When your kidneys aren't working right, your electrolytes pay the price. Potassium, phosphate, and magnesium aren't just numbers on a lab report-they're the invisible forces keeping your heart beating, your muscles moving, and your nerves firing. Get these out of balance, and you could be looking at arrhythmias, muscle weakness, or even sudden respiratory failure. This isn't theoretical. In hospitals across Australia and beyond, electrolyte imbalances are among the top causes of preventable in-hospital deaths, especially in patients with kidney disease, heart failure, or those on diuretics.
Why These Three Electrolytes Matter More Than Others
Potassium controls how your heart cells recharge between beats. Too little, and your heart can flutter dangerously. Too much, and it can stop. Phosphate is the fuel currency of your cells-without enough, your lungs can’t expand properly, and your muscles give out. Magnesium? It’s the quiet enabler. It’s needed for potassium to stay inside cells and for phosphate to work right. You can’t fix low potassium if magnesium is also low. It’s like trying to fill a bucket with a hole in the bottom.
Normal ranges are tight: potassium between 3.2 and 5.0 mEq/L, magnesium at 1.7 to 2.2 mg/dL, phosphate at 2.5 to 4.5 mg/dL. But the real danger zone starts at the edges. Potassium below 3.0 or above 6.5 mEq/L? That’s an emergency. Magnesium under 1.0 mg/dL? You’re at risk for life-threatening heart rhythms. Phosphate below 1.0 mg/dL? Your breathing muscles may shut down.
The Hidden Link: Magnesium and Potassium Dependence
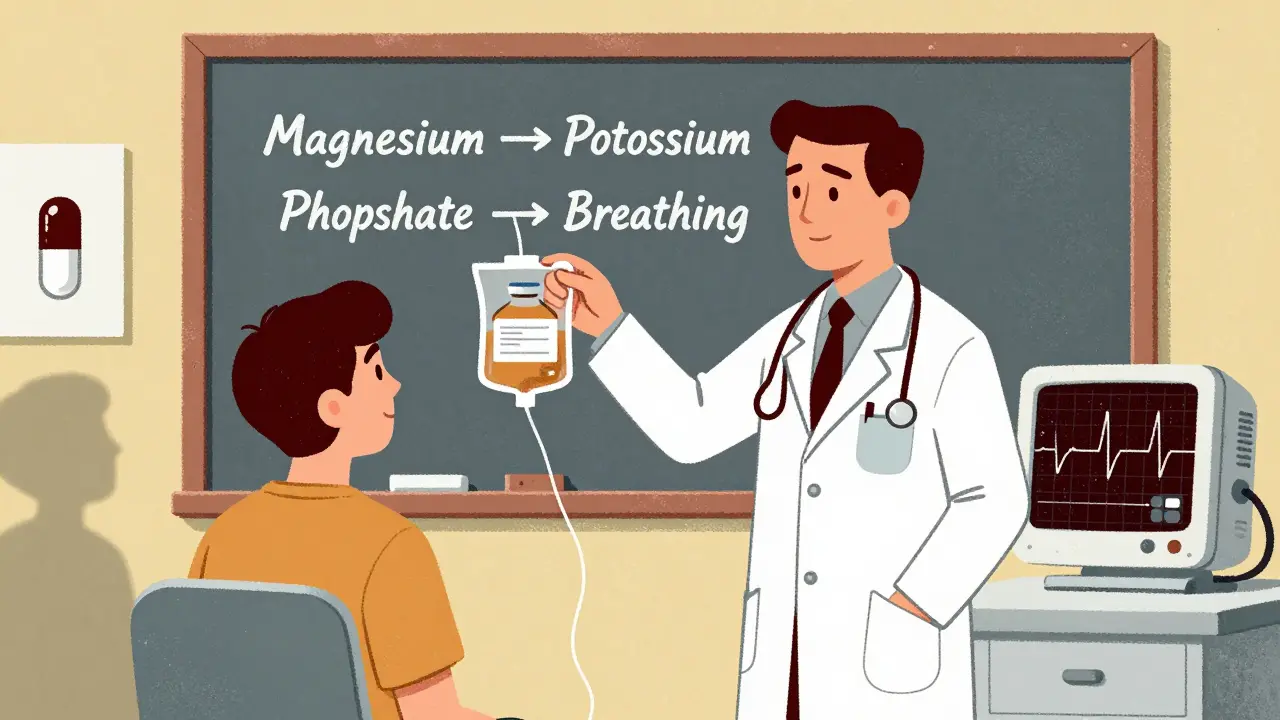
Here’s what most clinicians miss: you can give someone 100 mEq of potassium IV and still see no change in their blood levels-if their magnesium is low. Why? Because low magnesium makes the kidneys dump potassium like it’s trash. This isn’t a theory. It’s in the 2023 American Heart Association guidelines and confirmed by studies from Vanderbilt University Medical Center. If you’re treating a patient with persistent low potassium, check magnesium first. Always.
And it’s not just about replacement. Low magnesium also makes low calcium harder to fix. It’s a chain reaction. That’s why protocols now require magnesium to be corrected before potassium in any serious case. In the ER, we don’t just reach for the KCl bag anymore. We grab the magnesium sulfate first.
How to Correct Low Potassium-Safely
Oral potassium chloride is fine for mild cases-think 20-40 mEq per day split into doses. But if someone’s potassium is under 3.0 mEq/L and they’re dizzy, weak, or have abnormal ECG changes? You need IV. But here’s the catch: you can’t just dump it in fast.
Peripheral IV? Max 10 mEq per hour. Any faster, and you risk burning the vein or triggering cardiac arrest. Central line? Up to 40 mEq per hour, but only if you’re watching the ECG like a hawk. Every 15 minutes. You should expect a rise of about 0.25 mEq/L for every 20 mEq of IV potassium given. That means if someone’s at 2.8 mEq/L, you’re not going to get them to 4.0 in one hour. Patience saves lives.
And don’t forget: if they’re on diuretics like furosemide or spironolactone, you’re playing a losing game unless you’re replacing magnesium too. That’s why many hospitals now use combo packs: potassium and magnesium together in the same bag for high-risk patients.
Phosphate: The Silent Killer in ICU Patients
Phosphate drops quietly. You won’t feel it until your patient can’t breathe. That’s because low phosphate means your diaphragm can’t contract. It’s why critically ill patients-especially after surgery, trauma, or refeeding-are at high risk. Even more surprising: iron infusions. Since 2020, the FDA has flagged ferric carboxymaltose as a major cause of severe hypophosphatemia. If someone gets a big iron infusion and then gets weak or short of breath a few days later? Check phosphate.
For mild cases, oral phosphate works well-8 mmol per dose, 2-3 times a day. But if phosphate is under 1.0 mg/dL? You need IV. Standard dose: 7.5 mmol over 4-6 hours. Too fast? You risk calcium dropping, or worse, calcium-phosphate crystals forming in soft tissues. That’s why you monitor calcium every 4-6 hours during replacement. And never, ever give phosphate without checking magnesium. Again, they’re linked.
When Potassium Goes Too High-Hyperkalemia Emergency
High potassium is a ticking time bomb. Especially in kidney patients. ECG changes? Peaked T waves, widened QRS, flat P waves? That’s not just a lab result-it’s a cardiac arrest waiting to happen.
For potassium over 7.0 mEq/L with ECG changes, you don’t wait. You act in order:
- Give calcium gluconate (10-20 mL of 10% solution) over 2-3 minutes. This doesn’t lower potassium-it protects the heart from it.
- Give insulin (10 units) with 50g of dextrose. This shifts potassium into cells. Effect starts in 15 minutes.
- Use a potassium binder: patiromer or sodium zirconium cyclosilicate. These are newer, safer than old kayexalate, and approved by NICE since early 2023.
- If the patient has kidney failure or levels won’t drop? Dialysis. Fast.
Monitoring after treatment is non-negotiable. Check potassium at 1, 2, 4, 6, and 24 hours. Why? Because the insulin effect wears off. The potassium can rebound. And if you don’t catch it, the patient crashes.
Hypermagnesemia: Rare, But Deadly
This usually happens in kidney patients who get too much magnesium-like from antacids, laxatives, or IV magnesium for pre-eclampsia. Levels above 2.5 mg/dL? You start seeing muscle weakness. Above 4.0? You get paralysis, low blood pressure, and stopped breathing.
Treatment? Stop magnesium. Give calcium gluconate (10-20 mL IV) to reverse the neuromuscular block. If kidneys are working, give furosemide to flush it out. If not? Dialysis. No shortcuts.
Who’s at Risk? Screening Saves Lives
You don’t need to test everyone. But you should test:
- All hospitalized patients with kidney disease (eGFR under 45)
- Anyone on diuretics, ACE inhibitors, or ARBs
- Patients with heart failure or recent heart attack
- Those on IV iron infusions (ferric carboxymaltose)
- People with eating disorders, alcoholism, or recent refeeding
- Anyone with unexplained muscle cramps, palpitations, or fatigue
Many hospitals now use automated alerts in their electronic systems. If a patient’s potassium drops below 3.5 mEq/L, the system flags it and suggests checking magnesium and phosphate. Since 2021, teaching hospitals that implemented these protocols saw a 22.4% drop in electrolyte-related adverse events, according to JAMA Internal Medicine.
What’s New in 2025?
Point-of-care testing is now standard in most emergency departments. You can get a potassium result in under 10 minutes-not hours. That’s cut the time to treatment by 37 minutes on average, according to Annals of Emergency Medicine (2023).
New phosphate binders are helping kidney patients stay out of the danger zone for phosphate. And researchers are starting to look at genetics. Some people naturally lose more potassium or magnesium through urine. Phase 3 trials for genotype-guided replacement are wrapping up in late 2024. Soon, we may be tailoring doses based on DNA, not just lab values.
Bottom Line: Think in Systems, Not Single Numbers
Electrolytes don’t work alone. You can’t fix potassium without checking magnesium. You can’t fix phosphate without watching calcium. You can’t treat hyperkalemia without protecting the heart first. These aren’t isolated lab values-they’re pieces of a living system.
Every time you order a basic metabolic panel, ask yourself: What’s the story behind these numbers? Is this patient on diuretics? Did they get iron? Are they eating? Are they in kidney failure? The answer isn’t in the lab-it’s in the patient’s history.
Fixing electrolytes isn’t about giving pills or IVs. It’s about understanding the chain of events that broke them-and stopping the next one before it starts.
Can low magnesium cause low potassium even if I’m giving potassium supplements?
Yes. Low magnesium causes the kidneys to keep throwing out potassium, no matter how much you give. This is called "refractory hypokalemia." You must correct magnesium first-usually with 4 grams of IV magnesium sulfate-before potassium replacement will work. This is standard practice in all major hospital protocols as of 2025.
Is it safe to give potassium IV at home?
No. IV potassium replacement should only be done in a monitored setting like a hospital or clinic. Even at slow rates, it can cause dangerous heart rhythms if given incorrectly. Oral supplements are safe for mild cases, but IV potassium requires continuous ECG monitoring, trained staff, and immediate access to emergency drugs like calcium gluconate.
Why do kidney patients keep getting low phosphate?
Kidney patients often take phosphate binders to control high phosphate levels. But if they’re not eating enough, or if they’re on certain iron infusions like ferric carboxymaltose, their phosphate can crash. Also, when kidney function worsens, the body loses its ability to make active vitamin D, which is needed to absorb phosphate from food. It’s a perfect storm.
Can I just take magnesium supplements to prevent imbalances?
For healthy people, yes-magnesium supplements can help if your diet is low. But if you have kidney disease, taking extra magnesium can be dangerous. Your kidneys can’t clear it, and it builds up. Always check with your doctor before taking supplements if you have kidney issues, heart disease, or take diuretics.
How long does it take to correct a severe electrolyte imbalance?
It depends. Severe hyperkalemia can be stabilized in minutes with calcium and insulin. But getting potassium back to normal safely takes 24-48 hours. Phosphate and magnesium replacement usually takes 2-5 days, depending on severity and how well you’re eating. Rushing it can cause rebound problems. Slow and steady wins the race.
Are there foods I should eat to naturally balance these electrolytes?
Yes. For potassium: bananas, potatoes, spinach, beans. For magnesium: nuts, seeds, whole grains, dark chocolate. For phosphate: dairy, meat, fish, eggs. But if you have kidney disease, you may need to limit some of these. For example, too much potassium from bananas can be dangerous if your kidneys can’t clear it. Always tailor your diet to your kidney function and doctor’s advice.



Usha Sundar
December 25, 2025 AT 00:25This post is fire. I’ve seen patients crash because someone forgot magnesium. Always check it first. Period.
Done.
Wilton Holliday
December 25, 2025 AT 20:08Thank you for laying this out so clearly. As a nurse in a rural ER, I’ve seen too many near-misses because we were chasing potassium and missed the magnesium hole. This is the kind of stuff that saves lives. 🙌
Also, the point about IV iron causing hypophosphatemia? Huge. We missed it on a post-op patient last month. Lesson learned.
Harsh Khandelwal
December 26, 2025 AT 00:45Big Pharma doesn’t want you to know this, but magnesium is cheaper than potassium and they don’t make billions off it. They’d rather you keep giving KCl and charging for it every time it fails. Meanwhile, your patient’s heart keeps flipping out.
Also, check if they’ve been taking TUMS for ‘indigestion’ - that’s magnesium in disguise. They’re getting it from the pharmacy, not the fridge.
Delilah Rose
December 27, 2025 AT 15:19I really appreciate how this breaks down the interconnectedness of these electrolytes - it’s not just about fixing numbers, it’s about understanding the body’s systems like a web. I used to think potassium was the main villain, but now I see magnesium as the silent gatekeeper. It’s like trying to water a plant with a broken hose - you pour and pour and nothing sticks. And phosphate? I never realized how quietly it could steal someone’s breath. This changed how I look at every metabolic panel now. I’m printing this out and taping it to my station.
Also, the part about genotype-guided replacement? That’s the future. We’re moving from guesswork to precision, and I’m here for it.
Spencer Garcia
December 29, 2025 AT 00:31Spot on. We started using combo K+Mg bags in our med-surg unit last year. Adverse events dropped 30%. Simple fix, huge impact.
Also, the 2023 AHA guidelines mention this - it’s not new, but it’s still underused.
Bret Freeman
December 29, 2025 AT 21:50Let me guess - this was written by someone who gets paid to push hospital protocols. Real doctors know you don’t need all this fancy stuff. If a patient’s potassium is low, give them a banana and shut up. You’re overcomplicating everything. And don’t get me started on IV phosphate - that’s just giving people chemical cocktails because you’re too lazy to let them eat food.
Also, ‘genotype-guided replacement’? Next you’ll be telling me we need DNA tests before giving aspirin.
John Pearce CP
December 31, 2025 AT 15:47While the clinical details presented are accurate, the normalization of intravenous electrolyte replacement without stringent regulatory oversight in non-specialized settings is alarming. The erosion of procedural discipline in favor of expedience is a dangerous trend. In my tenure at Johns Hopkins, we never administered potassium IV without a dedicated physician and telemetry monitoring - not because of protocol, but because of principle. This article, while well-intentioned, contributes to a culture of complacency.
Furthermore, the casual mention of ‘combo packs’ suggests a commodification of care that undermines clinical judgment.
Ajay Sangani
January 1, 2026 AT 16:06what if the real problem isnt the electrolytes but the fact we treat the body like a machine with dials to turn? maybe we should ask why the kidneys are failing in the first place… why is the patient on diuretics? why is their diet so broken? fixing potassium is like patching a leaky roof while the whole house is on fire
also… magnesium is ancient. we’ve known this for centuries. why did it take 2025 for hospitals to care?
Lu Jelonek
January 3, 2026 AT 06:34As someone who grew up in a household where my grandmother used Epsom salt baths for everything - cramps, stress, even ‘bad blood’ - I never thought it had a place in ICU protocols. But this? This makes sense. The body’s been telling us this for ages. We just stopped listening.
Also, the part about phosphate and iron infusions? I’ve seen that in my mother’s case. She got an iron drip, then spent three days in bed. No one connected the dots. This should be mandatory reading for all new nurses.
siddharth tiwari
January 4, 2026 AT 11:20they’re hiding the truth. magnesium sulfate is banned in some countries because it’s too effective and too cheap. the pharmaceutical industry makes billions from kcl and binders. why do you think they made kayexalate a thing? it’s expensive and full of side effects. they want you dependent. check the patent dates. they’re not accidents.
also… why is this article so detailed? who funded it?
Adarsh Dubey
January 6, 2026 AT 02:52One of the clearest summaries I’ve read on this. The magnesium-potassium link is so often overlooked, even by seasoned clinicians. I’ve had patients with ‘refractory hypokalemia’ who improved within hours after a single IV magnesium dose. No drama. No fuss. Just science.
Also, the point about point-of-care testing cutting response time by 37 minutes? That’s not just efficiency - that’s survival.
Bartholomew Henry Allen
January 7, 2026 AT 16:47While the data presented is methodologically sound, the casual tone undermines the gravity of clinical electrolyte management. The use of phrases such as bucket with a hole and ticking time bomb is inappropriate for professional discourse. Furthermore, the recommendation to use combo packs without explicit dosing parameters may lead to iatrogenic harm in non-specialist settings. This article should be accompanied by a formal clinical pathway and institutional review board approval before dissemination.
Respectfully submitted,
Bartholomew Henry Allen MD, FCCM