If you’ve ever used an inhaler for asthma or COPD, you’ve probably held two different devices in your hands-one blue, one brown-and been told to use them at different times. But do you actually know why you need both? It’s not just about having options. It’s about two completely different ways of fixing your breathing problems-one quick, one slow, and both essential.
How Bronchodilators Open Your Airways
Bronchodilators are the fast-acting heroes of respiratory care. They don’t fix inflammation. They don’t cure anything. What they do is simple: they relax the tight muscles squeezing your airways shut. Think of your airways like a garden hose that’s been stepped on. Bronchodilators step in and kick the pressure off, letting air flow again. There are two main types. The first are beta-2 agonists like albuterol (also called salbutamol). These drugs bind to receptors in your lung muscles and trigger a chemical chain reaction that tells those muscles to loosen up. You feel the difference in 15 to 20 minutes. The effect lasts 4 to 6 hours for the short-acting versions-those are your rescue inhalers. The long-acting ones, like salmeterol or formoterol, take a little longer to kick in (around 30 minutes) but keep your airways open for 12 hours or more. The second type is anticholinergics, like ipratropium and tiotropium. These work by blocking a nerve signal that tells your airways to tighten. They’re often used in COPD, especially when beta-2 agonists aren’t enough. Ipratropium works in about the same time as albuterol, but tiotropium gives you 24-hour coverage with just one puff a day. Here’s the catch: bronchodilators are only for symptom relief. If you’re using your rescue inhaler more than two or three times a week, something’s wrong. That means your airways are still inflamed underneath-and that’s where corticosteroids come in.How Corticosteroids Quiet the Inflammation
Corticosteroids are the quiet, long-term fixers. They don’t make you breathe easier right away. In fact, if you take one during an asthma attack, you won’t feel any immediate relief. That’s because they’re not targeting muscle tension-they’re targeting the root cause: inflammation. These drugs work at the genetic level. Once inhaled, they enter the cells lining your airways and bind to receptors that control inflammation genes. They turn down over 100 genes that cause swelling, mucus production, and immune cell activity. At the same time, they turn up genes that help calm things down. It’s like flipping a switch from chaos to calm. Common inhaled corticosteroids include fluticasone (Flovent), budesonide (Pulmicort), beclomethasone (Qvar), and mometasone (Asmanex). They’re not instant. It takes days-sometimes weeks-of daily use before you notice a real difference. But over time, they reduce flare-ups by 30% to 50%. Studies show people who take them regularly have far fewer hospital visits, fewer missed workdays, and better lung function over years. But here’s the problem most people don’t talk about: if you don’t rinse your mouth after using a corticosteroid inhaler, you’re asking for trouble. About 5% to 10% of users get oral thrush-a fungal infection that causes white patches and soreness in the mouth. It’s not dangerous, but it’s annoying. And 38% of users report hoarseness or voice changes. Both are preventable with a simple rinse and spit after every use.Why You Need Both-And in That Order
The real magic happens when you use them together. Bronchodilators open the door. Corticosteroids walk through it. When your airways are tight, inhaled steroids can’t reach the deeper parts of your lungs. They hit the big tubes and bounce off. But if you use a bronchodilator first, your airways widen. The steroid particles can travel farther, stick better, and do their job more effectively. That’s why experts insist on a strict sequence: bronchodilator first, wait five minutes, then corticosteroid. It’s not a suggestion. It’s science. A 2023 Cleveland Clinic study found patients who followed this order had 40% better medication deposition in their small airways compared to those who mixed them up or skipped the wait. And it’s not just about technique-it’s about timing. If you’re using a long-acting bronchodilator like formoterol as part of your daily maintenance, it’s often combined with a corticosteroid in one inhaler-like Symbicort or Advair. These combination devices are now used in 68% of asthma prescriptions in the U.S. because they simplify treatment and improve adherence. But here’s the danger: never use a long-acting bronchodilator alone. The SMART trial in 2006 showed that people using LABAs without corticosteroids had a 3.5 times higher risk of asthma-related death. That’s why the FDA requires a black box warning on all LABA-only inhalers. They’re not meant to be used by themselves.
What Patients Actually Experience
Real people don’t read guidelines. They live with their inhalers every day. On Reddit’s asthma forum, 78% of 1,245 users said their symptoms improved dramatically once they started waiting five minutes between inhalers. One user wrote: “I thought my Pulmicort wasn’t working. Turns out I was spraying it into a closed door. Once I used my blue inhaler first, my brown one finally did something.” But side effects are a big concern. On Drugs.com, 65% of users reported shaking hands, fast heartbeat, or nervousness after using albuterol. That’s normal. It’s not dangerous for most people, but it’s uncomfortable. For corticosteroids, the big complaints are thrush and hoarseness. And while 42% of patients in a Mayo Clinic survey had at least one episode of thrush, only 31% rinsed their mouth after every use. The biggest mistake? Confusing rescue and maintenance inhalers. A 2022 American Lung Association survey found that 44% of asthma patients couldn’t tell which inhaler was for daily use and which was for emergencies. That’s dangerous. Using a rescue inhaler every day means your disease isn’t under control-and you’re missing the chance to prevent damage.What’s New in 2026
The field is evolving fast. In 2023, the FDA approved Airsupra-the first as-needed combination inhaler. It contains albuterol and budesonide in one device. You use it only when you feel symptoms, and it gives you both quick relief and anti-inflammatory action at the same time. The Global Initiative for Asthma (GINA) now recommends this approach for mild asthma instead of using albuterol alone. Why? The SYGMA trials showed a 64% drop in severe flare-ups when patients used this combo as needed. Another big shift? Triple therapy. For severe COPD, doctors are now prescribing inhalers that combine a long-acting bronchodilator, another type of bronchodilator (called a LAMA), and a corticosteroid-all in one device. Trelegy Ellipta, for example, cuts exacerbations by 25% compared to dual therapy. And there’s growing interest in personalized treatment. FeNO testing-measuring nitric oxide in your breath-now helps doctors decide how much steroid you really need. High FeNO? You likely have allergic inflammation and need more steroid. Low FeNO? You might not need steroids at all.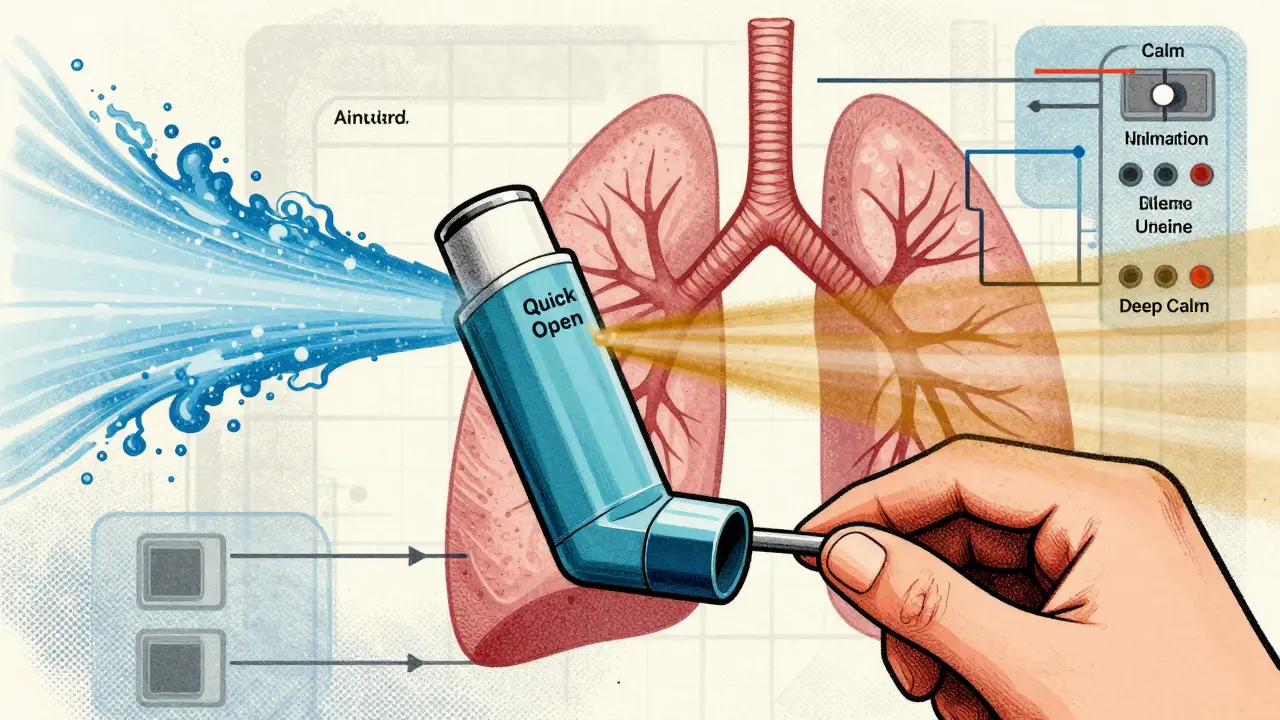
Getting It Right: Practical Tips
You don’t need to be a doctor to use these medications correctly. But you do need to be intentional.- Always use your rescue inhaler first. Wait five minutes. Then use your corticosteroid.
- Rinse and spit after every corticosteroid puff. Even if you don’t feel anything. It prevents thrush.
- Use a spacer if you’re on a metered-dose inhaler. Spacers improve delivery by 70%. They’re cheap, easy, and often free with your prescription.
- Don’t use long-acting bronchodilators alone. Always paired with a corticosteroid.
- Track your rescue inhaler use. If you’re going through more than one canister a month, talk to your doctor. You need better control.
What’s Not Working
Despite all the advances, big gaps remain. Only 31% of patients use inhalers correctly without training. That’s not because they’re careless. It’s because most people get a device and a pamphlet-and that’s it. Hospitals are starting to fix this. Johns Hopkins implemented standardized asthma action plans with visual guides and step-by-step videos. Result? Medication errors dropped by 47%. The future is in education-not just more drugs. The American Lung Association’s free Lung HelpLine (1-800-LUNGUSA) handles over 120,000 calls a year. Most are from people asking, “Which one do I use when?” You don’t need to memorize pharmacology. But you do need to know this: your blue inhaler is for emergencies. Your brown one is for daily prevention. And if you’re not using them in the right order, you’re not getting the full benefit.Final Thought
Respiratory medications aren’t magic pills. They’re tools. And like any tool, they only work if you use them the right way. Bronchodilators give you back your breath. Corticosteroids protect your lungs from long-term damage. Together, they don’t just manage symptoms-they change the course of your disease. If you’ve been using your inhalers the same way for years and still feel like you’re fighting for air, it’s not you. It’s the technique. Try the five-minute rule. Rinse your mouth. Use a spacer. And talk to your doctor-not just about what to take, but how to take it.Can I use a bronchodilator and corticosteroid at the same time?
Technically, yes-you can press both inhalers one after the other. But doing so without waiting reduces how much of the corticosteroid reaches your deep lungs. Always use the bronchodilator first, wait five minutes, then use the corticosteroid. This gives the steroid the best chance to work where it’s needed most.
Why does my inhaler make my heart race?
That’s likely your rescue inhaler-usually albuterol. It’s a beta-2 agonist, and while it targets the lungs, a small amount can enter your bloodstream and stimulate your heart. Shaking, fast heartbeat, and nervousness are common side effects. They’re usually mild and go away in 15 to 30 minutes. If they’re severe or last longer, talk to your doctor. You may need a different medication or lower dose.
Do corticosteroids weaken my immune system?
Inhaled corticosteroids are designed to act locally in your lungs. The amount that enters your bloodstream is very low-much less than oral steroids. They don’t significantly weaken your overall immune system. However, long-term use at high doses (over 1000 mcg of fluticasone daily) can slightly increase pneumonia risk in older COPD patients. That’s why doctors avoid high doses unless absolutely necessary.
Can I stop using my corticosteroid if I feel fine?
No. Corticosteroids work to prevent inflammation before it causes symptoms. If you stop taking them, inflammation returns quietly-often before you feel any breathing trouble. That’s why people think they don’t need it. But stopping leads to more flare-ups, hospital visits, and long-term lung damage. Always follow your doctor’s plan, even when you feel good.
What’s the difference between a rescue inhaler and a maintenance inhaler?
Rescue inhalers (like albuterol) are for quick relief during asthma attacks or sudden breathlessness. They work in minutes but last only a few hours. Maintenance inhalers (like fluticasone or budesonide) are for daily use to prevent inflammation and flare-ups. They don’t work right away but reduce your risk of attacks over time. One is emergency medicine. The other is preventive care.
Are combination inhalers better than using two separate ones?
For most people with persistent asthma or COPD, yes. Combination inhalers like Advair or Symbicort simplify your routine, improve adherence, and ensure you get both medications together. Studies show people are more likely to take one device correctly than two. They also reduce the chance of using a long-acting bronchodilator without a steroid-something that’s dangerous.
Do inhalers harm the environment?
Yes. Traditional metered-dose inhalers use propellants that are potent greenhouse gases. One albuterol inhaler has the same carbon footprint as driving 300 miles. Dry powder inhalers don’t use propellants and are much greener. Many new inhalers released since 2020 are dry powder types. Ask your doctor if you can switch to one-it’s better for your lungs and the planet.



Allie Lehto
January 24, 2026 AT 22:37Henry Jenkins
January 26, 2026 AT 13:28Renia Pyles
January 28, 2026 AT 01:45Nicholas Miter
January 28, 2026 AT 18:22Suresh Kumar Govindan
January 30, 2026 AT 17:51Ashley Karanja
January 31, 2026 AT 19:15Karen Droege
February 2, 2026 AT 19:14Shweta Deshpande
February 3, 2026 AT 22:08Jessica Knuteson
February 4, 2026 AT 00:44Ashley Porter
February 5, 2026 AT 00:01Peter Sharplin
February 5, 2026 AT 19:26Kipper Pickens
February 6, 2026 AT 02:53Joanna Domżalska
February 7, 2026 AT 06:56Josh josh
February 9, 2026 AT 05:29