miscarriage by 60%.
Autoimmune diseases (like lupus or rheumatoid arthritis): Some drugs like cyclophosphamide and leflunomide are off-limits. But others, like sulfasalazine or hydroxychloroquine, are considered safe. Work with a rheumatologist to switch medications well before trying to conceive.
HIV: If you’re on antiretroviral therapy, aim for a viral load under 50 copies/mL before conception. This reduces the chance of passing HIV to your baby from 25% to less than 1%. Some medications, like efavirenz, are linked to birth defects - so your provider may switch you to dolutegravir or raltegravir.
Contraception Is Part of the Plan
If you’re taking a medication that needs to be stopped before pregnancy, you still need to prevent pregnancy during the transition. But here’s a problem: some seizure medications - like carbamazepine and phenytoin - make hormonal birth control less effective. Up to 47% of women on these drugs experience contraceptive failure. Solution? Use non-hormonal options like copper IUDs or condoms with spermicide. If you prefer hormonal methods, talk to your doctor about higher-dose pills or progestin-only options. Never rely on one method alone if you’re on enzyme-inducing drugs.Who Should Be Involved?
This isn’t something you do alone. You need a team:- Your OB/GYN or primary care provider: Coordinates everything.
- Your specialist: Neurologist, rheumatologist, endocrinologist, or psychiatrist - whoever manages your condition.
- Your pharmacist: They can flag dangerous interactions and help with timing.
- A genetic counselor (if needed): Especially if there’s a family history of birth defects or genetic conditions.

What If You’re Already Pregnant?
If you didn’t plan ahead and just found out you’re pregnant, don’t panic. But don’t wait either. Call your doctor immediately. Tell them every medication you’ve taken since your last period - even if you think it’s nothing. Many medications are safe during pregnancy, but you need expert guidance to know which ones. The key is to stop harmful drugs as soon as possible. For example, if you were on isotretinoin and just learned you’re pregnant, stopping it now still helps - the risk is highest in the first 6 weeks. Your provider can arrange an early anatomy scan to check for issues.Barriers to Getting This Done
Despite how important this is, only 24% of obstetric providers regularly do preconception medication reviews. Why? Time. Most appointments are 15 minutes. Many doctors don’t have access to updated teratogen databases. And if you’re in a fee-for-service system, there’s no financial incentive to spend time on prevention. But there’s good news: Kaiser Permanente, which uses integrated healthcare systems, achieves a 67% preconception review rate. That’s more than triple the national average. The difference? They have protocols, electronic alerts, and care teams built for this. If your doctor doesn’t bring it up, ask. Say: “I’m thinking about getting pregnant soon. Can we review my medications to make sure they’re safe?”The Bigger Picture
Countries like Sweden and the Netherlands have national preconception care programs. Their rates of major birth defects are 35% lower than in the U.S. That’s not because their genetics are better. It’s because they make this kind of planning standard - not optional. You don’t need to be perfect. You don’t need to overhaul your life overnight. But if you take one step - getting your meds reviewed 6 months before you try - you’re already doing more than most. And that small step could mean the difference between a healthy baby and a preventable tragedy.What if I’m on antidepressants and want to get pregnant?
Many antidepressants, including sertraline and citalopram, are considered low-risk during pregnancy. But others, like paroxetine, are linked to a slightly higher risk of heart defects. Never stop your medication suddenly - that can cause withdrawal or relapse. Work with your psychiatrist to switch to a safer option at least 2-3 months before conception. Your mental health matters just as much as your baby’s physical health.
Can I keep taking vitamins and herbal supplements?
Some are fine, others aren’t. Prenatal vitamins with folic acid are essential. But avoid high-dose vitamin A, black cohosh, dong quai, or goldenseal - they can trigger contractions or affect fetal development. Always check with your doctor before continuing any supplement, even if it’s labeled "natural."
How long should I wait after stopping a dangerous medication?
It depends on the drug. Methotrexate needs 3 months to clear from your system. Isotretinoin requires 1 month. Lithium and valproic acid need 1-2 months for stabilization. Your doctor will give you a timeline based on your specific meds. Don’t guess - this isn’t something to rush.
Do I need to see a specialist, or can my regular doctor handle this?
Your regular doctor can start the process, but if you have a chronic condition like epilepsy, diabetes, or lupus, you’ll need input from a specialist. A rheumatologist, neurologist, or endocrinologist knows which drugs are safest for your condition during pregnancy. Coordination between providers is key.
Is it safe to get pregnant if I have high blood pressure?
Yes - but not if you’re on ACE inhibitors or ARBs, which can cause kidney damage and skull defects in the fetus. Switch to methyldopa, labetalol, or nifedipine before conception. Control your blood pressure for at least 3 months before trying. Uncontrolled hypertension raises your risk of preeclampsia and preterm birth.
What if I’m over 35 and want to get pregnant?
Age increases risks for chromosomal conditions and complications like gestational diabetes. But a preconception medication plan can help. Review medications for diabetes, thyroid issues, or high blood pressure. Optimize your health before conception - it reduces age-related risks by up to 22%. Folic acid and weight management are especially important.
Can I use over-the-counter pain relievers before pregnancy?
Acetaminophen (Tylenol) is safe. Avoid NSAIDs like ibuprofen and naproxen if you’re trying to conceive. They can interfere with ovulation and may affect early embryo implantation. If you need pain relief, stick with acetaminophen and limit use. Always check with your doctor if you’re taking them regularly.

Emma Addison Thomas
January 8, 2026 AT 07:12My mum took valproic acid before she knew she was pregnant. I’m 32 now and perfectly fine, but I’ve spent years wondering if my mild scoliosis was linked. This post made me cry. Not because I’m scared, but because I wish someone had told her back then.
Everyone needs to read this. Even if you’re not planning it, you might be closer than you think.
Also, folic acid is non-negotiable. I take it daily. Even on days I eat junk food. It’s my tiny act of rebellion against chaos.
Christine Joy Chicano
January 8, 2026 AT 20:02Let’s be real - the real tragedy isn’t just teratogenic meds, it’s that the healthcare system treats preconception care like a luxury spa day instead of a medical imperative. We spend billions on IVF and neonatal ICUs, yet 76% of OB-GYNs don’t even ask about meds until you’re 8 weeks along.
And don’t get me started on how pharmacies still don’t flag high-dose vitamin A or St. John’s Wort in their automated alerts. It’s not negligence - it’s systemic apathy dressed up as efficiency.
Also, ‘natural’ doesn’t mean ‘non-teratogenic.’ If your herbalist can’t cite a PubMed study, they’re guessing. And you’re the lab rat.
Adam Gainski
January 10, 2026 AT 17:19As a pharmacist, I see this every day. A woman comes in for birth control refills, says she’s thinking about kids in 6 months, and I pull up her med list - and boom, there’s topiramate and methotrexate. Half the time, she’s never told her doctor.
It’s not about scaring people. It’s about giving them a roadmap. I hand out printed checklists now. One page. No jargon. Just: ‘Stop this. Switch to this. Wait this long.’
And yes, I’ve had patients cry because they didn’t know. That’s on us. Not them.
Anastasia Novak
January 12, 2026 AT 03:24Oh my god, I’m so glad this exists. I was on isotretinoin for 11 months. I thought ‘one month after’ was enough because I read it on WebMD. Then I got pregnant. My OB just shrugged and said ‘well, you’re lucky it’s not worse.’
Turns out, my daughter has a tiny cleft palate. Not life-threatening. But she had surgery at 6 months. And now I have to live with the fact that I didn’t read the damn label properly.
This isn’t just advice. It’s a damn lifeline. If you’re on any of these meds and you’re not planning - stop. Now. And get a copper IUD.
Also, folic acid is not a suggestion. It’s your baby’s bodyguard.
Elen Pihlap
January 12, 2026 AT 07:25why do you care so much about babies? i mean, like, are you sure you want to bring another human into this world? also, i heard that folic acid causes autism. is that true? i saw it on a tiktok. my cousin’s friend’s sister took it and her kid is nonverbal. so… what now?
Sai Ganesh
January 13, 2026 AT 23:54India has no formal preconception guidelines. We don’t even have teratogen databases in most hospitals. I work in a clinic in Bangalore. Last month, a 24-year-old came in with lithium and carbamazepine - both on full dose. She was 6 weeks pregnant and didn’t know.
We had to call the neurologist, the OB, and the pharmacist - all on the same call. Took three hours. No one was paid extra. No one got credit.
This post? It’s the first time I’ve seen this discussed in English with clarity. Thank you.
But the real problem? We don’t have the infrastructure to fix it. We need policy. Not just posts.
Paul Mason
January 14, 2026 AT 10:00Look, I’ve been doing this for 20 years. I’ve seen it all. The truth? Most women don’t care until it’s too late. And no, taking folic acid doesn’t make you a saint. It’s just basic hygiene.
And if you’re on antidepressants, don’t panic. Sertraline’s fine. Paroxetine? Maybe not. But if you’re scared to stop your meds? That’s your anxiety talking, not your doctor.
Also, if you think herbal tea is safer than a pill, you’re living in 1987. Wake up.
And for the love of God, stop taking ibuprofen if you’re trying. It’s not a ‘harmless painkiller.’ It’s a fertility saboteur.
Aparna karwande
January 16, 2026 AT 03:43Why are Westerners so obsessed with controlling every molecule in their body? In India, women get pregnant naturally, take no pills, eat ghee and turmeric, and deliver healthy babies. You think you’re smarter because you have a spreadsheet? This is arrogance wrapped in science.
My sister got pregnant on valproic acid. Baby is 7 now. Runs faster than your kid. No defects. No surgeries. Just pure Indian genetics and God’s grace.
Stop overmedicalizing motherhood. You’re not a lab rat. You’re a woman.
Ayodeji Williams
January 16, 2026 AT 09:04bro i just took 3 ibuprofen last week and now i’m trying to get pregnant 😭 is it too late??
also can i still drink coffee? i mean like 4 cups a day? i saw a vid that said caffeine causes miscarriage but then another vid said it’s fine if under 200mg??
also can i still take my ‘immune booster’ gummies? they have vitamin c and zinc and like… glitter?? 🤔
Anthony Capunong
January 18, 2026 AT 03:09Look, I’m a veteran. I’ve seen my wife go through three rounds of IVF. We had a miscarriage. Then we had our daughter. She’s 4 now. Perfect.
But here’s what no one tells you - if you’re on any of these meds, you’re not just protecting your baby. You’re protecting your marriage. Your sanity. Your future.
My wife cried for a week when she had to stop her anxiety med. But she did it. And we got our girl.
Don’t wait for the test to be positive. Do it before you even start trying. That’s love. Not luck.
Katrina Morris
January 18, 2026 AT 23:54thank you for this i just found out im pregnant and i was on topiramate and i panicked but i called my dr and they switched me to gabapentin right away and i started folic acid and im just so relieved
i didnt know any of this but now i feel like i can breathe again
also i love that you said natural doesnt mean safe because my aunt swore by her chamomile tea and now her grandkid has a heart thing
pls keep sharing this kind of stuff its so helpful