
Every year, thousands of children under five end up in emergency rooms because they swallowed medicine they weren’t supposed to. It’s not because parents are careless-it’s because medication poisoning is sneakier than most people realize. A child doesn’t need to be left alone to get into medicine. They just need to see a bottle on a counter, hear a parent say "this is candy," or find a purse left on the couch. And when it happens, the clock starts ticking fast.
Most Poisonings Happen at Home-And Often When Adults Are Around
Over 90% of accidental medicine poisonings in kids happen inside the home. Shockingly, most of these incidents occur while a parent or caregiver is right there-distracted for just a few seconds. Maybe they’re answering a phone call. Maybe they’re pouring their own coffee. Maybe they’re putting their own pills down while helping a toddler get dressed. That’s all it takes.
According to data from Poison Control, 58% of these incidents happen between noon and 6 p.m.-not at night, as many assume. This is when families are most active, and distractions are highest. A 2022 study from Nationwide Children’s Hospital found that 40% of poisonings happened because a parent was actively using a medication (like applying a topical cream or pouring a liquid dose) and turned away for even a moment. The medicine didn’t disappear. The child just moved faster.
What Medicines Are Most Dangerous?
Not all medicines are created equal when it comes to risk. The top three offenders in accidental poisonings are:
- Acetaminophen (Tylenol, Panadol)
- Ibuprofen (Advil, Motrin)
- Aspirin (especially in liquid form)
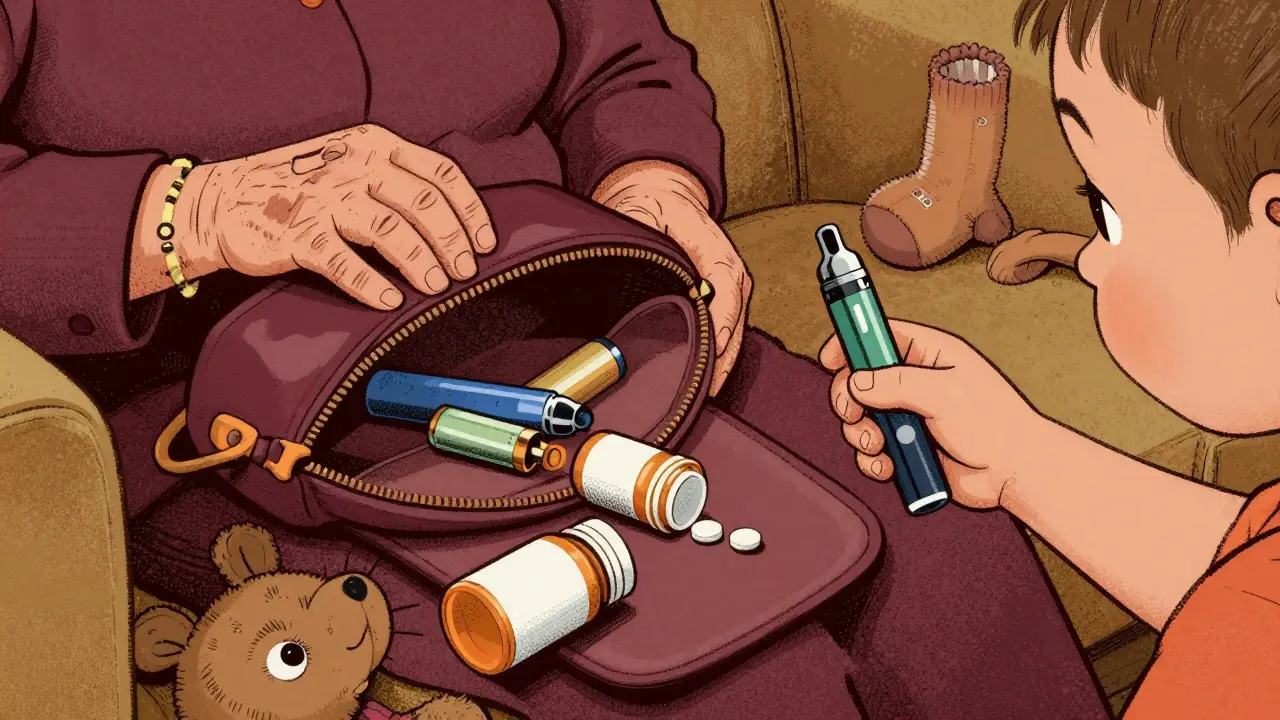
These are common, easy to find, and often stored in plain sight. But even more alarming is the rise in poisonings from liquid nicotine in e-cigarettes. Just half a milliliter-a teaspoon’s worth-can be fatal to a toddler. Many parents don’t realize these pens and cartridges are as dangerous as pills. They think, "It’s just vape juice." But nicotine is a potent neurotoxin. A single cartridge can contain enough to kill two children.
Antihistamines, cold syrups, and sleeping pills also top the list. They’re often labeled "gentle" or "for kids," which makes parents think they’re safe to leave out. They’re not.
Why "Child-Resistant" Isn’t Enough
You’ve probably heard: "Use child-resistant caps." That’s good advice-but it’s not enough. Child-resistant doesn’t mean childproof. It means a child under two might struggle to open it. A 16-month-old who’s been watching you for months? They’ve already figured out how to twist, pull, and pry. By age two, many toddlers can open these caps in under 30 seconds.
And here’s the real problem: 25% of poisonings happen when medicine is taken out of its original container. A parent transfers liquid Tylenol into a juice bottle because it’s easier to carry. Or they dump pills into a pill organizer because they don’t want to fumble with the bottle. Suddenly, the child doesn’t recognize it as medicine. It looks like juice. It looks like candy. And they’re not afraid to try it.
Storage Mistakes That Put Kids at Risk
Where you store medicine matters more than how you cap it. Here are the most common-and deadly-mistakes:
- Storing medicine in purses, bags, or coat pockets. Thirty percent of poisonings come from visitors’ belongings. Grandparents, babysitters, or friends leave their medications in a handbag on the floor. A toddler pulls it out. Done.
- Leaving medicine on counters, nightstands, or tables. The Rural Health Information Hub found that 78% of poisonings involve items stored below 4 feet-the height a toddler can reach. Even if it’s "up high," if it’s on a dresser or bedside table, it’s within reach.
- Using kitchen spoons to measure doses. Over 40% of dosing errors happen because parents use a regular spoon. A teaspoon isn’t 5 mL. It’s anywhere from 3 to 7 mL. That’s a 40% overdose risk. Always use the syringe or cup that came with the medicine.
And never, ever call medicine "candy." It sounds harmless. But research from the American Academy of Pediatrics shows that children who hear medicine called "candy" are 3.2 times more likely to take it without asking. They don’t understand the difference between a reward and a treatment. They just know it tastes sweet.
How to Lock It Down-For Real
Here’s what works, based on real-world data from hospitals and poison control centers:
- Use locked cabinets. Not just closed. Not just high up. Locked. Magnetic locks that require a key or code are best. Place them at least 54 inches off the floor-beyond the reach of even the most determined climber.
- Install automatic-locking latches. These click shut when the cabinet door closes. They’re cheap, easy to install, and effective. But test them. Kids can learn to push, pull, or wiggle them open. If your latch doesn’t stay locked, replace it.
- Store medicine in its original container. No transfers. No pill organizers. No juice bottles. The label tells you what it is, the dose, and the expiration date. If you can’t see that, you can’t trust it.
- Check every room. Get down on your hands and knees. Look from a child’s eye level. Where do they sit? Where do they climb? What’s within reach? A medicine bottle on the bathroom counter? A pill bottle in the kitchen cabinet? A vape pen in the bedroom drawer? These are all risks.
- Keep medicine away from visitors. If someone comes over, ask them to keep their medications in a locked bag or leave them in the car. If they forget, offer them a secure spot. A locked drawer. A high shelf. A small lockbox.
Developmental Surprises: What Kids Can Do Before You Expect It
Children develop faster than we think. By 18 months, many can climb onto chairs, pull open drawers, and reach over the edge of a crib. By age two, they can turn doorknobs, open cabinets with latches, and mimic adult behavior. By age three, they can read labels, recognize shapes, and remember where things are kept.
UCSF Benioff Children’s Hospital advises parents to think ahead: "Anticipate what your child will be able to do in the next three to six months, and secure things before they get there." Don’t wait until they start climbing. Lock it up before they even try.

Emergency Prep: What to Do If It Happens
Even with the best precautions, accidents happen. Here’s what you need to have ready:
- Post the Poison Help number (1-800-222-1222) on your fridge, near the phone, and on your phone’s speed dial. Homes with this number posted respond 47% faster in emergencies.
- Save webPOISONCONTROL in your phone’s bookmarks. It’s free, instant, and available 24/7. You don’t need to wait for an ambulance. Call or go online immediately.
- Know basic CPR and the Heimlich maneuver for children. Twelve percent of severe poisoning cases require immediate intervention before help arrives. Training takes 30 minutes. It’s worth it.
- Do not wait for symptoms. If you suspect your child swallowed medicine, call Poison Control immediately-even if they seem fine. Some drugs take hours to show effects. By then, it’s too late.
Poison Control’s data shows that if you call within five minutes of exposure, outcomes improve by 89%. Delaying by even 20 minutes can mean the difference between a quick recovery and a hospital stay.
What’s Working: Real Solutions That Reduce Poisonings
Some communities are making real progress:
- Free lockboxes from pharmacies. Nationwide Children’s Hospital gives out free, childproof lockboxes to families with toddlers. Households that use them see a 41% drop in medicine access incidents.
- "Up and Away" campaigns. These public education efforts, run by poison control centers, have cut pediatric exposures by 19% in areas where they’re active.
- Smart medicine containers. Pilot programs with containers that track usage and send alerts to phones have reduced unsupervised access by 63%. These aren’t science fiction-they’re here, and they’re getting better.
The goal isn’t perfection. It’s reduction. Every locked cabinet, every labeled bottle, every saved phone number makes a difference.
Final Thought: It’s Not About Trust-It’s About Design
You trust yourself. You trust your partner. You trust your grandparents. But kids don’t understand trust. They understand access. They understand curiosity. They understand sweet-tasting things.
Preventing medicine poisoning isn’t about being a perfect parent. It’s about designing a home that doesn’t rely on memory, attention, or good intentions. It’s about locks, labels, and location. It’s about putting the medicine where no child can reach-no matter how smart, how fast, or how curious they are.
What should I do if my child swallows medicine?
Call Poison Control immediately at 1-800-222-1222 or go online to webPOISONCONTROL. Do not wait for symptoms. Do not induce vomiting. Have the medicine container ready when you call. They’ll tell you if you need to go to the ER or if you can manage it at home. Time matters-calling within five minutes improves outcomes by 89%.
Are child-resistant caps enough to keep kids safe?
No. Child-resistant caps are designed to slow down a child under two, not stop them. By age 18 months, many toddlers can open them. Studies show over 25% of poisonings happen because medicine was taken from a bottle with a child-resistant cap. Always combine caps with locked storage.
Can I store medicine in the bathroom?
Only if it’s in a locked cabinet, and even then, it’s risky. Bathrooms are humid, which can degrade medicine. Plus, toddlers climb onto toilets, sinks, and counters. A locked cabinet in a bedroom or closet is safer. If you must keep it in the bathroom, use a magnetic lock at least 54 inches high.
Why is it dangerous to call medicine "candy"?
Research shows children who hear medicine called "candy" are 3.2 times more likely to take it without asking. Kids don’t understand context. If it tastes sweet and you call it candy, they’ll assume it’s a treat. Never use food-related terms for medicine-no matter how tempting.
Is it safe to keep medicine in a purse or pocket?
No. Thirty percent of poisonings come from medications left in purses, bags, or coat pockets. Visitors, grandparents, or even your own jacket on the chair can be a hazard. Always store medicine in a locked cabinet. If someone brings medicine to your home, offer them a secure place to keep it.
How can I prevent dosing errors?
Always use the measuring tool that came with the medicine-never a kitchen spoon. Teaspoons vary by 20-40% depending on the spoon. Use a syringe or dosing cup marked in milliliters. Write down the dose and time on a sticky note if you’re distracted. Double-check the label every time.
Are there any tools or programs that help prevent poisonings?
Yes. Many pharmacies offer free childproof lockboxes to families with toddlers. Programs like "Up and Away" and community pharmacy safety initiatives have reduced poisonings by 19-41%. Smart medicine containers with usage tracking and parental alerts are now available and have cut unsupervised access by 63% in pilot tests.




Mike Hammer
February 14, 2026 AT 22:34Man, I never thought about how fast toddlers move. I thought if I just put the medicine up high, I was good. Then my niece opened my cabinet like it was a toy box. 18 months old. No joke. I now have magnetic locks on everything. Scary stuff.
Charlotte Dacre
February 15, 2026 AT 18:14So let me get this straight - we’re supposed to turn our homes into Fort Knox just because kids are curious? 😏 My kid once tried to ‘medicate’ the dog with my Advil. We laughed. Then I bought a lockbox. Still laughing.
Virginia Kimball
February 17, 2026 AT 14:51This is the kind of post that makes you want to hug your kids and lock everything away. I used to keep my vitamins on the nightstand because I was ‘too lazy’ to walk to the closet. Now? Locked cabinet. Downstairs. With a code. And I still check twice. Better safe than sorry - and honestly, I’d rather be annoying than grieving.
Betty Kirby
February 17, 2026 AT 15:09People still use kitchen spoons to measure medicine? Are you serious? This isn’t 1995. You have a smartphone. You have a measuring cup. You have Google. Stop being lazy. Your child’s liver doesn’t care about your convenience.
Daniel Dover
February 18, 2026 AT 07:58Lock it up. Simple.
Sarah Barrett
February 19, 2026 AT 13:57The data on liquid nicotine is terrifying. I didn’t realize a single cartridge could be lethal to two children. I’ve since removed all vape pens from our home - even though I don’t use them. Better to be safe than sorry. This isn’t a ‘maybe’ - it’s a ‘must’.
Erica Banatao Darilag
February 19, 2026 AT 21:25I didn’t know calling medicine ‘candy’ was that dangerous. My mom used to say that to get me to take my syrup. I thought it was a treat. I still remember the taste. I never asked again. I’m so glad this is being talked about. We need to stop normalizing this.
Chiruvella Pardha Krishna
February 19, 2026 AT 23:12It is not enough to lock. It is not enough to educate. We must redesign society. The modern home is a battlefield of convenience. The child does not ask for permission. The child does not understand labels. The child understands only hunger - for taste, for touch, for truth. We must build walls not of wood, but of foresight. We must become architects of safety - not parents who hope.
Kapil Verma
February 21, 2026 AT 13:14India has 300 million kids under five. We don’t have lockboxes. We don’t have magnetic latches. We have grandmas who keep pills in their dupattas. You think this is a US problem? This is a global crisis. Stop talking about cabinets. Start talking about policy. Free lockboxes. Mandatory labeling. Public service announcements in every language. Or we will keep burying children. And you will keep scrolling.
Josiah Demara
February 23, 2026 AT 03:08Let’s be real - 90% of these parents are just lazy. They don’t want to install a lock. They don’t want to move the medicine. They’d rather rely on ‘child-resistant caps’ like it’s a magic spell. Then they act shocked when their kid gets sick. It’s not a tragedy. It’s negligence dressed up as ‘I’m busy.’
Esha Pathak
February 24, 2026 AT 01:53My daughter is 16 months. She climbs like a ninja. I used to keep my insulin on the counter. Now? Locked. In the basement. Behind a door with a keypad. I used to think I was careful. Turns out, I was just lucky. I cried when I read this. Not because I’m scared - because I realized I wasn’t doing enough. So I bought three lockboxes. One for medicine. One for cleaning. One for her own toys (yes, she’s already trying to open the toy box). Kids don’t wait. Neither should we.
Michael Page
February 25, 2026 AT 03:44The real tragedy isn’t the poisonings. It’s that we treat this like a parenting flaw instead of a systemic design failure. We blame mothers. We shame caregivers. We don’t build infrastructure. We don’t fund public lockbox programs. We don’t regulate pill packaging. We just say ‘be careful.’ That’s not prevention. That’s hope with a side of guilt.
Mandeep Singh
February 26, 2026 AT 19:57Look, I’ve been a nurse for 22 years. I’ve seen 147 pediatric poisonings. Let me tell you what actually works: 1) Lock boxes - yes. 2) Education - yes. 3) Smart containers with alerts - YES. 4) Removing ALL non-essential meds from the home - ESPECIALLY if you’re visiting someone with kids. 5) Never, ever, ever leave your purse on the floor. Ever. I had a mom tell me her sister’s purse had the liquid nicotine. The baby died. That purse was on the couch. The mom was on the phone. That’s not a mistake. That’s a failure of awareness. And we’re not talking about it enough. Stop scrolling. Start securing.